Introduction. Cervical pregnancies occur when the fertilized egg implants in the wall of the cervix below the internal cervical os. The incidence is between 1 in 8600 and 1 in 12,400 pregnancies. The risk factors include previous instrumentation, cervical or uterine surgery, in vitro fertilization with embryo transfer, uterine anomalies, leiomyomas, synechiae, previous caesarean section, and pelvic inflammatory disease. Sonographic findings in cervical pregnancy may include an hourglass uterine shape, ballooned cervical canal, gestational tissue at the cervix, absence of intrauterine gestational tissue, and a portion of the endocervical canal between the gestation and the endometrial canal. The medical management includes the systemic administration of methotrexate, but failure is common in pregnancies over nine weeks with a crown-rump length (CRL) greater than 10 mm, presence of embryonic cardiac activity, and beta-human chorionic gonadotropin (β-HCG) levels higher than 10,000 mIU/ml. Materials and method. This paper represents a case report of a 34-year-old woman with a history of previous caesarean section and elective abortion, presenting with 8 weeks of amenorrhea. She was diagnosed one week prior with cervical ectopic pregnancy. Results. The ultrasound examination revealed the presence of a gestational sac with an embryo showing cardiac activity, located in the upper part of the cervix, below the uterine scar. The CRL measured 10 mm, corresponding to a gestational age of 7 weeks and 1 day. The uterine cavity displayed an endometrial thickness of 11 mm, and both ovaries appeared normal. With the patient’s informed consent, surgical evacuation was performed, using suction curettage, resulting in minimal bleeding. The cervical lacerations were sutured with transfixion sutures. The subsequent progress was favorable. Conclusions. While it is an extremely rare variety of ectopic pregnancy, cervical pregnancy represents a potential surgical emergency if not diagnosed in a timely manner. The possible complications include uterine rupture with subsequent hemorrhage, requiring hemostatic hysterectomy in such cases.
Cervical ectopic pregnancy – case report
Sarcina cervicală – prezentare de caz
First published: 27 noiembrie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.42.4.2023.8996
Abstract
Rezumat
Introducere. Sarcina ectopică cu localizare cervicală se datorează implantării ovocitului fertilizat în peretele colului uterin la un nivel inferior orificiului cervical intern. Incidenţa este între 1 la 8600 şi 1 la 12400 de sarcini. Factorii de risc includ chiuretajul uterin în antecedente, intervenţii chirurgicale cervicale sau uterine, fertilizare in vitro cu transfer de embrioni, anomalii uterine, leiomioame, sinechii, uterul cicatricial după operaţie cezariană sau boala inflamatorie pelviană. Constatările ecografice în sarcina cervicală pot include forma de clepsidră a uterului, canal cervical cu aspect de balon, sac gestaţional la nivelul colului uterin, absenţa sacului gestaţional intrauterin şi o porţiune liberă a canalului endocervical între sarcină şi canalul endometrial. Managementul medical include administrarea sistemică de metotrexat, dar eşecul este frecvent în sarcinile cervicale de peste 9 săptămâni cu o lungime craniocaudală (LCC) mai mare de 10 mm, prezenţa activităţii cardiace embrionare sau niveluri ale beta-gonadotropinei corionice umane (β-HCG) mai mari de 10000 UI/L. Materiale şi metodă. Acest articol reprezintă un studiu de caz al unei femei de 34 de ani cu uter cicatricial după operaţie cezariană şi chiuretaj uterin evacuator şi aspirativ electiv în antecedente, cu 8 săptămâni de amenoree. Pacienta a fost diagnosticată cu o săptămână înainte cu sarcină ectopică cervicală. Rezultate. Examenul ecografic a evidenţiat existenţa unui sac gestaţional cu embrion cu activitate cardiacă prezentă, situat în partea superioară a colului uterin, sub cicatricea uterină. LCC a măsurat 10 mm, corespunzătoare unei vârste gestaţionale de 7 săptămâni şi 1 zi. Cavitatea uterină prezenta o grosime a endometrului de 11 mm, iar ambele ovare aveau aspect ecografic normal. Cu consimţământul informat al pacientei, s-a realizat evacuarea sarcinii cervicale prin chiuretaj aspirativ, rezultând o sângerare minimă pe cale vaginală. Laceraţiile cervicale s-au suturat cu fire transfixiante. Evoluţia ulterioară a fost favorabilă. Concluzii. Deşi este un tip extrem de rar de sarcină ectopică, sarcina cervicală reprezintă o potenţială urgenţă chirurgicală dacă nu este diagnosticată în timp util. Complicaţiile posibile includ ruptura uterină cu hemoragie secundară, fiind necesară histerectomia de hemostază în astfel de cazuri.
