Uterine tumor resembling ovarian sex cord tumor (UTROSCT) represents a rare uterine neoplasm with uncertain malignant potential. Several reports have described recurrences, metastases and even deaths associated with these generally considered benign tumors, thus making them a controversial disease entity. UTROSCT has an unclear histogenesis and it possesses a polyphenotypic immunophenotype. We present a case of UTROSCT in a patient accusing abnormal genital bleeding and symptoms associated with anemia. After performing a total abdominal hysterectomy with bilateral salpingectomy, the final pathology report revealed UTROSCT with no sarcomatous features. The patient is still disease-free after 30 months of follow-up. We also present the data available in literature regarding this relative new type of uterine tumor. We are of the opinion that a high index of suspicion is of paramount importance when examining a patient with an uterine mass in order to promptly identify the risk factors that may predict agressive tumor behaviour.
Tumoră uterină asemănătoare tumorilor de cordoane sexuale ovariene: o diagnosticăm dacă o cunoaştem. Prezentare de caz şi review al literaturii
Uterine tumor resembling ovarian sex cord tumor: we can diagnose it if we consider it. Case report and literature review
First published: 24 martie 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.35.1.2022.6132
Abstract
Rezumat
Tumora uterină asemănătoare tumorilor de cordoane sexuale ovariene (UTROSCT) reprezintă un tip rar de neoplasm uterin, având un potenţial malign incert. Mai multe studii au raportat recurenţe, metastaze şi chiar decese asociate cu aceste tumori generic considerate benigne, ceea ce le încadrează totuşi într-o tipologie controversată. UTROSCT prezintă un model de histogeneză încă neclar şi un poliimunofenotip. În această lucrare, aducem în discuţie cazul unei paciente care s-a prezentat în clinica noastră acuzând modificări ale ciclului menstrual şi simptome asociate anemiei. În urma investigaţiilor clinice şi paraclinice, s-a decis practicarea histerectomiei totale cu salpingectomie bilaterală pentru o formaţiune tumorală intracavitară, diagnosticul anatomopatologic fiind UTROSCT fără modificări sarcomatoase. Pacienta prezintă în continuare o evoluţie favorabilă la 30 de luni postoperatoriu. De asemenea, am efectuat un review al literaturii de specialitate referitoare la acest tip relativ nou de tumoră. Opinăm că este deosebit de important un indice ridicat de suspiciune în cazul pacientelor diagnosticate cu tumori uterine pentru a putea identifica factorii de risc potenţial predictivi pentru evoluţia agresivă a acestora.
Introduction
Uterine tumor resembling ovarian sex cord tumor (UTROSCT) represents a rare distinct neoplasm included in the current World Health Organization (WHO) classification of endometrial stromat tumors(1) and its clinical characteristics are not fully understood. It was first described by Clement and Scully in 1976(2).
These neoplasms resemble morphologically sex cord tumors of the ovary and have a polyphenotypic immunophenotype. Their molecular pathogenesis has not been clearly described yet; however, tumors lack alterations found in other uterine tumors bearing sex cord-like differentiation, such as endometrial stromal sarcoma(3).
UTROSCTs usually occur in middle-aged women and behave as tumors of low malignant potential. The clinical characteristics are abnormal uterine bleeding, abdominal pain associated with an enlarged uterus or a palpable uterine mass without specific imaging aspects(4). Most of the times, the diagnosis is incidental, following immunohistochemical and ultrastructural studies on the surgical specimen(5).
The treatment options include hysterectomy with or without bilateral salpingo-oophorectomy or even the hysteroscopic resection of the tumor(6); yet, the management, prognosis, morbidity and mortality of this rare pathology are still under current debate.
In this paper, we present the case of a 32-year-old patient with abnormal uterine bleeding who was finally diagnosed with UTROSCT. Her treatment and follow-up after diagnosis are discussed and the data published regarding this entity are reviewed.
Case report
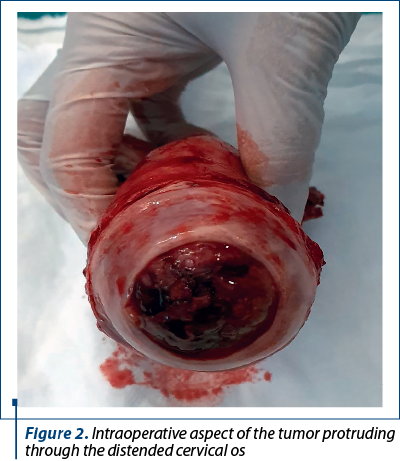
A 32-year-old gesta 3 para 1 Caucasian woman attended a local hospital accusing a six-month history of abnormal genital bleeding and symptoms associated with anemia. She had no prior history of allergy, comorbidities, use of medication or surgery, and there was no family history of gynecological cancer. The clinical gynecologic examination showed a large, bleeding mass protruding through the cervical os, and the initial pelvic ultrasound examination revealed an uterine hypoechogenic mass with vascularization at power Doppler (RI 0.67) with a diameter of 6/2.5 cm (Figure 1, bottom right). Interestingly, the endometrial sampling revealed a normal microscopic appearance. The patient was referred to our hospital for further investigation; after imaging and diagnostic workup and taking into account that the patient had completed the family planning, we decided to perform a total abdominal hysterectomy with bilateral salpingectomy. At gross pathologic examination, the intracavitary lesion appeared yellow, polycyclic, with a soft consistency and being poorly delineated with respect to the surrounding myometrium (Figures 1 and 2).
