Endometriosis is a chronic estrogen-dependent disease with inflammatory potential, characterized by the presence of ectopic endometrial tissue outside the uterus, with polymorphic and multifocal characteristics. In the same patient, there may be present several types of endometriotic lesions – from superficial endometriosis to endometriomas and deep infiltrative endometriosis. We can even say that it is a fibrotic condition in which the stroma and the endometrial epithelium are identified. Materials and method. We conducted a retrospective study, between 2017 and 2021, on a group of 126 patients, aged between 25 and 50 years old, operated in the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology, Bucharest, the Euroclinic Hospital – Private Health Network, and Monza Hospital, Bucharest. Results. We performed a comparative study of the diagnosis of ultrasound endometriosis/MRI and intraoperative endometriosis. According to information, the MRI diagnosis of endometriosis lesions is clearly superior, having a higher accuracy compared to the ultrasound diagnosis. Conclusions. There is no imaging method that can be used individually and be effective enough to identify the location and extent of endometriosis. The performance of these imaging procedures should be considered depending on the type of suspected endometriosis, the proposed therapeutic strategy, and the information to be provided to the patient. Transvaginal ultrasound is a repeatable, costless procedure that can be used to diagnose certain types and locations of endometriosis. The role of transvaginal ultrasound is to guide the type of subsequent complementary investigations depending on the location of the lesions, when suspected.
Imagistica şi maparea chirurgicală în endometrioză
Imaging and surgical mapping in endometriosis
First published: 15 aprilie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.32.2.2021.4998
Abstract
Rezumat
Endometrioza este o boală cronică estrogen-dependentă, cu potenţial inflamator, caracterizată prin prezenţa ţesutului ectopic endometrial în afara uterului, cu caracter polimorf şi multifocal, la aceeaşi pacientă putând fi prezente mai multe tipuri de leziuni endometriozice – de la endometrioza superficială la endometrioame şi endometrioză profund infiltrativă. Putem spune chiar că este o afecţiune fibrotică în care se pot identifica stroma şi epiteliul endometrial. Materiale şi metodă. Am realizat un studiu retrospectiv, între 2017 şi 2021, pe un grup de 126 de paciente, cu vârste cuprinse între 25 şi 50 de ani, operate în Spitalul Clinic de Obstetrică-Ginecologie „Prof. Dr. Panait Sîrbu”, Spitalul Euroclinic – Reţeaua privată de sănătate şi Spitalul Monza, Bucureşti. Rezultate. Am efectuat un studiu comparativ al diagnosticului de endometrioză pus ecografic/pe baza IRM şi al endometriozei intraoperatorii. Conform datelor, diagnosticul IRM al leziunilor endometriozei este net superior, având o precizie mai mare comparativ cu diagnosticul ecografic. Concluzii. Nu există o metodă imagistică utilizată individual care poate fi îndeajuns de eficientă pentru a identifica localizarea şi amploarea endometriozei. Efectuarea acestor proceduri imagistice ar trebui luată în considerare în funcţie de tipul de endometrioză suspectată, de strategia terapeutică propusă şi de informaţiile care trebuie furnizate pacientei. Ecografia transvaginală este o procedură repetabilă, necostisitoare, care poate fi utilizată pentru a diagnostica anumite tipuri şi localizări de endometrioză. Rolul ecografiei transvaginale este de a ghida tipul de investigaţii complementare ulterioare în funcţie de localizarea leziunilor, atunci când sunt suspectate.
Introduction
Endometriosis is a chronic, estrogen-dependent disease with inflammatory potential, characterized by the presence of endometrial ectopic tissue outside the uterus, with polymorphic and multifocal characteristics. In the same patient, there may be present several types of endometriotic lesions – from superficial endometriosis to endometriomas and deeply infiltrative endometriosis(1,2,3). We can even say that it is a fibrotic condition in which the stroma and the endometrial epithelium can be identified(4).
