Introduction. In the project “Fetal Neurosonography - Evaluating the potential of 3D ultrasound in the routine screening” we analyzed the possibilities of evaluating the corpus callosum through 2D and 3D ultrasound in routine investigations. Methods. Our work encompasses two studies: a prospective study regarding obtaining a correct image of the corpus callosum with two-dimensional (2D) and three-dimensional (3D) ultrasound on two levels of training (beginner and advanced sonographer) and a retrospective study that targeted the ability to obtain an image of the corpus callosum from a three-dimensional (3D) volume selected from our data base using a computer software. Results. In our prospective study we obtained a correct image of the corpus callosum in 65.38% with 2D ultrasound and 82.69% with 3D ultrasound at the beginner level, and respectively 82.69% and 94.23%for the advanced level. In the retrospective study, the off line manipulation of the volumes showed similar results with values of 81% and 94%. Conclusion. 3D ultrasound allows an easier approach for demonstrating the normal corpus callosum especially for beginners. Introducing the 3D approach in the routine fetal ultrasound will encourage sonographers to obtain an image of the corpus callosum in the difficult cases, where the position of the fetus does not allow us to obtain a median section with 2D ultrasound.
Evaluarea corpului calos fetal în examinarea de rutină - ecografie 2D versus ecografie 3D
Imaging the fetal corpus callosum in the routine examination – 2D versus 3D ultrasound
First published: 15 aprilie 2015
Editorial Group: MEDICHUB MEDIA
Abstract
Rezumat
Introducere. În cadrul proiectul „Neurosonografia fetală - evaluarea potenţialului ecografiei 3D în examinarea de rutina” am analizat posibilităţile evaluării corpului calos fetal cu ajutorul ecografiei 2D şi 3D în examinarea de rutină. Metoda. Lucrarea noastră cuprinde două studii: unul prospectiv privind obţinerea unei imagini corecte a corpului calos prin ecografie bidimensională (2D) şi tridimensională (3D), pe două niveluri de pregătire în examinarea ecografică (începători şi avansaţi) şi un studiu retrospectiv, care a urmărit abilitatea în obţinerea unei imagini corecte a corpului calos dintr-un volum 3D, ales din baza de date a clinicii folosind un program de calculator. Rezultate. În studiul prospectiv am obţinut o imagine corectă a corpului calos în 65,38% din cazuri cu ecografia 2D şi de 82,69% cu ecografia 3D la nivelul începători şi, respectiv, 82,69% şi 94,23% la nivelul avansaţi. În studiul retrospectiv, prelucrarea off-line a volumelor a arătat rezultate similare, cu valori de 81% şi 94%. Concluzie. Ecografia 3D permite o demonstrare mai uşoară a corpului calos, în special pentru examinatorii începători. Introducerea ecografiei 3D în examinarea fetală de rutină va încuraja examinatorii în obţinerea unei imagini a corpului calos şi în cazurile dificile, acolo unde poziţia fetală nu permite obţinerea unei secţiuni mediane cu ecografia 2D.
Introduction
In the project “Parteneriat strategic pentru creşterea calităţii cercetării ştiinţifice din universităţile medicale prin acordarea de burse doctorale şi postdoctorale - DocMed.net_2.0”, ID Proiect 136893 - Fetal Neurosonography – Evaluating the potential of 3D ultrasound in the routine screening”, we analyzed the possibilities of evaluating the corpus callosum through 2D and 3D ultrasound in routine investigations.
