Ectopic pregnancy is a serious health problem that leads to maternal mortality and morbidity. Ovarian pregnancy is a very rare variety of ectopic pregnancy and represents a medical challenge in terms of its management. Although the incidence of ovarian ectopic pregnancy is low, there is a high risk of severe complications (hemorrhagic shock) if it’s not identified and treated in time. The symptoms of ovarian ectopic pregnancy can be difficult to distinguish based on ultrasound imaging and clinical examination alone. Laparoscopic management is required for definitive diagnosis and treatment. Identifying these emergent cases early is very important because of the high risk of maternal death. We present the case of a 34-year-old female who accused left lower abdominal pain, whilst she declared 5 weeks and 4 days of amenorrhea and a positive pregnancy test. Transvaginal sonography identified a gestational sac in the very proximity of the left ovary. Laparoscopy was performed and so we discovered a purple tumor, 3.5/3 cm, with intense vascular drawing, situated on the left ovary. Thus, primary ovarian ectopic pregnancy was diagnosed and confirmed by histopathology. The postoperative evolution was favorable, the patient being discharged the next day postoperatively. Our purpose is to highlight the successful treatment with a minimally invasive surgical technique of an ovarian pregnancy.
Diagnosticul precoce al sarcinii ovariene – prezentare de caz
Early diagnosis of ovarian pregnancy – a case report
First published: 12 decembrie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.26.4.2019.2710
Abstract
Rezumat
Sarcina ovariană este o varietate foarte rară de sarcină ectopică şi reprezintă o provocare medicală în ceea ce priveşte managementul acesteia. Deşi incidenţa sarcinii ectopice ovariene este scăzută, există un risc ridicat de complicaţii severe (şoc hemoragic) dacă nu este identificată şi tratată la timp. Simptomele sarcinii ectopice ovariene pot fi dificil de diagnosticat doar pe baza aspectului ecografic şi a examenului clinic. Abordul laparoscopic este necesar pentru un diagnostic şi tratament definitiv. Identificarea timpurie a acestor cazuri este foarte importantă, din cauza riscului mare de deces matern. Prezentăm cazul unei femei de 34 de ani care a acuzat dureri abdominale inferioare în hipocondrul stâng, declarând 5 săptămâni şi 4 zile de amenoree şi un test de sarcină pozitiv. Ecografia transvaginală a identificat un sac gestaţional în imediata apropiere a ovarului stâng. S-a intervenit chirurgical pe cale laparoscopică şi s-a constatat prezenţa unei formaţiuni tumorale de culoare violacee, cu dimensiuni de 3,5/3 cm, cu desen vascular intens, situată pe ovarul stâng, diagnosticându-se o sarcină ectopică ovariană primară, confirmată de examenul histopatologic. Evoluţia postoperatorie a fost favorabilă, pacienta fiind externată a doua zi postoperatoriu. Scopul nostru este de a evidenţia succesul tratamentului chirurgical minim invaziv în contextul unei sarcini ovariene.
Introduction
Ovarian ectopic pregnancy is a rare type of ectopic pregnancy with an estimated prevalence between 1:7000 and 1:70,000, representing 3% of all ectopic cases(1).
The symptoms mimic those of ectopic tubal pregnancy and can be difficult to differentiate only on the basis of the ultrasound image and on the clinical and paraclinical examination. The laparoscopic management is most often required for the diagnosis and treatment of ovarian pregnancy. The early identification of these cases is imperative because of the high risk of maternal death(2).
It usually ends in a gestational sac rupture in the first trimester of pregnancy due to increased ovarian tissue vascularization that will lead to internal bleeding and hypovolemic shock. The diagnosis is usually made by emergency laparoscopy and histopathological evaluation(2). There are two types of ovarian pregnancy: the primary ovarian pregnancy, when implantation occurs at the level of the ovary per prima, and the secondary ovarian pregnancy, when the primary nesting occurs at the level of the fallopian tube and subsequently the ovarian attachment results second into tubal abortion(3).
