Ovarian fibromas are representative in the group of solid benign tumors of the ovary, accounting for 4% of all ovarian masses. Ovarian fibromas have sex cord/stromal origin and appear particularly in the fourth or fifth decade in menopausal women. The aim of this study is to determine the accurate and reproducible ultrasound elements for the diagnosis of ovarian fibromas, through a comparative analysis between the specialty literature and the experience from the “Filantropia” Clinical Hospital of Obstetrics and Gynecology, Bucharest. Mostly clinical asymptomatic or with a nonspecific appearance, ovarian fibromas require a careful approach and a constant differential diagnosis with gynecological tumors, especially uterine pathology, and pelvic masses. This study describes eight clinical cases of ovarian fibromas, diagnosed in the “Filantropia” Clinical Hospital in 2018. All cases were unilateral ovarian tumors, diagnosed by ultrasonography and histopathologicaly confirmed, after surgical treatment. The surgical treatment is mandatory due to the difficult differential diagnosis and the possibility of a malignant involvement.
Diagnosticul ecografic al fibroamelor ovariene
Ultrasound diagnosis of ovarian fibromas
First published: 30 septembrie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.29.3.2020.4062
Abstract
Rezumat
Fibromul uterin reprezintă o tumoră benignă a ovarului, reprezentând 4% din formaţiunile ovariene. Acestea apar frecvent în a patra sau a cincea decadă a vieţii la femeile aflate la menopauză. Scopul studiului a fost de a determina elementele ultrasonografice de diagnostic pentru fibromul ovarian, prin intermediul unei analize comparative a literaturii de specialitate şi a experienţei din cadrul Spitalului Clinic de Obstetrică şi Ginecologia „Filantropia”, Bucureşti. Majoritatea fibroamelor ovariene au fost oligosimptomatice, cu simptome nespecifice, diagnosticul diferenţial realizându-se cu tumorile uterine şi ovariene. Studiul descrie opt cazuri de fibroame ovariene, diagnosticate în anul 2018 în Spitalul „Filantropia”. Toate cazurile au fost tumori unilaterale, diagnosticate prin ultrasonografie şi confirmate histopatologic postoperatoriu. Tratamentul chirurgical este esenţial, având în vedere dificultăţile de diagnostic diferenţial cu tumorile maligne.
Introduction
Solid ovarian tumors are peculiar but fascinating neoplasms, from an embryologic, morphologic and clinical point of view. The sex cord stromal ovarian tumors represent a group of ovarian tumors which most often present a wide range of endocrine manifestations due to estrogenic and androgenic hormone secretion. Confoundingly diverse, ovarian tumors are usually morphologically characterized as biphasic neoplasms, composed of both stromal and sex cord elements(1). Tumors in which cells resemble fibroblasts producing collagen or theca-cells belong to the fibroma-thecoma group. Ovarian fibromas are rarely associated with steroid hormone production and account for approximatively 4% of the cases of all ovarian masses. They are most commonly found in menopausal women in the fourth or fifth decade, and rarely appear in patients younger than 30 years of age.
Ovarian fibromas are sometimes associated with two uncommon syndromes, the basal cell nevus syndrome and Demons-Meigs syndrome. Demons-Meigs syndrome is defined by the presence of a fibrous ovarian tumor accompanied by ascites and pleural effusion which disappear after the removal of the tumor. Fibromas with this presentation are commonly edematous(2). The basal cell nevus syndrome – also called the nevoid basal cell carcinoma syndrome or Gorlin’s syndrome – is defined by the presence of at least one of the following: basal cell carcinoma in early life, keratocysts of the jaw, calcification of the dura, mesenteric cystis, ovarian fibromas. In this case, the ovarian tumors are bilateral, multinodular and calcified(3).
Mostly clinical asymptomatic or with a nonspecific appearance, ovarian fibromas require a careful approach and a constant differential diagnosis with both gynecological tumors, especially uterine pathology, and other pelvic masses. The surgical treatment is mandatory due to the difficult differential diagnosis and the possibility of microscopy focal fibrosarcomatous changes and therefore malignant involvement.
Patients and method
This is a retrospective study conducted in a university-affiliated tertiary gynecological referral center, the “Filantropia” Clinical Hospital of Obstetrics and Gynecology, Bucharest. All patients admitted between January 2018 and December 2018 with an operative diagnosis of an ovarian fibroma were identified from operating theatre records and computerized clinical management database. The demographic characteristics, the clinical presentations, the intraoperative findings, the operative procedures and the outcomes were recorded and analyzed.
