The objective of this paper was to analyze the metabolic model for the monitoring and management of gestational diabetes. This is a descriptive, retrospective and observational study, based on the medical records from the database of the “Alessandrescu-Rusescu” Institute for Maternal and Child Health, Bucharest. There were included 157 patients who showed up for consult in every trimester of pregnancy. Fat accumulation during pregnancy is variable and may depend on the woman’s pre-pregnancy metabolic status and other lifestyle variables such as diet and physical activity. Pregnancy represents a critical period of growth, development and physiological change, providing an opportunity for early lifestyle intervention. The goal of identifying an effective lifestyle program for the gestational period that leads to healthy fetal development and subsequent normal weight offspring less likely to develop obesity and its comorbidities is unique and could mitigate the intergenerational cycle of obesity. The main objective in the management of obesity during pregnancy is prevention. Basically, apart from pre-conceptional weight loss in the management of obese pregnant women, glucose screening should be considered in obese women in early pregnancy to rule out undiagnosed pregestational diabetes.
The metabolic pattern for monitoring and management of gestational diabetes
Profilul metabolic pentru monitorizarea şi managementul diabetului gestaţional
First published: 30 martie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.39.1.2023.7781
Abstract
Rezumat
Obiectivul acestui studiu este analiza modelului metabolic în monitorizarea şi managementul diabetului gestaţional. Am realizat un studiu descriptiv, retrospectiv şi observaţional, utilizând baza de date a Institutului Naţional pentru Sănătatea Mamei şi Copilului „Alessandrescu-Rusescu”, Bucureşti. Am inclus 157 de parturiente, care au fost monitorizate în fiecare trimestru de sarcină. Curba ponderală în timpul sarcinii este variabilă şi poate depinde de statusul metabolic al pacientei anterior sarcinii, precum şi de alte variabile ce ţin de stilul de viaţă, precum dieta şi activitatea fizică. Sarcina reprezintă o perioadă critică, cu variaţii ale statusului ponderal şi fiziologice, ce conferă o oportunitate pentru a interveni precoce în privinţa stilului de viaţă. Un stil de viaţă optim în perioada gestaţională conduce la o dezvoltare fetală corespunzătoare şi ulterior la o greutate optimă a bebeluşilor, reducând astfel riscul de apariţie a obezităţii şi a comorbidităţilor, fapt ce poate iniţia ciclul intergeneraţional al obezităţii. Obiectivul principal în managementul obezităţii în sarcină este prevenţia. Practic, dincolo de scăderea ponderală din perioada anterioară sarcinii în managementul gravidei obeze, monitorizarea precoce a nivelului glucozei serice trebuie luată în considerare la pacientele obeze încă de la debutul sarcinii, pentru a exclude diabetul pregestaţional nediagnosticat.
1. Introduction
Globally, the prevalence rate of overweight or obesity between 1980 and 2013 increased by 27.5% for adults and by 47.1% for children, to a total of 2.1 billion individuals considered overweight or obese(1). These increases have been seen in both developed and developing countries. However, the prevalence of overweight and obesity is higher in developed countries than in developing countries at all ages. In developed countries, more men were considered overweight or obese than women; the opposite has been observed in developing countries(2). In the United States of America, obesity rates are 12.4% for boys under 20 years old, 31.7% for men with the age of 20 or older, 13.4% for girls younger than 20, and 33.9% for 20-year-old women or older. Prevalence rates increased between 1992 and 2002, but have stabilized ever since(1).
The World Health Organization (WHO) define normal weight as a Body Mass Index (BMI; weight [kg]/height [m]2) of 18.5-24.9, overweight as a BMI of between 25 and 29.9, and obesity as a BMI of 30 or higher(3).
A study from 2020 found obesity and maternal age to be the two most important factors independently affecting the risk of gestational diabetes(4). The study included 17,145 pregnant women who enrolled at 15 to 20 weeks of gestation from 1 August 2018 to 1 March 2019. A 2-hour 75 g oral glucose tolerance test (OGTT) was performed for each participant at 24-28 weeks of gestation. The study concluded that pre-pregnancy overweight and obesity, increased gestational BMI from conception to 15-20 weeks of gestation, and older age were associated with an increased risk of gestational diabetes.
A retrospective cohort study by Whitaker (2004) of more than 8400 children in the USA in the early 1990s reported that those children born to obese mothers (based on first-trimester BMI) had twice as likely chances of being obese by the age of 2 years old(5). If a woman had a BMI of 30 or more in the first trimester, the prevalence of childhood obesity (BMI greater than the 95th percentile based on CDC criteria) at ages of 2, 3 and 4 years old was 15.1%, 20.6% and 24.1%, respectively. This was between 2.4 and 2.7 times higher than the prevalence of obesity seen in children of mothers whose BMI was in the normal range (18.5-24.9). This effect was only slightly modified by birth weight.
