One of the most common gynecological pathologies is the myoma, with a great socioeconomic burden. One of the uterine-sparing treatment is represented by the uterine artery embolization (UAE). The objective of this study is to evaluate this treatment method mainly through evolution of symptomatology and the quality of life impact. We studied a number of 36 patients who underwent UAE between January 2015 and March 2018. They were evaluated at the beginning of the study, after a month and after three months. At one month after the procedure, we evaluated the evolution of symptomatology, the Pictorial Blood Loss Assessment Chart (PBAC) score and the ultrasound post-procedural aspects. In addition, at three months we evaluated the quality of life impact (uterine fibroid symptoms and health-related quality of life questionnaire). At the final evaluation, 88.88% of the patients reported a significant improvement in symptomatology (z=-5.030; p<0.001), with a significant reduction in PBAC score, the ultrasounds showed a decrease in uterine fibroid volume (t=2.113; p=0.049) and the quality of life was improved (p<0.001). UAE leads to the control of fibroid-related symptoms and improves the quality of life.
Embolizarea arterelor uterine în uterul fibromatos – controlul simptomatologiei şi îmbunătăţirea calităţii vieţii
Uterine artery embolization for leiomyomata – symptoms control and quality of life
First published: 27 decembrie 2018
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.22.4.2018.2140
Abstract
Rezumat
Uterul fibromatos reprezintă una dintre cele mai frecvente patologii ginecologice, constituind o adevărată povară socioeconomică. Unul dintre tratamentele conservatoare pentru fibromul uterin este reprezentat de embolizarea arterelor uterine (UAE). Obiectivul acestui studiu este de a evalua această metodă de tratament, evidenţiind evoluţia simptomatologiei şi impactul asupra calităţii vieţii. A fost inclus un număr de 36 de paciente ce au optat pentru EAU între ianuarie 2015 şi martie 2018. Evaluările lotului au avut loc la începutul studiului, la o lună de la procedură şi ulterior la trei luni. La o lună după această procedură, am evaluat evoluţia simptomatologiei, scorul raportat la pierderile sangvine (PBAC Pictorial Blood Assessment Chart) şi modificările ecografice. În plus, la trei luni am evaluat impactul asupra calităţii vieţii prin utilizarea chestionarelor privind calitatea vieţii. La evaluarea finală, 88,88% dintre paciente au raportat o îmbunătăţire semnificativă a simptomatologiei (z=-5,030; p<0,001), cu o reducere semnificativă a scorului PBAC, examinarea ecografică a arătat o scădere a volumului fibromului uterin (t=2,133; p=0,049), iar calitatea vieţii s-a îmbunătăţit în toate aspectele ei (p<0,001). EAU conduce la controlul simptomelor determinate de fibromul uterin şi îmbunătăţeşte semnificativ calitatea vieţii pacientelor care aleg această metodă de tratament.
Introduction
Embolization is a relatively new branch in interventional radiology which has demonstrated its utility in many areas. As with any procedure, it is necessary to correctly identify the patients who could benefit most from uterine artery embolization (UAE). The ideal candidates are patients with symptomatic uterine fibroids who wish to preserve the uterus and the fertility and/or want to avoid surgery. The aim of the procedure is to reduce the symptoms specifically manifested by abundant bleeding, neuralgia compression, abdominal discomfort or abdominal pain(1). Thus, especially at this point, due to the psychosocial implications on the patient, an important role is represented by the minimally invasive therapeutic approach of this pathology. The primary goal of the UAE is to stop the atypical bleeding followed by diminishing the fibroid volume. The literature confirms the efficacy of this treatment associated with much reduced morbidity and mortality. Regarding fertility, although it was initially considered that UAE would not be an eligible treatment for fertility preservation, ulterior studies have demonstrated the feasibility of achieving a pregnancy. The pregnancy following UAE involves a higher incidence of complications(2). The remission of symptomatology in literature is consider to be 80.9-90.8%, with the following cumulative symptom control rate: 96.9% at one year, 94.5% at two years, 89.5% at three years, 89.5% at four years, and 89.5% at five years(3-6). The decrease in symptomatology at different time intervals was 88.5% at 3-6 months(7) and 82% at two years(8). The study realized by Katsumor et al.(9) (96.9%, 94.5%, 89.5%, 89.5%, and 89.5% respectively) considered that the major benefit was the absence of other surgical interventions. The average time between procedure and intervention in cases requiring surgery was approximately 20 months(9). The main effect of UAE is the reduction of abnormal bleeding. Their reduction was found in 86-92% of cases(6,10), with 94% reduction in metrorrhagia and 83% reduction in menorrhagia(11). The impact on the urinary tract was favorable in 73-89% of the cases(11). Hydronephrosis due to fibrous compression was significantly reduced after the procedure(12). Pelvic pain and discomfort were ameliorated in 76% of cases(10). The long-term clinical efficacy of UAE was evaluated with follow-ups for approximately 6 years in a study conducted by Scheurig-Muenkler. The results showed the symptoms control rate and the normalization of the quality of life in 75% of cases, with 54 patients with treatment failure(13). A meta-analysis realized in 2018(14), which included 85 articles representing 17,789 women, showed a reintervention risk of 14.4% (95% CI; 9.8-19.6%) for UAE.