Introduction
The definition of an ectopic pregnancy (EP) is that of a pregnancy where implantation occurs outside the endometrial cavity. Roughly 95% of EPs take place in the fallopian tube. Unusual locations include the cervix, a rudimentary horn, and myometrial scars resulting from procedures like caesarean delivery or myomectomy. Other atypical forms of EP include intraovarian, abdominal, retroperitoneal and mediastinal pregnancies, along with heterotopic pregnancies (where both ectopic and intrauterine gestations coexist). Reports even suggest ectopic pregnancies occurring after supracervical hysterectomy and total abdominal hysterectomy, though these are exceedingly rare.
Cervical ectopic pregnancies represent a unique scenario in which the fertilized egg implants directly into the wall of the cervix, specifically below the level of the internal cervical os. This condition is characterized by the embryo establishing itself in the cervical region rather than the typical location within the endometrial cavity. Various factors elevate the risk of cervical EP. These encompass a history of previous instrumentation, such as medical procedures involving the cervix or uterus, cervical or uterine surgery, past experiences with abortion or curettage, involvement of in vitro fertilization with embryo transfer (IVF-ET), the presence of uterine anomalies, the existence of leiomyomas (commonly known as uterine fibroids), synechiae (adhesions), Asherman syndrome (characterized by intrauterine adhesions), a history of caesarean delivery, intrauterine device (IUD) placement, and a background of pelvic inflammatory disease (PID). Understanding and identifying these risk factors are crucial for both the diagnosis and the management of cervical ectopic pregnancies(1).
Materials and method
This paper represents a case report of a 34-year-old woman, non-smoker, with normal Body Mass Index (BMI), with a history of previous caesarean section (eleven years earlier) and one elective abortion, presenting with eight weeks of amenorrhea, nausea and vomiting. Her medical record included secondary anemia and appendectomy. Her family medical history consists of one case of paternal malignant melanoma. She was diagnosed one week prior with cervical EP on transvaginal ultrasound examination.
Results
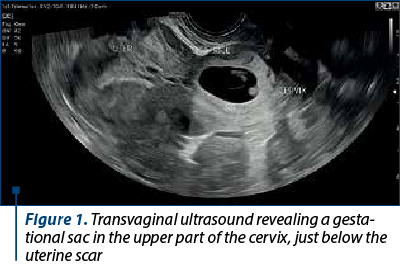
Transvaginal ultrasound examination revealed the presence of a gestational sac located in the upper part of the cervix, below the uterine scar, containing an embryo with cardiac activity. The CRL measured 10 mm, corresponding to a gestational age of 7 weeks and 1 day. The uterine cavity displayed an endometrial thickness of 11 mm, and both ovaries appeared normal (Figure 1).
The gestational sac was revealed as an eccentric location, intricately embedded in the cervix’s wall as trophoblastic tissue infiltrates through the cervical mucosa. This invasion typically occurs through a defect created by prior instrumentation or injury. The diagnostic clarity is heightened in transverse images, facilitating the recognition that the gestational sac (GS) is situated within the cervix’s wall, distinctly separated from the endocervical canal, which exhibits displacement due to the sac’s presence. A comprehensive ultrasound examination is imperative, targeting both the external and internal ostia. The incorporation of 3D ultrasound further enhances precision in delineating the pregnancy’s exact location (Figure 2).

The gestational sac itself presents as an oval structure, enveloped by a thick, well-formed echogenic rim. Color Doppler ultrasound imaging reveals vascularity within the gestational sac’s wall, accompanied by feeding vessels extending from the cervix’s wall to the sac.