Therefore, the most important aspect in the diagnosis of deeply infiltrative endometriosis is the accuracy of the preoperative imaging – ultrasound and/or MRI diagnosis performed by an experienced clinician and radiologist.
Transvaginal ultrasound has a high sensitivity in the detection of deep endometriosis lesions in the uterosacral ligaments, vaginal wall, rectovaginal space, Douglas sac and rectosigmoid(5).
It can be performed on an outpatient basis, it is costless, it can be repeated in dynamics without possible side effects compared to pelvic MRI, therefore it is considered a first-line investigation when the clinical suspicion of endometriosis is raised.
Materials and method
We conducted a retrospective study, between 2017 and 2021, on a group of 126 patients, aged between 25 and 50 years old, operated in the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology, Euroclinic Hospital – Private Health Network, and Monza Hospital, Bucharest.
Results
The statistical analysis was performed using IBM SPSS Statistics 25 and Microsoft Office Excel/Word 2013. Quantitative variables were tested for distribution using the Shapiro-Wilk test and were expressed as means with standard deviations or medians with interpercentile intervals. The categorical variables were expressed in absolute or percentage form and were tested using the Fisher’s Exact Test.
The existing correlations were made using the Pearson and Spearman’s rho correlation coefficient, depending on the distribution of quantitative variables.
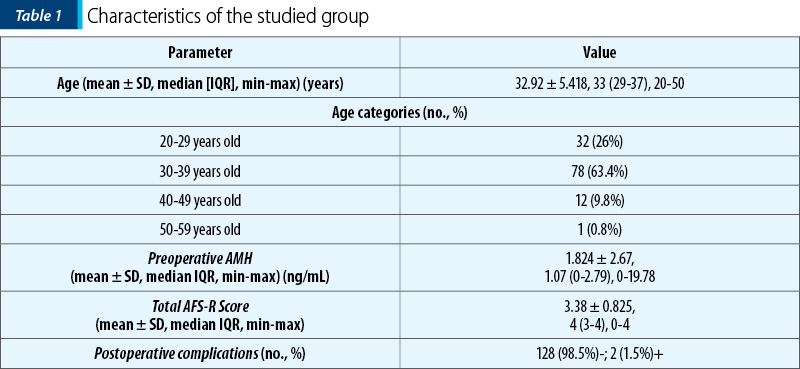
The data in Table 1 represent the characteristics of the studied group. The following are observed:
-
The average age is 32.92 ± 5.418 years old, with a median of 33 years old.
-
The most common age category is 30-39 years old (63.4%).
-
The mean value of preoperative AMH is 1.824 ± 2.67 ng/mL, with a median of 1.07 ng/mL.
-
The average total AFS-R score is 3.38 ± 0.825 points, with a median of 4 points.
-
Most patients did not have postoperative complications (98.5%), only two patients had postoperative complications (postoperative fever and rhabdomyolysis).
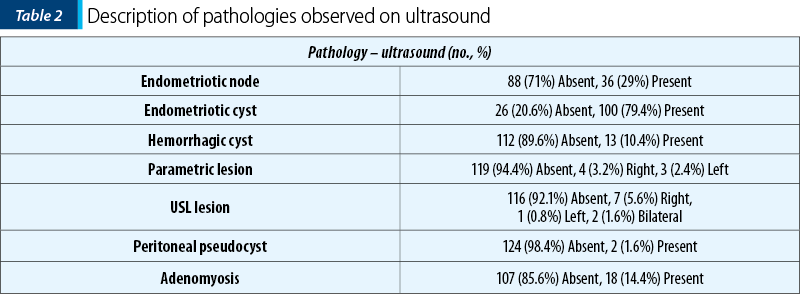
The data in Table 2 represent the description of the pathologies observed ultrasound, describing the following:
-
29% of the patients had an endometriotic node.
-
79.4% of the patients had endometriotic cyst.
-
10.4% of the patients had hemorrhagic cyst.
-
5.6% of the patients had parametric lesion, more frequently straight (3.2%).