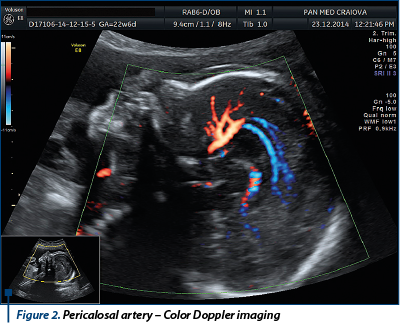
The corpus callosum is a telencephalic structure composed mainly of white matter, which unites the left and right hemispheres, being the main interhemispheric communication line. It has four parts: rostrum, genu, body and splenium.It is initially a compact structure but it grows considerably in the second trimester of pregnancy when its four parts can be distinguished forming the ceiling of the third ventricle. The first fibers that unite the two hemispheres were showed on histology studies to appear at around 13 weeks, but the complete development demonstrated on imaging studies was obtained at 18-19 weeks; imaging of its partial development (rostrum and genu) has been described on MRI images at 15 weeks(1). The direction of development is from anterior to posterior, so any error will affect predominantly the body and the splenium. The intrauterine evaluation of the corpus callosum has the purpose to diagnose or exclude the complete or partial agenesis, with transabdominal or transvaginal ultrasound using two-dimensional (2D) or three-dimensional ultrasound (3D). The corpus callosum agenesis has an incidence of 0.5% in the general population and 2-3% in the population with neuro-psychiatric disabilities - pediatric studies following children with agenesis of the corpus callosum showed progressive intellectual deterioration and association with different types of psychosis(2,3,4,5). Complete agenesis of the corpus callosum associates with important distortion of the cerebral architecture with moderate ventriculomegaly associated to a neuronal migration disorder predominantly at the occipital level (colpocephaly)(2,6,7,8,9). Other aspects include a larger distance between the anterior horns, ascension of the third ventricle, cysts or lipomas on the median line, absence of the pericalosal artery - demonstrable with Color or Power Doppler(2,10). Diagnosis of partial agenesis of the corpus callosum is far more difficult, transversal sections being frequently useless - for demonstrating a defect (which is more often a lack of development of the posterior portion) a median section is necessary. Using Color Doppler will show an incomplete and deformed trajectory of the pericalosal artery(2,11).
Methods
We realized a prospective study that started in 1.07.2014 and ended in 30.11.2014 - it monitored the evaluation of the corpus callosum in patients that presented in the Prenatal Diagnosis Unit, SCJU Craiova, for the anomaly scan. The cohort had 52 cases of singleton low-risk pregnant women with gestational ages between 19 and 25 weeks. Our research was approved by the University Ethical Committee and all patients provided written informed consent to participate in the study. Three cases were excluded from the study due to the impossibility to obtain a good quality fetal brain volume because of extreme and prolonged fetal movement at the moment of the examination.
All examinations were performed on Voluson 730 PRO and Voluson E8 ultrasound machines (GE Healthcare, Kretz Ultrasound, Zipf, Austria) using transabdominal (RAB4-8) and transvaginal (RIC 5-9) volumetric probes. Cases were scanned by four examiners gruped as it follows: two experienced examiners (AC & FT), two beginners (CC & AN). The Advanced examiners had a certificate of competence in obstetric sonography with more than 5 years experience. The beginners are residents in training who had completed the first part of the ultrasound training. The neutral observer was the head of the obstetrics department. We analyzed the ability to obtain a correct image of the corpus callosum with three methods (both transabdominal and transvaginal images were allowed):
-
Obtaining a 2D image
-
Obtaining an image of the pericalosal artery with Color Doppler
-
Obtaining an image of the corpus callosum from a volume acquired during the examination.
The techniques used in our study were based on recommendations of the International Society of Obstetrics and Gynecology(12,13,14).
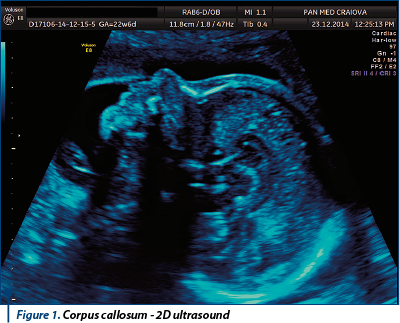
The 2D examination of the corpus callosum starts from the sagital plane with the fetal profile - with moderate lateral move of the probe, through the anterior fontanelle we obtained the median plane with the entire corpus callosum. Also, starting from the coronal image of cavum septum pelucidum and anterior horns, rotating the transducer 90 degrees, we obtained the median plane with a complete image of the corpus callosum. An additional 2D image that is useful in the demonstration of a normal corpus callosum is the trajectory of the pericalosal artery. After obtaining the median plane as described by the 2D examination, we used Color Doppler (or HD-flow) to visualize the pericalosal artery. The recommended PRF (pulse repetition frequency) was 20-40 cm/sec., but Color map, gain and Doppler region of interest were left for each examiner to decide.