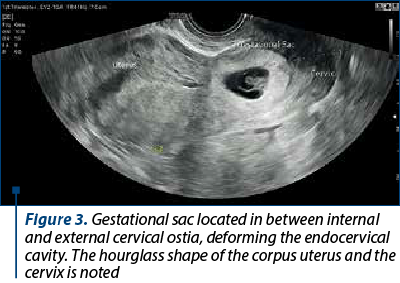
In the later stages of pregnancy, the cervix undergoes noticeable changes, exhibiting enlargement, a bulbous appearance, and heightened vascularity upon inspection. Ultrasound imaging captures this transformation, depicting a uterus with an hourglass shape. This configuration is characterized by the uterine corpus and a disproportionately enlarged cervix, forming a discernible “waist” at the level of the internal os (Figure 3). It is noteworthy that, in contemporary clinical practice, diagnosing cervical ectopic pregnancies at such an advanced stage is uncommon, as most cases are identified early in the first trimester. Early detection and comprehensive imaging play pivotal roles in understanding and managing cervical ectopic pregnancies.
Distinguishing between a cervical pregnancy and an impending or inevitable miscarriage presents a diagnostic challenge, particularly when observing the evacuation of the gestational sac passing through the endocervical canal. In instances of an impending miscarriage, the gestational sac is typically centrally located within the endocervical canal. The surrounding cervical stroma exhibits a symmetrical thickness, a characteristic that is best discerned on transverse images. The gestational sac in miscarriages may present with an irregular, flattened or crenated border and lacks the surrounding vascularity seen in cervical ectopic pregnancies.
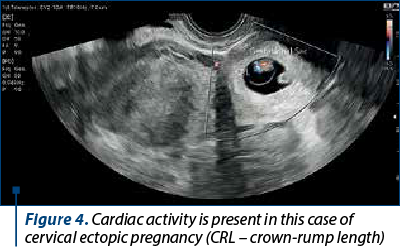
While the presence of trophoblastic blood flow or embryonic cardiac activity can increase the likelihood of a gestational sac in the cervix being a cervical ectopic pregnancy, these features can also be observed in aborting intrauterine pregnancies (Figure 4). The sliding sign helps in the differential diagnosis and involves applying gentle pressure to the cervix with a transvaginal transducer. In cases of an aborting gestational sac, it will exhibit a sliding movement up and down in the endocervical canal. Contrary, such movement will not occur with an implanted cervical ectopic pregnancy(1).
This nuanced diagnostic approach becomes imperative in clinical settings where a precise differentiation between these conditions is essential for making informed and effective management decisions. It underscores the importance of comprehensive imaging and careful consideration of dynamic signs to ensure accurate diagnosis and appropriate intervention, particularly given the potential implications for the patient’s health and fertility.
In cases where patients are hemodynamically stable, the evacuation of the pregnancy can be considered as a treatment method. Historically, the standard treatment for cervical pregnancy involved uterine curettage coupled with strategies aimed at mitigating bleeding. However, the risk of significant hemorrhages necessitating hysterectomy is higher with this approach. Therefore, this therapeutic method should be reserved for situations where other treatment options are not feasible.
Before the procedure, the physician may opt for preoperative measures such as ligating the cervical arteries or embolizing the uterine arteries to enhance the control of bleeding. Postoperatively, the insertion of a catheter with a balloon into the cervix is recommended as a local tamponade method. If hemostasis cannot be achieved through local tamponade, a necessity hysterectomy must be performed.
Hysterectomy may be chosen as a treatment method in specific scenarios, including cases involving hemodynamically unstable patients or situations where individuals have completed their family planning. The selection of the appropriate treatment strategy requires careful consideration of the patient’s overall health, reproductive goals, and the specific clinical circumstances.
Medical treatment should be indicated for uncomplicated forms of tubal and cervical ectopic pregnancies when several criteria are met simultaneously. These include a hemodynamically stable patient, compliance with post-therapeutic monitoring, the patient’s desire to preserve fertility, the absence of contraindications for taking methotrexate, serum b-HCG levels between 1500 mIU/mL and 5000 mIU/mL, adnexal mass size below 3.5 cm, and the absence of embryonic cardiac activity at transvaginal echography. Notably, the presence of embryonic cardiac activity is associated with a decreased chance of success with medical treatment, the studies indicating a higher failure rate for baseline b-HCG levels above 5000 mIU/ml.