-
7.9% of the patients had LUS lesion, more frequently right (5.6%).
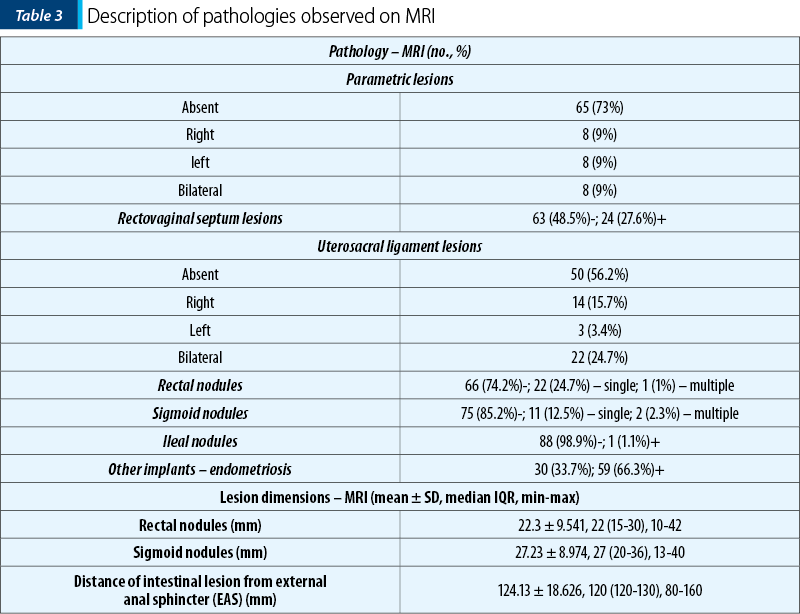
The data in Table 3 represent the description of the pathologies observed on MRI. The following are observed:
-
27% of the patients had parametric lesions (right, left or bilateral).
-
27.6% of the patients had lesions of the rectovaginal septum.
-
43.8% of the patients had uterosacral ligament lesions, more frequently bilateral (24.7%).
-
25.8% of the patients had rectal nodules, more frequently unique (24.7%).
-
14.8% of the patients had sigmoid nodules, more frequently unique (12.5%).
-
1.1% of the patients had ileal nodules.
-
66.3% of the patients had other locations of endometriosis.
-
The average size of the rectal nodules was 22.3 ± 9.541 mm, with a median of 22 mm (IQR = 15-30 mm).
-
The average size of the sigmoid nodules was 27.23 ± 8.974 mm, with a median of 27 mm
-
(IQR = 20-36 mm).
-
The average distance of intestinal lesions from the external anal sphincter was 124.13 ± 18.626 mm, with a median of 120 mm (IQR = 120-130 mm).
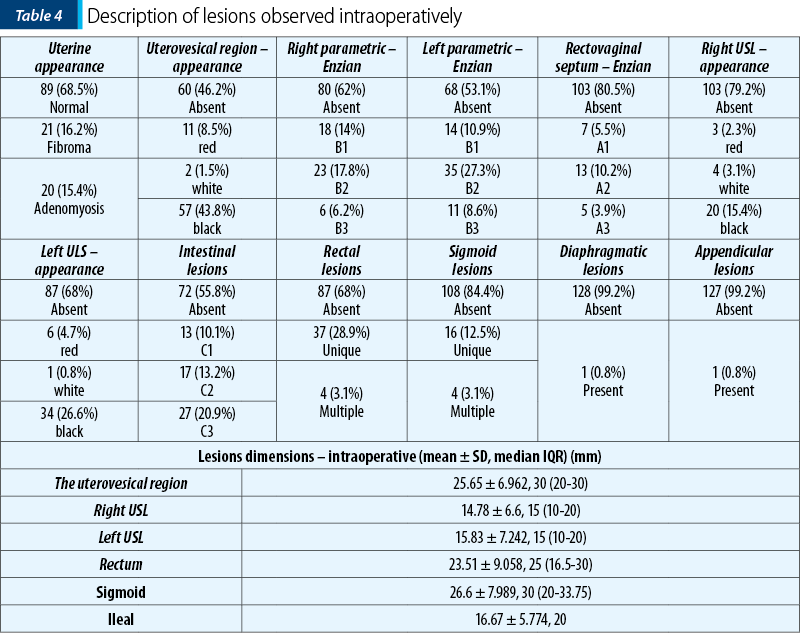
The data in Table 4 represent the description of the pathologies observed intraoperatively. The following are observed:
-
Most patients had a normal appearance of the uterus (68.5%), 16.2% of the patients had fibroids and 15.4% of the patients had adenomyosis.