Therefore, both pre-pregnancy maternal obesity and the presence of maternal diabetes may independently affect the risk of adolescent obesity in the offspring.
Maternal obesity is also a risk factor for fetal macrosomia.
2. Materials and method
The objective of this paper is to analyze the metabolic model for the monitoring and management of gestational diabetes. This is a descriptive, retrospective and observational study, based on the medical records from the database of the “Alessandrescu-Rusescu” Institute for Maternal and Child Health, Bucharest.
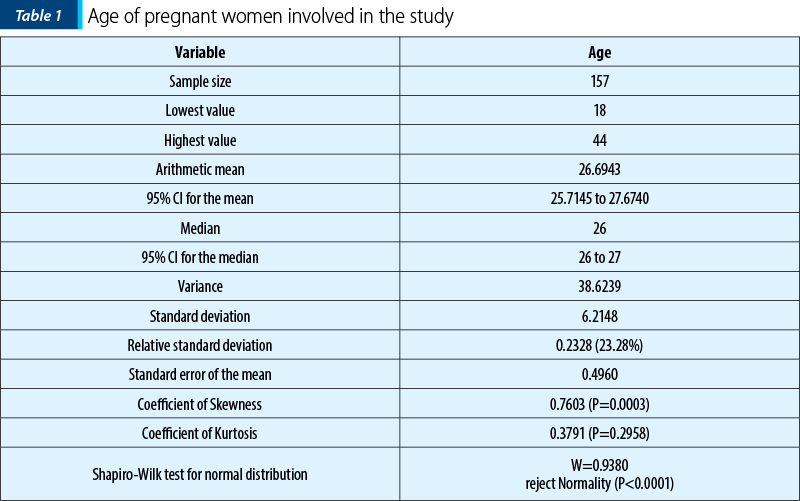
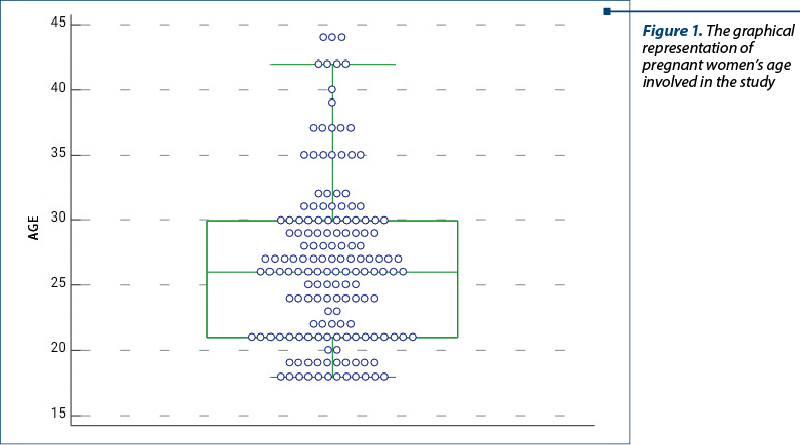
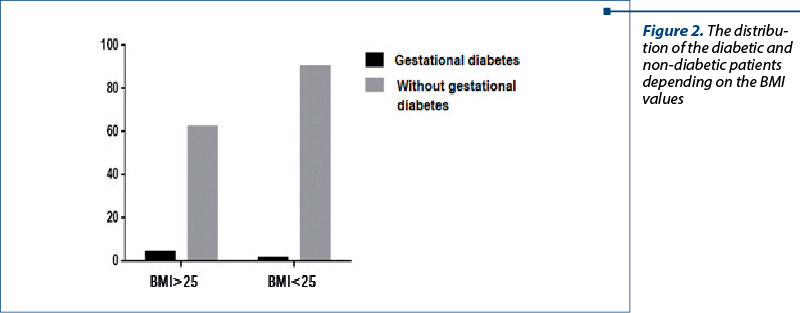
There were included 157 patients who showed up for consult in every trimester of pregnancy. All the patients had the minimal age of 18, and gave their written consent for enrolling in the study. There have been taken into consideration the demographical data (age), the anthropometric data (Body Mass Index, abdominal circumference), and a complete set of paraclinical data in order to assess which patients had a higher risk of developing gestational diabetes (GD) depending on BMI, and to monitor the differences in abdominal circumferences during all three trimesters of pregnancy regarding patients with diabetes as well as those who were non-diabetic.
The statistical analysis was conducted using GraphPad 8 and MedCalc 14.1.
3. Results and discussion
The study was conducted on 157 patients who were divided into two lots: A – 66 obese women who had their BMI higher than 25 kg/m2, and B – 91 normal weight women who had their BMI below 25 kg/m2.
Obesity is further characterized by BMI in class I (30-34.9), class II (35-39.9), and class III (greater than 40)(6).