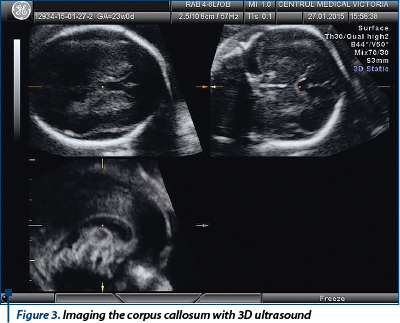
For the 3D ultrasound the following standard protocol was designed:
-
We set the axial section in plane A.
-
We set the axial plane to obtain the standard image with cavum septum pellucidi, thalamus and the posterior horns of the lateral ventricles.
-
We set the reference dot at the level of the cavum septum pellucidi.
-
In the C plane we will obtain the corpus callosum.
The criteria for the 3D volumes were an angle between 40 and 60 degrees with the inclusion of the entire cerebral structure. Recommended but not compulsory was a quality of high 2 or max. Use of volume contrast imaging (VCI) or tomographic ultrasound imaging (TUI) was allowed.
Parallel with our prospective study we analyzed a retrospective evaluation of the corpus callosum from our volume data base - a neutral evaluator (NC) selected 100 cases with the necessary quality criteria. The 100 cases were shared similar to the prospective study by two groups of examiners: experienced (AC & FT) and beginners (CC & AN) using 4D view software. A neutral evaluator analyzed the images obtained by the four members of the team and classified them in satisfactory and unsatisfactory/non-interpretable image.

Statistical analysis was performed using Microsoft Excel (Microsoft Corp., Redmond, WA, USA), together with the XLSTAT add-on for MS Excel (Addinsoft SARL, Paris, France) and IBM SPSS Statistics 20.0 (IBM Corporation, Armonk, NY, USA) for processing the data. Data was recorded using Microsoft Excel files. Data Processing - the graphic representation of the study data was performed in Excel, using Pivot Tables, Functions-Statistical, Charts and Data Analysis module. Statistical tests (Z test for proportions, Fisher exact test) were performed using the XLSTAT add-on or SPSS. Z test for proportions is used to investigate the statistical significance of the difference between a theoretical frequency f (in a population) and the observed frequency p in a representative sample for a qualitative or binary variable, or to compare the frequencies calculated on two randomized samples, independently extracted from two different populations. The test can be applied if the number of observations in the sample group, n, is large enough (n • p, n • (1-p)>10), or if the two samples have a sufficient number of subjects (n1, n2> 30).The Chi square test (c2) is a statistical test that shows if there is a connection (association or influence) between two factors. It is used to interpret incidence tables generated by cross tabulation of 2 factors monitored in the study. If, for the analyzed incidence table, the probable frequency is less than 1, or if more than 20% of probable frequencies are less than 5, it is recommended to use Fisher’s exact test when its application is allowed (small groups with <100 cases, small incidence tables, with less than 10 cells, e.g. 2x2 - 5x2, 3x3).We used both Z test and Fisher exact test on our data, to double check with two different methods if the results show significant differences between the compared categories.
Results
Prospective study:
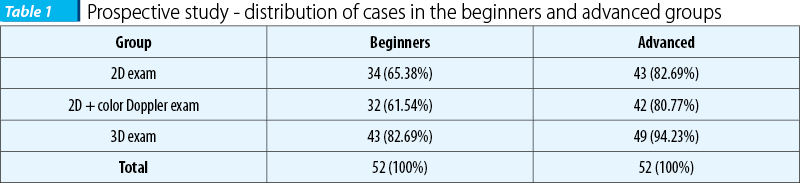
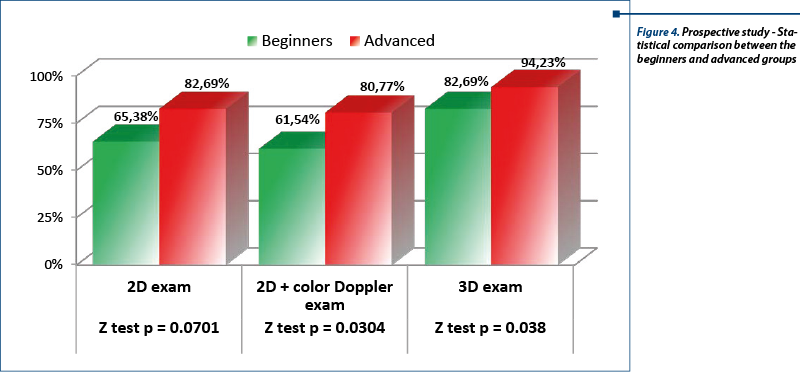