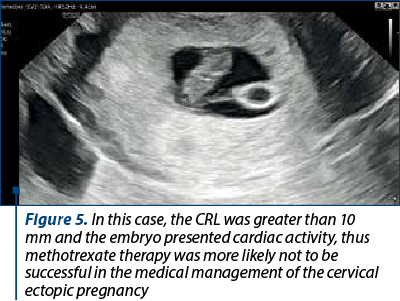
The physician must adhere to contraindications for methotrexate administration, which include absolute contraindications such as heterotopic pregnancy if the patient wishes to continue the intrauterine pregnancy, hemodynamic instability, and ruptured ectopic site. Relative contraindications encompass serum b-HCG levels above 5000 mIU/ml, adnexal mass exceeding 3.5 cm, and the presence of embryonic cardiac activity. Specific contraindications to methotrexate administration must also be respected. Failure of systemic methotrexate administration is common in pregnancies over 9 weeks with a crown-rump length (CRL) greater than 10 mm, presence of embryonic cardiac activity, and beta-human chorionic gonadotropin levels higher than 10,000 mIU/ml (Figure 5)(2).
The medical treatment should be limited to compliant patients defined by adherence to criteria such as alcohol abstinence, avoidance of vitamins with folinic acid until the resorption of the ectopic pregnancy, prohibition of nonsteroidal anti-inflammatory drugs, maintenance of sufficient hydration, and the use of effective contraception for at least three months. Effective contraception must be followed due to the possible teratogenic risk.
The physician must obtain the informed consent from patients who partially meet the eligibility criteria, informing them about the vital risks, the possibility of subsequent surgical or ambulatory medical treatment, the need for strict monitoring to detect the warning signs, and the adverse effects following treatment.
The choice of the methotrexate protocol should be guided by baseline serum b-HCG levels, with the physician informing the patient about the risks and benefits of each medical protocol. The options include a single-dose, two-dose or multiple-dose regimen, with the single-dose protocol suitable for patients with relatively low or plateaued baseline b-HCG levels. The two-dose protocol may be recommended for patients with higher baseline b-HCG levels as an alternative to the multiple-dose protocol to reduce adverse effects.
The multiple-dose regimen may be indicated when the pregnancy is cornual or cervical, fetal heart activity is present, or b-HCG levels exceed 3500 mIU/ml. In the case of ectopic pregnancy, the physician can administer intraovular local methotrexate or a potassium chloride solution(3).
In this case, upon obtaining the informed consent of the patient, a carefully planned and executed surgical evacuation was performed, using the method of suction curettage. This approach, known for its efficacy and minimal bleeding, was chosen to ensure a comprehensive and thorough removal of any residual tissue. During the procedure, special attention was given to addressing cervical lacerations, and meticulous suturing with transfixion sutures was carried out to promote optimal healing and reduce the risk of complications.
Following the surgical intervention, ongoing monitoring and assessment were conducted to track the patient’s progress. The favorable outcome reported post-surgery underscores the effectiveness of the chosen approach and the attentiveness to detail in managing the procedure. This comprehensive care, from the initial informed consent to the meticulous surgical techniques employed, reflects a commitment to the patient’s well-being and underscores the importance of a thorough and thoughtful approach in medical interventions.
Discussion
In a comprehensive review conducted in 2022, which synthesized findings from multiple studies spanning the period from 2000 to 2022, the treatment landscape for cervical ectopic pregnancies was thoroughly examined. Notably, the focus of the review was on alternative fertility-sparing treatments. Among these, transvaginal ultrasound-guided local injections of absolute ethanol and the concomitant use of systemic methotrexate alongside intraamniotic potassium chloride emerged as notably effective approaches in terminating the pregnancy. Importantly, the efficiency of these treatments was such that no additional interventions were deemed necessary. It’s noteworthy, however, to acknowledge the limitation of the studies included in this review. The pool of studies specifically addressing these alternative treatments for cervical ectopic pregnancies was relatively small, with only two patients in the first study, respectively one patient in the latter. While the findings are promising and suggest the efficacy of these approaches, the limited sample size emphasizes the need for further research and larger-scale studies to validate these conclusions and ensure broader applicability(4).