-
53.8% of the patients had anterior sac lesions, more frequently with a black appearance (43.8%), with an average size of 25.65 ± 6.962 mm.
-
38% of the patients had straight parametric lesions, more frequently class B2 (17.8%), and 46.9% of the patients had left parametric lesions, more frequently class B2 (27.3%).
-
19.5% of the patients had lesions of the rectovaginal septum, more frequently class A2 (10.2%).
-
20.8% of the patients had straight USL lesions, more frequently with a black appearance (15.4%) and an average size of 14.78 ± 6.6 mm, and 32% of the patients had left USL lesions, more frequently with a black appearance (26.6%) and with an average size of 15.83 ± 7.242 mm.
-
44.2% of the patients had intestinal lesions, more frequently class C3 (20.9%), 32% had rectal lesions, more frequently single (28.9%), with an average size of 23.51 ± 9.058 mm, 15.6% had sigmoid lesions, more frequently unique (12.5%), with an average size of 26.6 ± 7.989 mm.
-
0.8% of the patients had diaphragmatic or appendicular invasion.
The data in Table 5 and Figure 1 represent the comparison of ultrasound/MRI and intraoperative endometriosis diagnoses. According to the data, the MRI diagnosis of endometriosis lesions is clearly superior, having a higher accuracy compared to the ultrasound diagnosis.
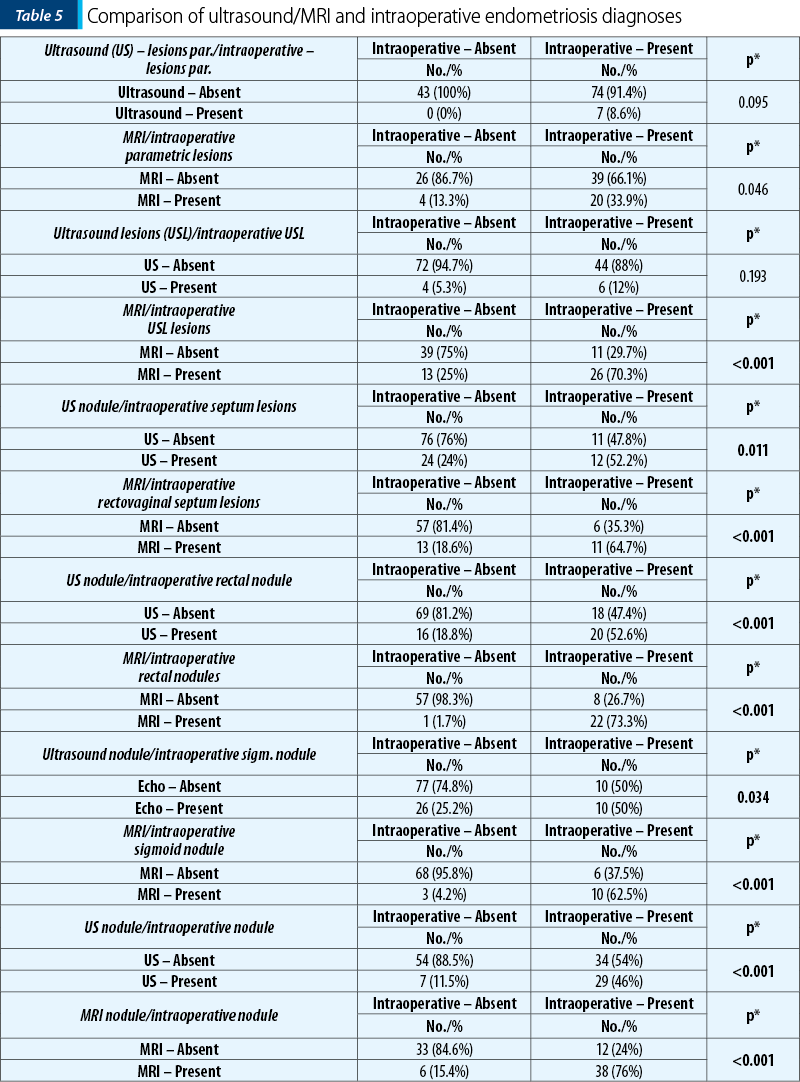
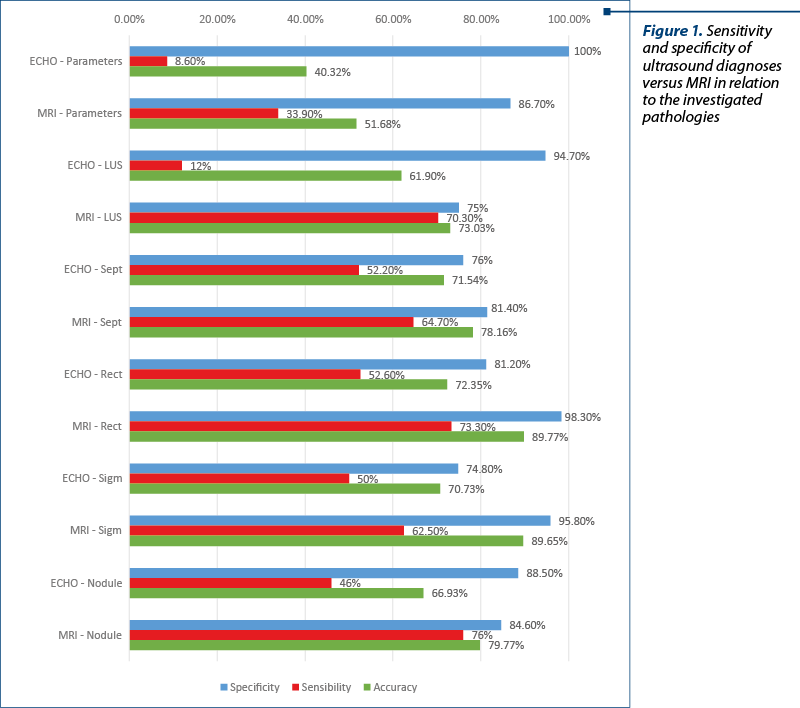
For parametric lesions: MRI accuracy 51.68% versus ECO accuracy 40.32%; MRI sensitivity 33.9% versus ECO sensitivity 8.6%; MRI specificity 86.7% versus ECO specificity 100%.
For USL lesions: MRI accuracy 73.03% versus ECO accuracy 61.9%; MRI sensitivity 70.3% versus ECO sensitivity 12%; MRI specificity 75% versus ECO specificity 94.7%.
For rectovaginal septal lesions: MRI accuracy 78.16% versus ECO accuracy 71.54%; MRI sensitivity 64.7% versus ECO sensitivity 52.2%; MRI specificity 81.4% versus ECO specificity 76%.
For rectal lesions: MRI accuracy 89.77% versus ECO accuracy 72.35%; MRI sensitivity 73.3% versus ECO sensitivity 52.6%; MRI specificity 98.3% versus ECO specificity 81.2%.
For sigmoid lesions: MRI accuracy 89.65% versus ECO accuracy 70.73%; MRI sensitivity 62.5% versus ECO sensitivity 50%; MRI specificity 95.8% versus ECO specificity 74.8%.