We analyzed the images on examination groups – beginners versus advanced sonographers. In the beginner group a correct image was obtained in 65.38% with 2D and in 82.69% with tridimensional ultrasound. Color ultrasound allowed demonstration of a normal pericalosal artery in 61.54% of cases probably because of difficulties in selecting the right Doppler parameters and more difficult positions of the fetus. In the advanced group we had a 82.69% correct image percentage, with a detection of the pericalolosal artery of 80.77%. Three-dimensional ultrasound had better results for both beginners and advanced groups, the latter having a percentage of 94.23%. The difference between beginners and advanced was statistically significant for this group of 52 cases regarding the 2D exam, the p values for both Fisher’s exact test (p=0,036) and for Z test for proportions (p=0.044) being smaller that the cut-off value, 0.05. The difference is even greater for 2D+ color Doppler (Fisher p=0.025, Z test p=0.030). The 3D exam showed a difference between the 2 groups of investigators, but, surprisingly, it wasn’t statistically significant for this group (Fisher p=0.061, Z test p=0.066); however, it could prove significant if a larger sample of cases is used, because the p values were not larger than 0.05. Comparing, separately for beginners and advanced investigators, the differences between the 3 types of examinations, we found significant differences only between 2D+Doppler and 3D, for both groups of investigators, while 2D vs. 2D+Doppler showed almost no difference for both groups. 2D vs. 3D showed a statistically significant for the beginner group (Fisher p=0.036, Z test p=0.044), and a not significant difference for the advanced group (Fisher p=0.061, Z test p=0.066); the latter could prove significant if a larger sample of cases is used, because the p values were not larger than 0.05.
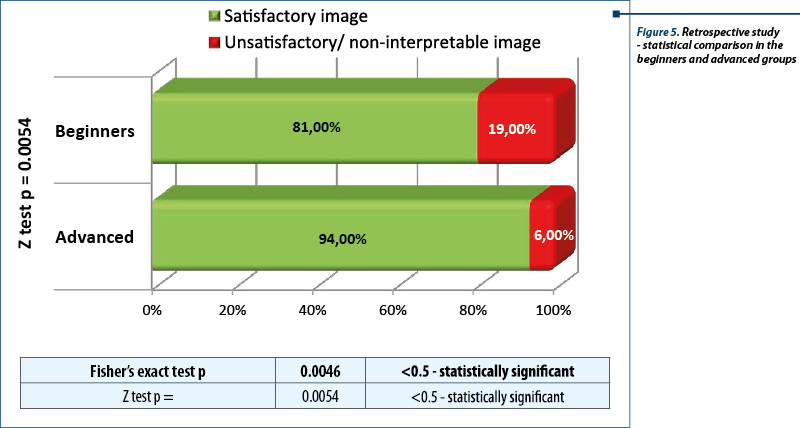
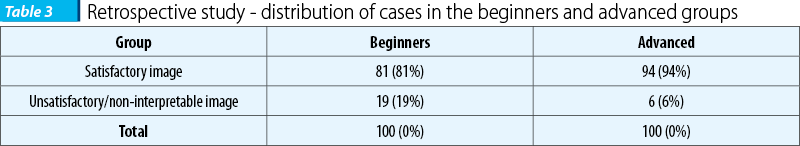
Retrospective study:
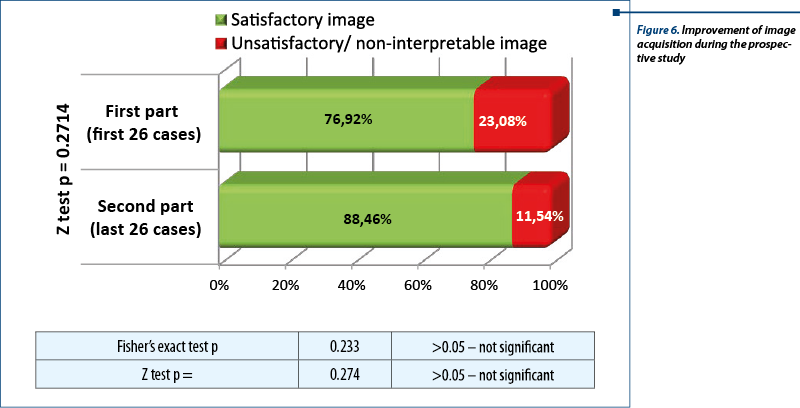
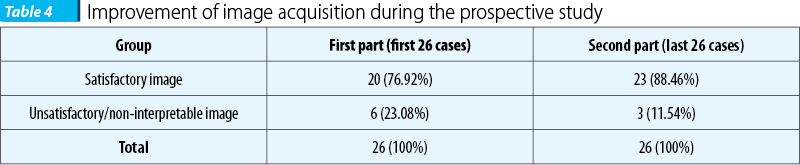
The images from the volume data base were analyzed by the neutral observer (NC), without any information regarding from which group of examiners the image belonged to. Images obtained were saved in jpeg format and were classified in satisfactory and unsatisfactory or non-interpretable. A correct section was obtained in 81% in the beginners group and in 94% in the advanced group. We should also mention the role of the retrospective study in acquiring the dexterity necessary to manipulate the ultrasound volumes. As the studies took place, in parallel beginners benefited from the supplementary experience of using the 4D view software, showing an improvement in the quality of the image in the second part of the study. However, even if the performance of the investigators in training improved during the prospective study because of the image analysis carried out in the retrospective study, the difference is not statistically significant.
Discussions