In a case series report conducted in Italy spanning the period between 2014 and 2019, the efficacy of hysteroscopy in the fertility-sparing treatment of cervical ectopic pregnancies was investigated. The study involved the analysis of five reported cases and, notably, none of these cases needed suction or curettage procedures either before or after the hysteroscopic detachment of the pregnancy. Within this series, there was a noteworthy incident in which a hysteroscopic procedure was interrupted before the complete resection of the pregnancy. This interruption was prompted by a profuse hemorrhage, resulting in a substantial blood loss, necessitating a blood transfusion. Following this incident, a second hysteroscopy was performed on the subsequent day, with the specific aim of achieving complete resection of the cervical pregnancy. Importantly, uterine artery embolization was not employed in this case to preempt hemorrhage and facilitate hemostasis. Following the hysteroscopic procedures, no complications, such as vaginal bleeding, were recorded. The completion of the hysteroscopic management, involving the complete resection of the cervical pregnancy and coagulation of vessels at the implantation site, marked a critical point in the treatment process. Subsequent monitoring revealed a faster decrease in serum b-HCG levels from the day after the procedure. Notably, the b-HCG levels became undetectable within a range of 15 to 40 days after the hysteroscopic management. It’s worth mentioning that, among the cases studied, the patient who exclusively received medical treatment had an undetectable serum b-HCG level within 35 days. However, transvaginal ultrasound findings revealed the presence of a persistent vascularized lesion at the implantation site after five months. This underscores the importance of considering not only the serum b-HCG levels, but also imaging findings for a comprehensive assessment of the effectiveness of fertility-sparing treatments for cervical ectopic pregnancies(5).
In a case report from 2021, a 31-year-old woman, initially diagnosed with early miscarriage due to six weeks of amenorrhea and an initial b-HCG value of 72 mIU/ml, was later correctly diagnosed with cervical ectopic pregnancy through reevaluation with ultrasonography. The embryo exhibited a CRL of 8 mm and no visible cardiac activity. Consequently, systemic methotrexate was administered, and four days later, intraamniotic methotrexate was injected due to persistently high b-HCG values and consistent ultrasound images. The subsequent clinical course became complicated by worsening vaginal bleeding on the 12th day of hospitalization. In response, selective embolization of the left cervical branch was undertaken, followed by curettage under general anesthesia the next day. Fortunately, the patient’s clinical evolution was favorable, leading to discharge the following day. Post-discharge follow-up involved weekly monitoring of b-HCG levels, which became negative on the fourth week after discharge (49 days after diagnosis). Transvaginal ultrasound assessments during the first- and second-week post-discharge revealed a nodular and cavitated image measuring 18x13 mm at the cervical level, with mild peripheral vascularization, suggesting residual trophoblastic tissue in the process of resorption. By the third week, the ultrasound returned completely to normal. As of the latest update, the patient was reported to be clinically well and initiated oral contraception(6).
In another notable case study from 2022, a cervical ectopic pregnancy complicated by a ruptured posterior cervical lip, initially misdiagnosed as an 11-week incomplete abortion, adds to the spectrum of unique clinical presentations. The patient, with no medical history of vaginal instrumentation, was initially scheduled for manual vacuum aspiration. However, during pelvic examination under sedation, a significant 4-cm defect was identified in the posterior cervical lip, with a protruding cystic mass through the defect. Transvaginal ultrasonography confirmed the diagnosis. After obtaining the informed consent, which included the possibility of hemostatic hysterectomy, the patient was taken to the operating room. Under general anesthesia, the gestational sac was delivered through the posterior cervical rupture, after the instillation of diluted vasopressin into the cervix. The cervical defect was meticulously repaired using continuous sutures with Vicryl number 1. The subsequent examination of the uterine cavity by manual vacuum aspiration revealed no significant aspirate. To maintain the cervical canal, a size 8 Foley catheter was introduced into the uterus and retained for one week. The patient experienced an uneventful postoperative period, with a vaginal examination indicating a serous discharge in the posterior fornix and a well-healing wound on the posterior cervical lip. The intrauterine Foley catheter was subsequently removed, and the patient was scheduled for a two-week follow-up at the outpatient clinic. However, she missed the appointment and, despite several attempts to contact her by telephone, she remained unreachable. This case underscores the importance of careful clinical evaluation and the need for timely and thorough follow-up in managing complex cases of cervical ectopic pregnancies(7).