Results
During the study period, eight cases with an operative diagnosis of ovarian fibroma were identified. There was a total of 189 cases of surgical removal of ovarian masses over the same period of time. The incidence of ovarian fibromas was, therefore, 4.23%. The statistical approach was performed using Excel data analysis.
Patient characteristics
The median age was 45 years old (range: 37-77), and five patients (62.5%) were postmenopausal women. None of the patients reported a positive family history of ovarian fibroma.
Clinical presentation
The most frequent symptom was abdominal pain (n=6, or 75%) associated with abdominal distension (n=5, or 62.5%). One patient presented menorrhagia and another patient was asymptomatic and the tumor was detected during routine gynecological examination. Upon physical examination, an abdominopelvic mass was detected in six patients (75%), and in all these cases it was difficult to differentiate it from a uterine mass.
Preoperative investigations and diagnosis
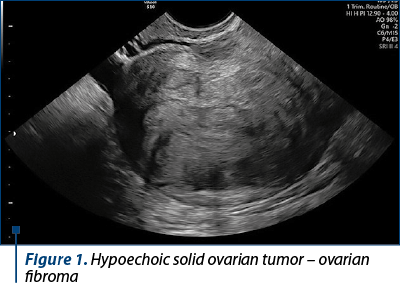
Transvaginal ultrasound was performed in all patients. The uterus was found to be normal in six cases and enlarged with fibroids in two cases. The size of ovarian fibromas ranged from 3 to 20 cm. Five patients had completely solid, hypoechoic masses with ultrasound beam attenuation (62.5%), and three had mixed echogeneity with both solid and cystic components (37.5%) – Figure 1. Free peritoneal fluid in the pouch of Douglas was found in three cases. In these patients, CA-125 value was minimally increased, as well as the suspicion of malignant ovarian pathology.
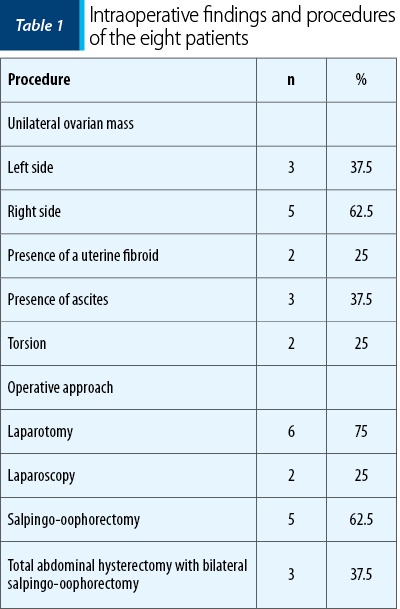
Intraoperative findings and procedures
All patients underwent surgical treatment: two by laparoscopy and six by laparotomy (Table 1). The intraoperative findings were: clear straw-colored peritoneal fluids of 500 ml up to 2900 ml in three patients, two cases of ovarian fibromas associated with 540° torsion, and two patients presented uterine fibromas (Figure 2). Both patients with torsion had large ovarian masses (15/12 cm and 15/10 cm), and this complication can be related to the size of the tumor. All tumors were unilateral: 5 (62.5%) on the right side, and 3 (37.5%) on the left side. The size of the tumors ranged from 4 to 20 cm, with a median of 10 cm. The tumors were smaller in the laparoscopy group, with a median of 5 cm. Both patients treated through the laparoscopy approach underwent salpingo-oophorectomy. In the laparotomy approach group, three patients underwent unilateral salpingo-oophorectomy and three patients underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy because of the large size of the tumors or suspicion of malignancy. Only three cases showed predominantly solid masses with focal areas of cystic changes. None of the patients had intraoperative surgical complications. The operative time in the laparoscopy group was 50 minutes (range: 40-60 minutes), and in the laparotomy group, 70 minutes (range: 50-90). All patients underwent extemporaneous biopsy, and the histopathological examination confirmed the diagnosis of ovarian fibromas and fibrothecomas, without cellular atypia or mitosis.
Postoperative course
The postoperative hospital stay was short both in the laparoscopy group (three days), and in the laparotomy group (four days). Uneventful postoperative outcome was noted in all cases.
Discussion
Ovarian fibromas are benign ovarian masses, difficult to diagnose due to the asymptomatic or nonspecific symptoms. Moreover, it is mandatory to make a careful differential diagnosis, because not only gynecological conditions, such as ovarian and uterine cystic or solid masses, but also pelvic tumors may present similar clinical findings.