As we can see in the literature, the patient satisfaction after the procedure is high, even though afterwards another therapy is necessary; the scores regarding symptoms severity reduce and the HRQL scores increase(15).
The patient reassessment is performed by imaging control (ultrasound or magnetic resonance)(16). Most studies performed show a decrease in uterine volume and individual nodules, with vascular changes represented by decreased blood supply(11,17,18). Their decrease was reported at three months (37-40%) and at six months (37-40%)(4,19,20). The reduction in fibroid volume is variable, showing differences depending on the embolus material used, dimensions, localization, vascularization and total evaluation of the uterus or only the fibroid nodules.
Method
In order to obtain the necessary data, we conducted a prospective observational study that included patients who addressed the Obstetrics and Gynecology service between January 2015 and March 2018. The statistical analysis was done using the SPSS 20 (Statistical Package for Social Sciences) program, which we used for planning and collecting data, as well as for their management, reporting and presenting the results. The study included a total of 36 patients (30-51 years old) who were admitted to the Obstetrics and Gynecology Department of the University Emergency Hospital Bucharest for a fibroid uterus between January 2015 and March 2018, followed by UAE. We used as inclusion criteria: fertile females or premenopausal patients, the presence of uterine fibroids (minimum one), the agreement of the patient to be included in the study, patient desire to undergo UAE. The exclusion criteria were represented by: patient’s refusal to perform the intervention, allergies to use substances in the procedure, the treatment with ulipristal acetate in the past, vascular features such as ileo-femoral artery occlusions or aorto-iliac, current pregnancy, inflammatory pelvic diseases, the presence of progesterone-releasing intrauterine devices, endometrial hyperplasia, anticoagulant treatment in progress, and other decompensated pathologies (renal failure, uncontrolled hypertension, congestive heart failure or any other pathology that could endanger the patient at the time of surgery).
The follow-up protocol for patients included the initial evaluation, the follow-up at one month and the follow-up at three months. The initial evaluation included anamnesis, complete clinical examination, paraclinical examination (biological sampling and imaging examinations), filling in the quality of life questionnaires (uterine fibroid symptom and health-related quality of life questionnaire; UFS-QOL), the evaluation of bleeding with PBAC. UAE was performed in the intervention radiology department; brachial approach through the Seldinger method, 700-900 µm microspheres were used. At one month, we evaluated the symptomatology during the post-procedure month, with complete clinical exam, imaging examinations, and PBAC score. At three months, the symptomatology was evaluated, the clinical and imaging evaluation was performed, PBAC score was realized, and the quality of life questionnaires were applied. After one month, 36 patients were evaluated, but at the three-month evaluation only 18 of them presented.
Results
In the study group, the average age was 38.78 years old. The mean Body Mass Index was 25.58. In the evaluated group, coffee consume was found in 29 patients (80.55%), alcohol (affirmative) in four patients (11.11%), and tobacco in 21 patient (58.33%). Thirteen patients (36.11%) took combined oral contraceptives over the last three years. As a heredocolateral history, 8 patients (22.22%) had their mother or sister known with uterine fibroids. The average age when menarche installed was 12.39 years, 47.2% of the patients had no birth (17 patients) and 38.9% had no abortion.