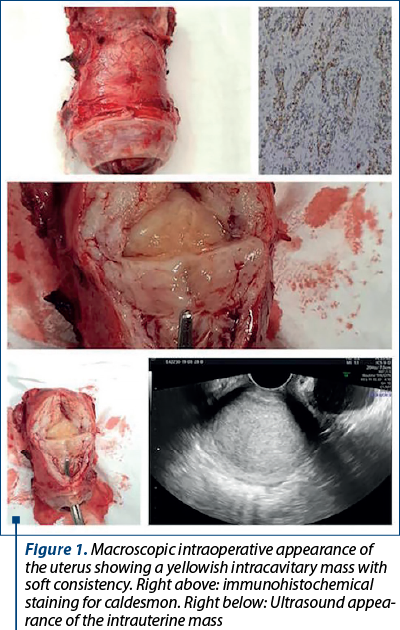
On microscopic examination, the tumor was composed of elements similar to the sex cord cells with a trabecular and alveolar arhitectural pattern and tubular elements. The cells showed an epithelioid appearance with irregular nuclei and abundant cytoplasm, fine chromatin and a high nucleoplasm ratio. These findings were consistent with UTROSCT. Immunohistochemical staining showed that the tumor cells were positive for Ki67, WT1, ER CD99, caldesmon and calretinin (Figure 1, above right). Both of the tubes were histologically normal.
At the regular checkups, the patient remained asymptomatic with normal pelvic examination and ultrasound findings up until the present time, at 30 months after surgery.
The patient has consented to the submission of the case report to the journal.
Discussion
To date, less than 100 cases of UTROSCT have been reported in literature(7). The average age at diagnosis is 50.6 years old and the median age is 51 years old, while the tumor size is, on average, 47.6 mm(8), the latter being consistent with the one in our case report.
The clinical diagnosis of UTROSCT is challenging as the symptoms vary among patients and are not typical in most of the cases, therefore being misleading. The common symptoms consist in abnormal uterine bleeding, including postmenopausal bleeding (33.9%)(8) and pelvic pain. Dimitriadis et al. reported ectopic hyperprolactinaemia due to a malignant UTROSCT in a patient with a normal cranial MRI and in whom the prolactin rose further with dopamine agonist treatment(9).
The diagnosis can only be confirmed by histology after tumor resection, in most cases incidentally following hysterectomy performed due to an uterine mass (endometrial polyp or fibroid)(10). Until now, there have not become available any noninvasive diagnostic tests such as specific serum markers or imaging findings. As a type of rare uterine tumor, UTROSCT can be diagnosed based on morphological and immunohistochemical conditions. Recently, UTROSCTs were found to be defined by recurrent fusions involving NCOA2 (nuclear receptor coactivator 2) or NCOA3, a finding that is directly amenable to diagnostic evaluation(3).
The standardized treatment for UTROSCT is lacking, due to its rarity, at present surgery being the preferred therapeutic method. It includes total hysterectomy with or without bilateral salpingo-oophorectomy or mass resection alone. Fertility sparing surgery should be offered to patients who wish to preserve their fertility; however, radical surgery must be considered after childbirth(1). The youngest patient with UTROSCT reported so far is a 22-year-old nulligravida who underwent a hysteroscopic resection of an intrauterine mass presumed as grade I submucous myoma and was free of disease after 20 months, without any adjuvant therapy(6). In our case, the patient opted for radical surgery as she completed childbearing.
Having an uncertain malignant potential and relapse, the patients diagnosed with UTROSCT should be followed-up closely. Tumor metastasis can occur to the ovary, omentum(11), lymph nodes and epiploic appendix(12), lungs(13) and vaginal vault(5). In 2016, Endo et al. reported UTROSCT pelvic lymph node recurrence in a 62-year-old woman, 23 years after hysterectomy(14).
Moreover, there has been described the death of a 49-year-old woman from a metastatic UTROSCT initially considered as metastatic epithelial ovarian cancer(15).