Transvaginal ultrasound – and rarely abdominal ultrasound – is an essential investigation to differentiate ovarian fibromas from the more common uterine fibroids and other ovarian benign or malignant masses. The ultrasound findings that describe an ovarian fibroma, as the literature shows, can include a spectrum of sonographic features, from completely solid, hypoechoic masses with ultrasound beam attenuation to mixed echogeneity with both solid and cystic components(4). The investigator should pay attention to the tumor margins and the connection with the ovary or the uterus. Sometimes, an uterin fibroid with subserosal development can be diagnosed as ovarian fibroma, especially when it is described near the ovary. The vascular pattern on color Doppler assessment can differentiate between a uterine fibroid and an ovarian fibroma. It was observed that a well-vascularized solid pelvic mass with high-speed flow is suggestive of a subserosal fibroid, while a less vascularized tumor with low-speed flow points towards an ovarian fibroma(5). Another important aspect for the differential diagnosis is that a primary ovarian carcinoma appears rarely as a solid mass, and a secondary ovarian malignancy is typically bilateral(1).
In order to improve the preoperative description of the pelvic mass, computed tomography and magnetic resonance imaging can show particular findings. Ovarian fibromas appear as a solid mass with delayed accumulation of contrast medium on computed tomography scan and show marked T1and T2 hypointensities on magnetic resonance imaging(6,7).
In spite of the ultrasound findings observed to highly describe an ovarian fibroma, the confirmation of the diagnosis is entirely histological, after surgical treatment. An earlier series of 23 cases of ovarian fibromas made by A. Athchek et al., in 2003, showed that the risk of malignancies in solid ovarian tumors was 8.7% and that the diagnosis can only be established by histological assessment(1). In our study, all tumors were benign, but the number of cases was small, and therefore the absence of the malignancy might be just incidental.
The treatment is represented by conservative surgery by unilateral salpingo-oophorectomy, through a laparoscopy or laparotomy approach, depending on the tumor size. This procedure is available especially for patients at the reproductive age, with relatively small tumors and no other pelvic involvement. When the mass is suspected for malignancy, is large in size and appears in postmenopausal women, the total abdominal hysterectomy and bilateral salpingo-oophorectomy should be considered.
In conclusion, ovarian fibromas are uncommon gynecological conditions that require a proper differential diagnosis and surgical treatment due to the possibility of malignant involvement. The available data in literature about diagnosing and treating ovarian fibromas are poor. The condition should be further investigated in order to improve its management and to facilitate the gynecologist effort for diagnosing ovarian fibromas.
Bibliografie
-
Altchek A, Deligdisch L, Kase N. Diagnosis and management of ovarian disorders. Elsevier, 2nd ed, 2003;111-25.
-
Meigs J. Fibroma of ovary with ascites and hydrothorax. Meigs’ syndrome. Am J Obstet Gynecol. 1954;67(5):962-85.
-
Gorlin R. Nevoid basal cell carcinoma syndrome. Medicine (Baltimore). 1987;66(2):98-113.
-
Hartung MP. Ovarian fibroma. Available at: https://radiopaedia.org/articles/ovarian-fibroma. Accesed: 30.04.2019.
-
Valentin L. Gray scale sonography, subjective evaluation of the color Doppler image and measurement of blood flow velocity for distinguishing benign and malignant tumors of suspected adnexal origin. Eur J Obstet Gynecol Reprod Biol. 1997;72(1):63-72.
-
Bazot M, Ghossain M, Buy J, et al. Fibrothecomas of the ovary: CT and US findings. J Comput Assist Tomogr. 1993;17(5):754-9.
-
Schwartz R, Levine D, Hatabu H, Edelman RR. Ovarian fibroma: findings by contrast enhanced MRI. Abdom Imaging. 1997;22:535-7.
Articole din ediţiile anterioare
Studiu clinico-patologic al tumorilor ovariene - experienţa de un an într-un centru medical
Scopul acestui studiu este analiza retrospectivă a spectrului de tumori ovariene, din punct de vedere statistic, epidemiologic şi al caracteristi...
Raport de examinare ginecologică bazat pe consensul grupurilor internaţionale de studiu al tumorilor
Grupul IETA, fondat în 2008 la Chicago, cu ocazia Congresului Mondial de Ultrasonografie în Obstetrică şi Ginecologie, a publicat în ianuarie 2010 ...