Most patients (69.4%; 25 cases) described the bleeding as being severe. Six patients (16.7%) had moderate symptoms and only four patients (11.1%) had a mild symptomatology. One person did not experience symptoms such as bleeding. Most patients (44.4%; 16 patients) had menometrorrhagia, 38.9% (14 patients) had metrorrhagia, and 13.9% had menorrhagia (5 patients). There was also a patient who did not show altered bleeding during menstruation or between menses. In this case, UAE was performed in order to prevent the development of the myoma. Bleeding was quantified using the Pictorial Blood Loss Assessment Chart (PBAC). The baseline means PBAC was 279.92, with a minimum of 34 (for the asymptomatic patient) and a maximum of 1008. The median was 203 and the standard deviation was 203. The mean hemoglobin level was 10,024 g/dl. In the first month, a statistically significant reduction in bleeding was highlighted (z=-4,617; p<0.001); 72.33% of the patients reported a reduction in bleeding. After three months, the results indicated that the treatment had a significant effect, with significant differences between pre- and post-treatment scores (z=-5.030; p<0.001), the symptomatology being much lower at three months post-treatment compared to the previous situation (88.88% patients). The magnitude of this effect is 0.83, which reveals a strong effect of treatment on the decrease in bleeding. These results are supported by the values obtained for PBAC at one month and at three months after embolization. If initially the median value was 279.92, the scores decreased at 149.14 after one month and at 120.63 by three months. The differences were statistically significant (1 month t=5.655; df=35; p<0.001; 3 months t=4.786; df=18; p<0.001).
In addition to abnormal bleeding, patients with myomas may experience urinary symptoms, transit disorders, dysmenorrhea or dyspareunia, as a side effect of pelvic discomfort caused by leiomyoma. These other symptoms affected an increased number of patients, even though at different intensities. Thus, polyuria was present in 91.66% of patients (33 cases), transit disorders in 77.77% of cases (28 patients) and dysmenorrhea and dyspareunia were described by 88.88% of the cases (33 patients) and 58.33% of cases (21 patients). After one month, polyuria was resolved in 63.63% of the patients who had initial symptoms (z=-4.070; p<0.001; r=0.68) and in 63.15% at three months (z=-4.549; p<0.001; r=0.76). Regarding intestinal transit, 53.57% of the affected patients were found to have a remission of symptoms at one month after embolization, and 55.55% of all patients had the same intensity. At three months, the remission of symptoms occurred in 11 patients (73.33%). Transit differences were statistically significant in both one month (z=-2.982; p=0.003) and three months (z=-4.443; p<0.001). Dysmenorrhea affected 88.9% of the patients: 30.6% had severe symptoms, 30.6% had mild symptoms and 27.8% had moderate symptoms. The intensity at one month after treatment is significantly lower than initially (z=-4.066; p<0.001). Also, there were significant differences between the values after three months (z=-4.371; p<0.001). Dysmenorrhea at one month was resolved in 57.14% of the patients who had initial symptoms and in 90.90% of the patients at three months. Dyspareunia was either mild (38.9%) or moderate (16.7%) or severe (2.8%) at one month after treatment, and it was mild for 38.9% of the patients, while 55.6% did not show this symptom. At three months, only 13.9% of patients still had mild symptoms. Dyspareunia at one month was resolved in 59.57% of the cases (z=-2.840; p=0.005) and in 66.66% of the cases at three months (z=-3.874; p<0.001).
A volumetric reduction of the uterus and nodules can be seen after UAE. In this study, the uterine volume decreased significantly at one month and three months, respectively, compared to the initial measurement. The mean values were 269.6982 at one month, respectively 217.7972 at three months, with an average difference of 51.90±85.41, for the confidence interval of 95% (22.99%; 80.80%), with p=0.001. The initial and the 3-month mean values were 294.0286 and 211.8307, respectively, with an average difference of 82.19±119.17, for the confidence interval of 95% (24.75%; 139.63%), with p=0.008. For the first month, mean uterine volumes recorded a negative variation of -19.24% (51.91 cm³), from an average preembolization volume of 269.69±152.94 cm³ (extremes: 21.91-635.85) at an average volume per one month of 190.05±123.60 cm³ (extremes: 21.26-491.72), recording a downward trend (test t for pair samples; p-value=0.001; <0.05); the variation at three months was still negative, -42.36% (82.19 cm³) at 211.83±129.80 cm³ (extremes: 21.59-455.51) (test t for pairs, p-value=0.008; <0.50). The reduction in uterine volumes was found in 88.88% of the cases (32 patients out of 36) at one month and in 84.21% (16 patients) at three months of the 19 evaluated patients. In terms of volumetric reduction of nodules, one month after UAE the reduction was encountered in 88.88% of the patients (32 out of 36) and in 89.47% of the patients evaluated at three months (17 out of 19). The average volume for dominant nodule was 75.3732 cm3 initially, 56.2844 cm3 at one month, and 37.8728 cm3 at three months. The nodule volume decreased significantly at one month and at three months, respectively, compared to the initial measurement. For the 95% confidence interval, we had p=0.014 for the first pair and p=0.049 for the second pair. For the first month, mean nodule volumes recorded a negative variation of -25% (19.08 cm³), from an average pre-embolization volume of 75.37±101.28 cm³ (extremes: 3.77-523.60) to an average volume at one month of 56.28±91.94 cm³ (extremes: 2.67-518.10), recording a downward trend (t test for pair samples; p-value=0.014; <0.05); the three-month variation was negative at -42.93% (28.49 cm³) at 37.87±48.57 cm³ (extremes: 2.12-186.83) (t test for pair samples; p-value=0.049; <0.50).