In a groundbreaking case report from 2023, a live birth was achieved through uterus-conserving management in a cervical ectopic pregnancy, marking a significant advancement in clinical outcomes. The patient, a 37-year-old woman in her third pregnancy with two previous caesarean sections, presented at 7+3 weeks of pregnancy with a cervical ectopic pregnancy. Following a comprehensive discussion about the associated risks, including the potential for severe bleeding and the possibility hysterectomy at any stage of pregnancy, the patient made the decision not to terminate the pregnancy. This choice was motivated by ethical considerations that were significant to her. At the 12th week of pregnancy, a cerclage procedure was performed to prevent cervical distention caused by the expanding placenta. Given the lack of experience in managing cervical EP and to avoid emergency procedures, a caesarean section was recommended at the 30th week of pregnancy, due to unspecific pain reported by the patient. Importantly, there was no occurrence of vaginal bleeding throughout the pregnancy. During transverse laparotomy, the urinary bladder was sharply dissected from the anterior uterine and cervical wall. The baby was delivered through a transverse cervicotomy caudally of the placenta, and the placenta was intentionally left in situ. Following the delivery, the patient underwent prophylactic embolization of the uterine arteries to prevent severe hemorrhage. Forty-eight hours later, ultrasound examination revealed a floating, avascular placenta within a poorly echogenic fluid-filled cervical space, along with macrohematuria. Subsequent re-laparotomy and cervicotomy on the same day allowed for the complete and easy evacuation of the placenta. A recognized bladder injury was promptly closed, and a cervical internal os plasty was performed by inverting the cervical lips and suturing their distal ends to the proximal cervical tissue, resulting in complete cessation of bleeding. Despite receiving eight erythrocyte concentrates, the patient remained in a stable condition without experiencing hemorrhagic shock throughout the course of treatment. This case represents a pioneering achievement in achieving a live birth while conserving the uterus in the context of cervical ectopic pregnancy(8).
Conclusions
Cervical pregnancy, an exceedingly rare variant of ectopic pregnancy, demands vigilant attention due to its potential to escalate into a surgical emergency if not identified promptly. The stakes involve complications like uterine rupture, a grave scenario that could lead to substantial hemorrhage. In such critical instances, the intervention of hemostatic hysterectomy becomes imperative, if a timely diagnosis has not been established.
Contemporary medical strategies have evolved to embrace fertility-preserving therapies that offer alternatives to more radical interventions. Among these, the use of methotrexate, either systemically or through intraamniotic injection or intraamniotic injection of potassium chloride, has emerged as a viable option in certain conditions. Additionally, interventions such as curettage and hysteroscopy have been incorporated into the arsenal of treatments. These procedures are accompanied by a spectrum of pre- and postoperative techniques carefully designed to mitigate the risk of hemorrhagic complications.
This modern approach marks a paradigm shift in the management of cervical pregnancies, providing effective alternatives to the historical reliance on hemostatic hysterectomy. By prioritizing fertility preservation and employing nuanced interventions, contemporary medical practices aim to not only address the immediate complications associated with cervical pregnancies, but also uphold the reproductive potential and the overall well-being of the patient.
Conflict of interest: none declared.
financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.

Bibliografie
-
Baltarowich OH, Scoutt LM. Ectopic Pregnancy. In: Callen P, Norton M, Scoutt L. Callen’s ultrasonography in obstetrics and gynecology. 6th Ed.: Elsevier, 2017;966-1000.
-
Hoffman BL, Schorge JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM. Ectopic Pregnancy. In: Williams Gynecology. 3rd ed, McGraw-Hill Education, 2016;161-76.
-
Balint O, Pirtea L. Sarcina ectopică. Ghid clinic. 2019. https://sogr.ro/wp-content/uploads/2019/06/26.-Sarcina-ectopic%C4%83.pdf
-
Leziak M, Żak K, Frankowska K, et al. Future perspectives of ectopic pregnancy treatment - review of possible pharmacological methods. Int J Environ Res Public Health. 2022;19(21):14230.
-
Stabile G, Mangino FP, Romano F, et al. Ectopic cervical pregnancy: treatment route. Medicina. 2020;56(6):293.
-
Évora F, Hundarova K, Águas F, Carvalho G. Cervical ectopic pregnancy: a multidisciplinary approach. Cureus. 2021;13(10):e19113.
-
Elachi FA, Egwuda K, Egbodo CO, Olubiyi DO. Cervical ectopic pregnancy presenting with ruptured posterior cervical lip: a case report. Cureus. 2022;14(8):e28508.
-
Köninger A, Nguyen BP, Schwenk U, et al. Cervical ectopic pregnancy - the first case of live birth and uterus-conserving management. BMC Pregnancy Childbirth. 2023;23(1):664.
Articole din ediţiile anterioare
Tumoră uterină asemănătoare tumorilor de cordoane sexuale ovariene: o diagnosticăm dacă o cunoaştem. Prezentare de caz şi review al literaturii
Tumora uterină asemănătoare tumorilor de cordoane sexuale ovariene (UTROSCT) reprezintă un tip rar de neoplasm uterin, având un potenţial malign in...