Conclusions
UTROSCT are generally considered benign tumors with a favorable progosis, but they can easily relapse through incomplete resection. Surgery remains the primary management therapy and fertility preservation in patients of childbearing age is a vital consideration. It is crucial for pathologists to recognize this rare entity, as the clinical findings are nonspecific. Close follow-up is required for all patients due to the lack of prognostic biomarkers.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Carbone MV, Cavaliere AF, Fedele C, et al. Uterine tumor resembling ovarian sex-cord tumor: Conservative surgery with successful delivery and case series. Eur J Obstet Gynecol Reprod Biol. 2021;256:326-32.
- Clement PB, Scully RE. Uterine tumors resembling ovarian sex-cord tumors. A clinicopathologic analysis of fourteen cases. Am J Clin Pathol. 1976;66(3):512-25.
- Dickson BC, Childs TJ, Colgan TJ, et al. Uterine tumor resembling ovarian sex cord tumor: a distinct entity characterized by recurrent NCOAS2/3 gene fusions. Am J Surg Pathol. 2019;43(2):178-86.
- Giordano G, Lombardi M, Brigati F, Mancini C, Silini EM. Clinicopathologic features of 2 new cases of uterine tumors resembling ovarian sex cord tumors. Int J Gynecol Pathol. 2010;29(5):459-67.
- Marrucci O, Nicoletti P, Mauriello A, et al. Uterine tumor resembling ovarian sex cord tumors type II with vaginal vault recurrence. Case Rep Obstet Gynecol. 2019;5231219.
- Watrowski R, Jäger C, Möckel J, Kurz P, Schmidt D, Freudenberg N. Hysteroscopic treatment of uterine tumor resembling ovarian sex cord-like tumor (UTROSCT). Gynecol Endocrinol. 2015;31(11):856-9.
- Schraag SM, Caduff R, Dedes KJ, Fink D, Schmidt AM. Uterine tumors resembling ovarian sex cord tumors- treatment, recurrence, pregnancy and brief review. Gynecol Oncol Rep. 2017;19:53-6.
- Zhou FF, He YT, Li Y, Zhang M, Chen FH. Uterine tumor resembling an ovarian sex cord tumor: a case report and review of literature. World J Clin Cases. 2021;9(23):6907-15.
- Dimitriadis KG, Wajman DS, Bidmead J, et al. Ectopic hyperprolactinaemia due to a malignant uterine tumor resembling ovarian sex cord tumors (UTROSCT). Pituitary. 2020;23(6):641-7.
- Garcia FAR, Gaigher VP, Ferreira RN, Filho AC. Uterine tumor resembling ovarian sex-cord tumors initially diagnosed as a prolapsed fibroid. Case Rep Obstet Gynecol. 2018;4703521.
- Kantelip B, Cloup N, Dechelotte P. Uterine tumor resembling ovarian sex cord tumors: report of a case with ultrastructural study. Hum Pathol. 1986;17(1):91-4.
- Umeda S, Tateno M, Miyagi E. Uterine tumor resembling ovarian sex cord tumors (UTROSCT) with metastasis: clinicopathological study of two cases. Int J Clin Exp Pathol. 2014;7(3):1051-9.
- Kondo Y, Sakaguchi S, Mikubo M, et al. Lung metastases of a uterine tumor resembling ovarian sex-cord tumor: report of a rare case. Diagn Cytopathol. 2018;46(1):88-91.
- Endo D, Todo Y, Okamoto K. A case of recurrent group II uterine tumor resembling ovarian sex-cord tumors, against which two hormonal agents were ineffective. Taiwan J Obstet Gynecol. 2016;55(5):751-3.
- Kuznicki ML, Robertson SE, Hakam A, Shahzad MM. Metastatic uterine tumor resembling ovarian sex cord tumor: a case report and review of the literature. Gynecol Oncol Rep. 2017;22:64-8.
Articole din ediţiile anterioare
Imagistica şi maparea chirurgicală în endometrioză
Endometrioza este o boală cronică estrogen-dependentă, cu potenţial inflamator, caracterizată prin prezenţa ţesutului ectopic endometrial în afa...
Dificultăţi de examinare ecografică la gravidele supraponderale. Studiu retrospectiv şi analiza literaturii
Introducere. În ultimele decenii, sistemul medical se confruntă tot mai des cu paciente obeze sau supraponderale. Obezitatea este asociată cu un ri...
Extinderea examinării standard a sistemului nervos central fetal la ecografia de trimestrele doi şi trei
Protocolul de bază asigură diagnosticarea majorităţii anomaliilor sau cel puţin sesizarea prezenţei unei anormalităţi şi direcţionarea cazului ...
A rare case of complete hydatidiform mole with prolonged evolution – clinical case
Mola hidatiformă, cunoscută drept sarcină molară, reprezintă o boală gestaţională trofoblastică cu punct de plecare placentar şi capacitate de meta...