Two-dimensional ultrasound is now the gold standard in imaging the central nervous system. The quality of the image is superior to the image recreated from three-dimensional volumes and allows real-time, with or without Doppler, examination; it has no need for expensive volumetric probes or additional software. Its main disadvantage in the fetal neurosonography is the need for a good fetal position - in the case of the corpus callosum it has to allow a median section. Obtaining it may be time consuming or necessitate fetal manipulation that is difficult for the beginners and not always desirable. In our study examiners were asked not to manipulate the fetus in order to avoid additional bias (beginners will find it difficult) and to avoid undesirable incidents created by an incorrect or brutal maneuver.
The benefits of 3D ultrasounds in the examination of the fetal nervous system consist in the possibility to evaluate in three orthogonal planes simultaneously, which is impossible with 2D ultrasound. Additional software like VCI (volume contrast imaging) allows us to obtain a slice from a volume of a thickness predefined by the user (eq. 2 mm, 5 mm, etc). The result is an image with a lower image noise and superior contrast to the 2D or native 3D image. TUI (tomographic ultrasound imaging) is a new method to display the image from a 3D volume allowing viewing of several slices of a predefined section simultaneously. The two software were used almost exclusively by experienced sonographers, hence the better images and the greater speed in acquiring the image. Regarding the disadvantages of the 3D ultrasound in the examination of the corpus callosum the following aspects are worth mentioning: 1. it is very difficult to differentiate between the corpus callosum and the inferior cavum septum pellucidi - only with optimal visualization the corpus callosum can be differentiated as a sonolucent stripe located between cavum septum pellucidi and the superior midline; 2. shadowing of the posterior part is possible in difficult positions(14,15). Other studies also grant importance to the three-dimensional (3D) ultrasound of the fetal nervous system as a way to reduce dependence on operator skill - an algorithm based on Omni View technology used 3D volumes to obtain all the standard planes including the visualization of the corpus callosum(16).
Other aspects that are worth mentioning are the reason we concentrated our attention on the corpus callosum - first the corpus callosum is not on any standard plane on routine second trimester examination, second, the pathology associated with anomalies of the corpus callosum have great impact on the child’s intellectual development and parents should benefit from a prenatal diagnosis. In a study by Ghi and col. 50% of patients facing a diagnosis of partial agenesis of the corpus callosum opted for termination of pregnancy(17).
Conclusion
3D ultrasound allows an easier approach for demonstrating the normal corpus callosum especially for beginners. Introducing the 3D approach in the routine fetal ultrasound will encourage sonographers to obtain an image of the corpus callosum in the difficult cases, where the position of the fetus does not allow us to obtain a mid-sagital section with 2D ultrasound. However, for the moment, if an anomaly of the corpus callosum is suspected on a 3D volume it is necessary for the patient to benefit from an expert 2D ultrasound preferably transvaginal, in order to exclude or confirm a diagnosis.