Case presentation
We present the case of a 34-year-old female with a history of a full-term pregnancy, by caesarean section, in 2015, with previous regular menstrual cycle and with declared intent to conceive again, also known with a total thyroidectomy in 2017, in treatment with Euthyrox® 100 mcg, 1 cp/day, who was admitted into the surgical emergency department of the “Elias” University Hospital, in May 2019. She presented with left lower abdominal pain, with 5 weeks and 4 days of amenorrhea and a positive result on the pregnancy test. bHCG level was 7.749 mIU/mL. The vaginal examination found a tender cystic mass palpable in the left fornix. Transvaginal ultrasonography showed empty uterine cavity with 11 mm thickness. An ectopic gestational sac and yolk sac seemed to be inside her left ovary, and were identified close to the midline, which correlated with her 6-week amenorrheea. The fetus and fetal heart beat were not clearly seen. The vascular proliferation called “ring of fire” – which is typical for ectopic ovarian pregnancy – was detected around the gestational sac. Her right ovary and tubal structures seemed to be normal; no liquid in the Douglas sac. The diagnosis of left ovarian ectopic pregnancy was established and the patient was hospitalized for specialized treatment.
At the hospital, the patient was conscious, cooperative, oriented temporally and spatially, with blood pressure 100/50 mmHg, and heart rate 75/min. A physical examination showed minimal tenderness in all sides of her abdomen with an increase sensibility in the left lower pelvic section. A speculum examination showed a small amount of cervical bleeding. On the vaginal examination, the vagina and cervix were normal and the uterus had a normal size; a tender chystic mass was palpable in the left fornix.
Laboratory analyses showed a white blood cell count (WBC) of 66.40/uL, hemoglobin (Hb) 12.9 g/dl, hematocrit (Htc) 37.9%, thrombocytes 185,000 uL, beta human chorionic gonadotropin (b HCG) 7749, blood group 0I and Rh+, and normal urine results. Laparoscopic surgery was decided under general anesthesia with oro-tracheal intubation.
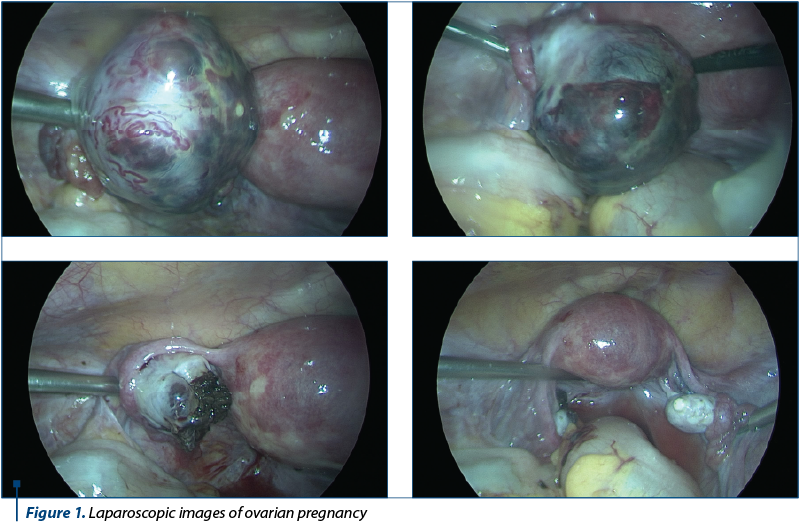
The laparoscopic surgery was performed, which revealed: the uterus of normal macroscopic appearance, the bilateral tubes and the right ovary were normal, at the level of the left ovary there was a purple tumor (3.5/3 cm), with intense vascular drawing (Figure 1).
The incision of the tumor was practiced with the externalization of an increased amount of blood and of trophoblastic tissue; hemostasis was difficult to achieve, the remaining ovary was sutured in order to ensure the hemostasis. The abdominal cavity was washed, hemostasis checked and drainage of the Douglas space was placed.
The evolution of the patient was favorable, being discharged 24 hours postoperatively.
The histopathological result revealed multiple fragments representing blood clots and numerous chorionic villi with non-specific modifications, trophoblast fragments without circumferential arrangement; ovarian stroma, no trophoblastic disease elements were identified; histopathological appearance of ovarian pregnancy with non-specific changes.
Discussion
The diagnostic criteria for ovarian pregnancy are the Springelberg criteria, described 100 years ago(4):
-
Gestation sac located in the ovary area.