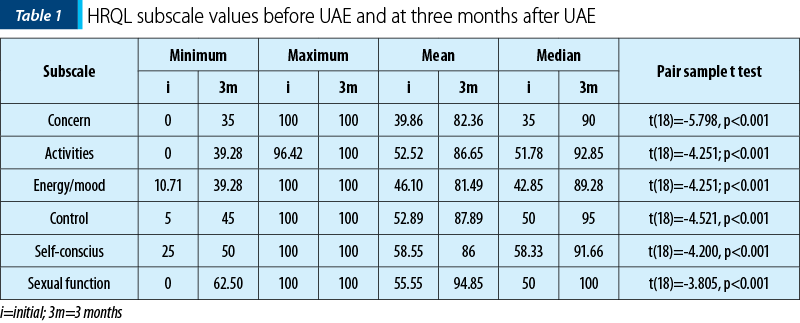
To assess the improvement in the daily life, we used the uterine fibroid symptoms and health-related quality of life questionnaire (UFS-QOL). The queries were applied to the patients before the procedure and at three months after the procedure. The baseline mean Ufs-QoL was 52.69±20.43, with a maximum of 81.25 and a minimum of 6.25, the questionnaire being applied to 36 patients. At three months, the average was 15.62±11.41, with a minimum value of 0 and a maximum of 37.5. The difference was statistically significant (p<0.001). The baseline mean HRQL was 49.78±21.37, with a maximum of 93.96 and a minimum of 13.79, the questionnaire being applied to 36 patients. At three months, the average was 85.24±15.62, with a minimum of 47.41 and a maximum of 99.13. The pair samples t test was applied to determine the relationship between the initial values of each of the subscales of the scores and the values three months after treatment. It shows the presence of a statistically significant relationship in each subscale (Table 1).
Discussion
According to the literature, the diagnosis of uterine myomas happens randomly in routine controls, and in these cases we refer to asymptomatic myomas, or due to symptomatology, manifested mainly by abnormal bleeding. In the study group, out of the 36 patients initially evaluated, 35 patients experienced abnormal bleeding. They also presented associated symptoms such as urinary disorders, pelvic discomfort and transit modification. The data obtained in the two stages regarding various symptoms can be compared with those from literature. However, the existence of a larger group of patients can lead to more accurate results which better outline the effect of UAE. As noted in literature, after UAE, the uterus reduces its volume and the vascularity modifies. All these modifications lead to a certain improvement of the quality of life. As with any other pathology, any treatment follows two components – healing and improving the quality of life. Some of the treatments, although they do not heal the underlying disease, improve their symptoms, prevent progression of the disease and improve the quality of life. Thus, we notice a positive evolution of the results and a statistically significant improvement in the quality of life, this being perhaps the most important in a benign pathology.
Conclusions
UAE is an efficient therapy for uterine fibroids, reducing symptomatology, the uterine volume and the nodule volume. Improving symptomatology due to the fibroid uterus leads to an increase in the quality of life in all its aspects. The use of quality of life questionnaires allowed a quantification of the patient’s symptomatology and well-being. UAE has a major impact on the quality of life, improving it significantly both at one and at three months.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Walker WJ1, Barton-Smith P. Long-term follow up of uterine artery embolisation – an effective alternative in the treatment of fibroids. BJOG. 2006; 113(4):464-8.
- Keung JJ, et al. Uterine artery embolization: A review of current concepts. Best Pract Res Clin Obstet Gynaecol. 2018; 46:66-73.
- Manyonda IT, Bratby M, Horst JS, Banu N, Gorti M, Belli AM. Uterine artery embolization versus myomectomy: impact on quality of life – results of the FUME (Fibroids of the Uterus: Myomectomy versus Embolization) Trial. Cardiovasc Intervent Radiol. 2012; 35(3):530-6.