Acknowledgement: The research/the study/work was (partially) funded by POSDRU grant no. 159/1.5/S/136893 grant with title: “Parteneriat strategic pentru creşterea calităţii cercetării ştiinţifice din universităţile medicale prin acordarea de burse doctorale şi postdoctorale – DocMed.Net_2.0”.
Bibliografie
2. Pilu G, Sandri F, Perolo A, Pittalis MC, Grisolia G, Cochi G. et al. Sonography of the fetal agenesis of the corpus callosum: a survey of 35 cases. Ultrasound obstet Gynecol. 1993; 3(5):318-29.
3. Gupta JK, Lilford RJ. Assesment and management of fetal agenesis of the corpus callosum. Prenat Diagn. 1995;15(4):301-12.
4. Moutard ML, Kiefer V, Feingold J et al. Agenesis of corpus callosum: prenatal diagnosis and prognosis. Chids Nerv System. 2003; 19(7-8):471-6.
5. Lewis SW, Revely MA, David AS, Ron MA. Agenesis of the corpus callosum and schizophrenia: a case report. Psychol Med. 1998; 18(2):341-7.
6. Bennett GL, Bromley B, Benaceraf BR. Agenesis of the corpus callosum: prenatal detection usually is not possible before 22 weeks of gestation. Radiology. 1996; 199(2):447-40.
7. Filly RA, Cardoza JD, Goldstein RB, Barkovich AJ. Detection of fetal central nervous system anomalies: a practical level of effort for routine sonogram. Radiology. 1989;172(2):403-8.
8. Patel M, Filly AL, Hersh DR, Golstein RB. Isolated mild fetal cerebral ventriculomegaly: clinical course and outcome. Radiology. 1994; 192(3):759-64.
9. Goldstein RB, La Pidus AS, Filly RA, Cardoza J. Mild lateral cerebral ventricular dilatation in uter: clinical significance and prognosis. Radiology. 1990; 176(1):237-42.
10. Mulligan G, Meier P. Lipoma and agenesis of the corpus callosum with associated choroid plexus lipomas. In utero diagnosis. J Ultrasound Med. 1989;8(10):583-8.
11. Volpe P, Palladini D, Resta M, et al. Characteristics, associations and outcome of partial agenesis of the corpus callosum in the fetus. Ultrasound Obstet Gynecol 2006; 27(5):509-16.
12. Youssef A, Ghi T, Pilu G. How to image the fetal corpus callosum Ultrasound Obstet Gynecol 2013; 42:718–20.
13. ISUOG Education Committee Sonographic Examination of the fetal central nervous system: guidelines for performing the ‘basic examination’ and the ‘fetal neurosonogram Ultrasound Obstet Gynecol 2007; 29:109–16.
14. Pilu G, Ghi T, Carletti A, Segata M, Perolo A, Rizzo N. Three-dimensional ultrasound examination of the fetal central nervous system. Ultrasound Obstet Gynecol. 2007; 30: 233–45.
15. Malinger G, Lerman-Sagie T, Vinals T. Three-dimensional sagittal reconstruction of the corpus callosum: fact or artifact? Ultrasound Obstet Gynecol. 2006; 28:742–3.
16. Rizzo G, Capponi A, Pietrolucci ME, Capece A, Aiello E, Mammarella S, Arduini D. An algorithm based on OmniView technology to reconstruct sagittal and coronal planes of the fetal brain from volume datasets acquired by three-dimensional ultrasound Ultrasound Obstet Gynecol. 2011; 38:158–64.
17. Ghi T, Carletti A, Contro E et al. Prenatal diagnosis and outcome of partial agenesis and hypoplasia of the corpus callosum. Ultrasound Obstet Gynecol. 2010; 35:35–41.
Articole din ediţiile anterioare
Semne ecografice timpurii în agenezia de corp calos
Obiective. Deşi agenezia de corp calos este un diagnostic stabilit în trimestrul al doilea, este un deziderat să scădem vârsta gestaţională pentru ...
Extinderea examinării standard a sistemului nervos central fetal la ecografia de trimestrele doi şi trei
Protocolul de bază asigură diagnosticarea majorităţii anomaliilor sau cel puţin sesizarea prezenţei unei anormalităţi şi direcţionarea cazului ...