-
The gestational sac is attached to the uterus by the ovarian ligament.
-
Ovarian tissue present in the gestational sac identified histopathologically.
-
The uterine tube on the involved side is intact.
The risk factors for the onset of ovarian pregnancy are(5):
Intrauterine devices.
-
Pelvic inflammatory disease.
-
Sexually transmitted diseases.
-
Assisted reproduction techniques.
-
Surgery in the pelvic aria in the past.
-
Endometriosis.
-
Ectopic pregnancy in the background.
-
Salpingitis.
-
Advanced maternal age.
-
Multiparity.
The actual cause of the abnormal implantation is unclear. Some theories suggest that the abnormal implantation that occurs in the ovarian pregnancy is the result of the following:
-
Migration of the embryo related to the presence of certain conditions that cause epithelial lesions of the uterine tube which alter the tubular motility(6).
-
Failure to release the egg from the broken follicle(7).
-
Inflammatory thickening of tuna albuginea(2).
The signs and symptoms that appear in the ovarian pregnancy are: moderate or intense pelvic pain, vaginal bleeding, amenorrhea, irregular menstrual cycle, nausea, vomiting, constipation, hemorrhagic shock in case of a rupture(5).
The ultrasound criteria in case of ovarian pregnancy are: free endometrial cavity, gestational sac that is identified at the level of the ovarian parenchyma, yolk sac with or without embryo image depending on the gestational age, image “crown of fire” (vascular proliferation) visible around the gestational sac, the presence of the ovarian cortex including corpus luteum and follicles around and with a much more pronounced echogenic ring than the ovary(8). Most ovarian pregnancies rupture before the 40th day of pregnancy, although there have been reports of a number of pregnancies that reached the third trimester(9). The differential diagnosis is made in this case with: cyst of corpus luteum, hemorrhagic ovarian cyst, endometrioma, tubal ectopic pregnancy, early intrauterine pregnancy or stopped in evolution, and in case of negative pregnancy test with appendicitis(10). The gold standard in the diagnosis and treatment of ovarian pregnancy is represented by laparoscopy or laparotomy with histopathological confirmation. However, laparoscopy has many advantages over laparotomy: shorter operative time, reduced blood loss, reduced hospitalization days and low postoperative analgesia(10). When choosing the right treatment, the patient’s desire to obtain a pregnancy should be taken into consideration. The conservative treatment with trophoblast resection or thinning or cystectomy with hemostatic suture is preferable to ovarectomy because the patient keeps her fertility(5).
The success of methotrexate in the management of ovarian pregnancy is still undetermined and generally impractical, only a few case studies reporting its use(11-13). The single dose of methotrexate and multidose were successfully used to treat stable patients with ovarian pregnancy with hCG levels up to 5200 mIU/mL. Most commonly, methotrexate is used in the treatment of increased beta-hCG following surgical treatment(14). Although it is less invasive than surgical treatment, there have been many cases of failure and even major ovarian bleeding(2,15).
In this case, we chose minimally invasive surgical treatment to ensure a high success rate. The Taiwan Institute, in a study of 110 patients with ovarian pregnancies over 21 years old, concluded that 70.9% of them were treated by laparoscopy and 29.1% by laparotomy, and none of the patients received drug treatment(16).
The treatment of ectopic pregnancies with the help of laparoscopic surgery is best indicated because the pregnancies are small in size, contain low consistency tissue which allows the extraction of fragments through the laparoscopic incisions, using the endobag, and also the morcellator allows the extraction of larger tissues(17). Due to a faster postoperative recovery of the patient after a laparoscopic intervention, the success rate in obtaining a normal intrauterine pregnancy is higher.
Conclusions
The diagnosis with the latest ultrasonography scanner and the experience in laparoscopic surgery have proven succes in treating ovarian pregnancy through minimally invasive surgery. Laparotomy was avoided, hospitalization days and costs were reduced, and the patient did not need adjuvant treatments. This method is safe when performed by an experienced operator and has the advantage of keeping fertility for the future.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
- Marcus SM, Brinsden PR. Primary ovarian pregnancy after in vitro fertilization and embryo transfer: report of seven cases. Fertil Steril. 1993; 60(1):167–70.