For peritoneal endometriotic nodules: MRI accuracy 79.77% versus ECO accuracy 66.93%; MRI sensitivity 76% versus ECO sensitivity 46%; MRI specificity 84.6% versus ECO specificity 88.5%.
Discussion
In our study, the accuracy of MRI proved to be clearly superior in the diagnosis of parametric lesions, uterosacral ligaments, rectovaginal septum and upper intestinal lesions.
Transvaginal ultrasound has a high sensitivity in detecting deep endometriosis of the uterosacral ligament, rectovaginal septum, the vaginal wall of the Douglas sac and the rectosigmoid.
Conclusions
There is no single imaging device that can be used individually and be sufficiently efficient to identify the location and extent of endometriosis. The performance of these imaging procedures should be considered depending on the type of suspected endometriosis, the proposed therapeutic strategy and the information to be provided to the patient.
Transvaginal ultrasound is a costless, repeatable procedure that can be used to diagnose certain types and locations of endometriosis. The role of transvaginal ultrasound is to guide the type of subsequent complementary investigations depending on the location of the lesions, when suspected(6).
The diagnosis of endometriosis is closely dependent on the operator.
A multidisciplinary approach with superior outcomes is needed in terms of complete resection of endometriotic lesions and improvement of the quality of life of the patient with deep infiltrative endometriosis(7).
High-resolution transvaginal ultrasonography and in particular magnetic resonance imaging are increasingly used to diagnose the presence and extent of infiltrating lesions and the involvement of rectosigmoid and ureters(8,9).
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Koninckx PR, Meuleman C, Demeyere S, Lesaffre E, Cornillie FJ. Suggestive evidence that pelvic endometriosis is a progressive disease, whereas deeply infiltrating endometriosis is associated with pelvic pain. Fertil Steril. 1991;55(4):759–65.
-
Liang Y, Yao S. Potential role of estrogen in maintaining the imbalanced sympathetic and sensory innervation in endometriosis. Mol Cell Endocrinol. 2016;424:42–9.
-
Vercellini P, Viganò P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10(5):261–75.
-
Mehedintu C, Plotogea MN, Ionescu S, Antonovici M. Endometriosis still a challenge.
-
J Med Life. 2014;7(3):349–57.
-
Guerriero S, Saba L, Pascual MA, Ajossa S, Rodriguez I, Mais V, et al. Transvaginal ultrasound vs. magnetic resonance imaging for diagnosing deep infiltrating endometriosis: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(5):586–95.
-
Chamié LP. Ultrasound evaluation of deeply infiltrative endometriosis: technique and interpretation. Abdom Radiol (NY). 2020;45(6):1648–58.
-
Scardapane A, Lorusso F, Francavilla M, Bettocchi S, Fascilla FD, Angelelli G, et al. Magnetic Resonance Colonography May Predict the Need for Bowel Resection in Colorectal Endometriosis. Biomed Res Int. 2017;2017:5981217.
-
Brosens I, Puttemans P, Campo R, Gordts S, Kinkel K. Diagnosis of endometriosis: pelvic endoscopy and imaging techniques. Best Pract Res Clin Obstet Gynaecol. 2004;18(2):285–303.
-
Chamié LP, Blasbalg R, Pereira RMA, Warmbrand G, Serafini PC. Findings of pelvic endometriosis at transvaginal US, MR imaging, and laparoscopy. Radiographics. 2011;31(4):E77-100.
Articole din ediţiile anterioare
Diagnosticul adenomiozei uterine la pacientele de vârstă reproductivă
Adenomioza uterină este o patologie ginecologică ce este caracterizată de prezenţa insulelor ectopice de ţesut endometrial în miometru. Această ...
Localizarea ultrasonografică a implantelor endometriozice
Obiective. Evaluarea principalelor tehnici ultrasonografice de diagnostic al endometriozei, evidenţiind tehnica, avantajele şi limitele fiecărei me...