- Goodwin SC, Bradley LD, Lipman JC, Stewart EA, Nosher JL, Sterling KM, Barth MH, Siskin GP, Shlansky-Goldberg RD; UAE versus Myomectomy Study Group. Uterine artery embolization versus myomectomy: a multicenter comparative study. Fertil Steril. 2006; 85(1):14-21
- Siskin GP, Shlansky-Goldberg RD, Goodwin SC, Sterling K, Lipman JC, Nosher JL, Worthington-Kirsch RL, Chambers TP; UAE versus Myomectomy Study Group. A prospective multicenter comparative study between myomectomy and uterine artery embolization with polyvinyl alcohol microspheres: long-term clinical outcomes in patients with symptomatic uterine fibroids. J Vasc Interv Radiol. 2006; 17(8):1287-95.
- Razavi MK, Hwang G, Jahed A, Modanlou S, Chen B. Abdominal myomectomy versus uterine fibroid embolization in the treatment of symptomatic uterine leiomyomas. Am J Roentgenol. 2003; 180(6):1571-5.
- Mara et al. Midterm clinical and first reproductive results of a randomized controlled trial comparing uterine fibroid embolization and myomectomy. Cardiovasc Intervent Radiol. 2008; 31(1):73–85.
- Ruuskanen A et al. Uterine artery embolisation versus hysterectomy for leiomyomas: primary and 2-year follow-up results of a randomised prospective clinical trial. Eur Radiol. 2010; 20(10):2524-32.
- Katsumor TM, Kasahara T, Akazawa K. Long-term outcomes of uterine artery embolization using gelatin sponge particles alone for symptomatic fibroids. AJR. 2006; 186:848-54
- Jun F, Yaminl L, Yushunl Z, Ujuan W, Xingyel V, Hao Q, Wenli G. Effect of selective uterine artery embolization on symptomatic uterine fibroids. J Med Colleg PLA. 2009; 24:346-53
- Pron G, Mocarski E, Bennett J, Vilos G, Common A, Zaidi M, Sniderman K, Asch M, Kozak R, Simons M, Tran C, Kachura J. Tolerance. hospital stay, and recovery after uterine artery embolization for fibroids: the Ontario uterine fibroid embolization trial. J Vasc Interv Radiol. 2003; 14(10):1243-50
- Mirsadree S, Tuite D, Nicholson A. Uterine artery embolization for ureteric obstruction secondary to fibroids. Cvlr. 2008; 31(6):1094-9.
- Scheurig-Muenkler C, Koesters C, Powerski MJ, Grieser C, Froeling V, Kroencke TJ. Clinical long-term outcome after uterine artery embolization: sustained symptom control and improvement of quality of life. J Vasc Interv Radiol. 2013; 24(6):765-71.
- Sandberg EM, Tummers FHMP, Cohen SL, van den Haak L, Dekkers OM, Jansen FW. Reintervention risk and quality of life outcomes after uterine-sparing interventions for fibroids: a systematic review and meta-analysis. Fertil Steril. 2018; 109(4):698-707.
- Smith WJ, Upton E, Shuster EJ, Klein AJ, Schwartz ML. Patient satisfaction and disease specific quality of life after uterine artery embolization. Am J Obstet Gynecol. 2004; 190(6):1697-703.
- Dumitraşcu MC, Horhoianu V. Embolizarea arterelor uterine. Ed. Univ. “Carol Davila” Bucureşti, 2008; ISBN: 978-973-708-285-5.
- Ganguli S, Stecker MS, Pyne D, Baum RA, Fan Cm. Uterine artery embolization in the treatment of postpartum uterine hemorrhage. J Vasc Interv Radiol. 2011; 22(2):169-76.
- Spies JB, Ascher SA, Roth, AR, Kim J, Levy EB, Gomez-Jorge J. Uterine artery embolization for leiomyomata. Obstet Gynecol. 2001; 98:29-34.
- Hald K, Kløw NE, Qvigstad E, Istre O. Laparoscopic occlusion compared with embolization of uterine vessels: a randomized controlled trial. Obstet Gynecol. 2007; 109(1):20–7.
- Hehenkamp WJ, Volkers NA, Donderwinkel PF, de Blok S, Birnie E, Ankum WM, Reekers JA. Uterine artery embolization versus hysterectomy in the treatment of symptomatic uterine fibroids (EMMY trial): peri- and postprocedural results from a randomized controlled trial. Am J Obstet Gynecol. 2005; 193(5):1618-29.