- Birge O, Erkan MM, Ozbeyand EG, Arslan D. Medical management of an ovarian ectopic pregnancy: a case report. J Med Case Rep. 2015; 9(1):290.
- Russell JB, Cutler LR. Transvaginal ultrasonographic detection of primary ovarian pregnancy with laparoscopic removal: a case report. Fertil Steril. 1980; 51(6):1055–6.
- Spiegelberg O. The causes of ovarian pregnancy. Arch Gynaecol. 1878; 13:73-9.
- Sotelo C. Ovarian ectopic pregnancy: a clinical analysis. J Nurse Pract. 2019; 15(3):224-7.
- Mathur SK, Parmar P, Gupta P, Kumar M, Gilotra M, Bhatia Y. Ruptured primary ovarian ectopic pregnancy: case report and review of the literature. J Gynecol Surg. 2015; 31(6):354-6.
- Melcer Y, Maymon R, Vaknin Z, Pansky M, et al. Primary ovarian ectopic pregnancy: still a medical challenge. J Reprod Med. 2016; 61(1-2):58-62.
- Roy J, Babu AS. Ovarian pregnancy: two case reports. Australas Med J. 2013; 6(8):406-10
- Choi HJ, Im KS, Jung HJ, Lim KT, Mok JE, Kwon YS. Clinical analysis of ovarian pregnancy: a report of 49 cases. Eur J Obstet Gynecol Reprod Biol. 2011; 158(1):87-9.
- Tehrani HG, Hamoush Z, Ghasemi M, Hashemi L. Ovarian ectopic pregnancy: a rare case. Iran J Reprod Med. 2014; 12(4):281-4.
- Shen L, Fu J, Huang W, Zhu H, Wang Q, Yang S, Wu T. Interventions for non-tubal ectopic pregnancy. Cochrane Database of Systematic Reviews. 2014; 7:CD011174.
- Chetty M, Elson J. Treating non-tubal ectopic pregnancy. Best Pract Res Clin Obstet Gynaecol. 2009; 23(4):529–38.
- Alalade A, Mayers K, Abdulrahman G, Oliver R, Odejinmi F. A twelve year analysis of non-tubal ectopic pregnancies: do the clinical manifestations and risk factor for these rare pregnancies differ from those of tubal pregnancies?. Gynecol Surg. 2015; 13(2):103-9.
- Parker VL, Srinivas M. Non-tubal ectopic pregnancy. Arch Gynecol Obstet. 2016; 294(1):19-27.
- Ghaneie A, Grajo JR, Derr C, Kumm TR. Unusual ectopic pregnancies: sonographic findings and implications for management. J Ultrasound Med. 2015; 34(6):951–62.
- Ko PC, Lo LM, Cheng PJ. Twenty-one years of experience with ovarian ectopic pregnancy at one institution in Taiwan. Int J Gynaecol Obstet. 2012; 119(2):154–8.
- Petca A, Veduta A, Mehedinţu C, Maru N, Petca R, Boţ M. Ectopic pregnancy în rudimentary horn: early diagnosis and management. Ginecologia.ro. 2018; 20(2):20-2.
Articole din ediţiile anterioare
Sarcină ectopică în corn rudimentar: diagnostic precoce şi management
Sarcina în corn rudimentar este o entitate clinică rară, cu o incidenţă ce variază între 1:76.000 şi 1:140.000 de sarcini. Simptomatologia care îns...
Un caz rar de sarcină abdominală secundară – prezentare de caz şi review al literaturii
Sarcina abdominală este o formă foarte rară de sarcină extrauterină şi este asociată cu o rată ridicată a mortalităţii. Principala complicaţ...
Sarcina ectopică cu evoluţie atipică
Prezentăm cazul unei paciente în vârstă de 32 de ani, cu istoric de infertilitate de cauză neexplicată (2 inseminări şi 2 fertilizări in vitro pe c...
Relaţia dintre cicatricea uterină determinată de intervenţii histeroscopice şi abdomenul acut chirurgical în sarcină - prezentare de cazuri -
Abdomenul acut chirurgical în cursul sarcinii reprezintă o entitate patologică, plurietiologică, cu evoluţie rapidă şi risc vital atât pentru partu...