Maternal obesity during pregnancy has been associated with adverse pregnancy outcomes, including hypertensive disorders of pregnancy, gestational diabetes and the need for surgical delivery(7). The risk of developing gestational diabetes for patients with the BMI higher than 25 is 5.5 times higher compared to patients whose BMI was lower than 25. The result is not statistically significant, but it should be taken into consideration.
A study from 2016 showed that maternal obesity is accompanied by maternal and fetal complications during and after pregnancy(8). The study revealed that the risks seem to increase with the degree of obesity. The study started from the premise that leptin plays a role in the development of obesity-related complications.
A study from 2019 showed that maternal obesity during pregnancy is associated with cardiovascular disease and mortality in the offspring(9). The study results showed that offspring of obese (BMI≥30 kg/m2) and overweight (BMI 25-29.9 kg/m2) mothers had an increased risk of type 2 diabetes compared to mothers with normal BMI, after adjusting for gestation when weight was measured, maternal history of pre-pregnancy diabetes, maternal history of hypertension, age at delivery, parity, socioeconomic status and offspring sex: HR 3.48 (95% CI; 2.33, 5.06) and HR 1.39 (1.06, 1.83), respectively.
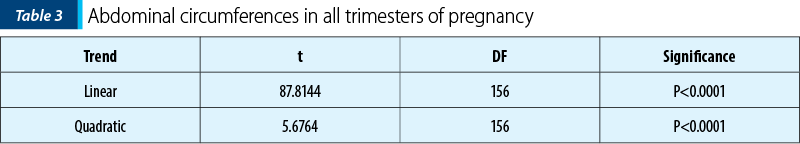
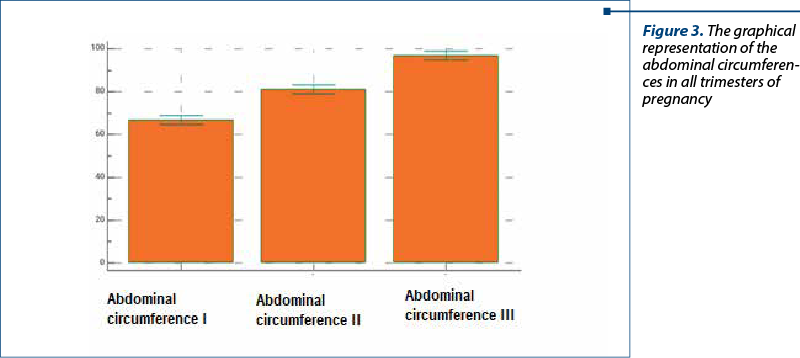
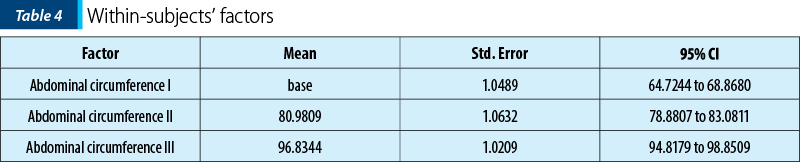
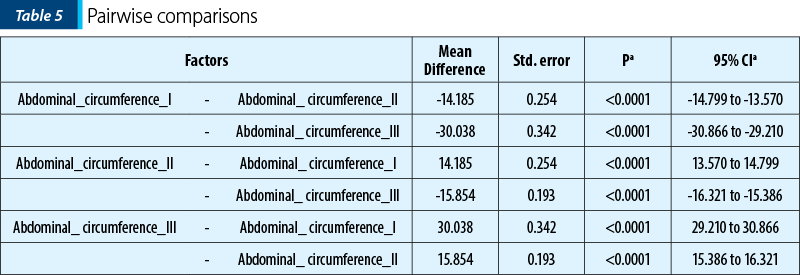
We applied the Bonferroni analysis method to illustrate the increase of the abdominal circumference values for all the three measurements performed during the three trimesters of pregnancy.
The average growth in the first and second trimesters is 14 cm, and the growth in the second and third trimesters is 15 cm. All the differences between the means are statistically significant, even though the linear or exponential trend (quadratic) is taken into consideration.
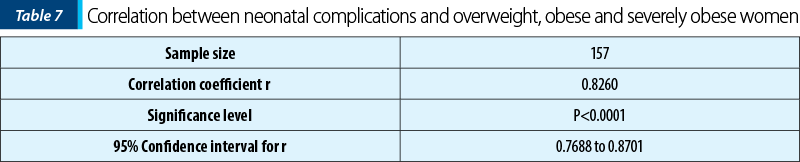
A study from 2011 aimed at estimating the association of maternal overweight and obesity on complications during pregnancy and childbirth in Denmark(10). The study revealed a significantly increased risk for a wide variety of pregnancy, birth and neonatal complications in overweight, obese and severely obese women.
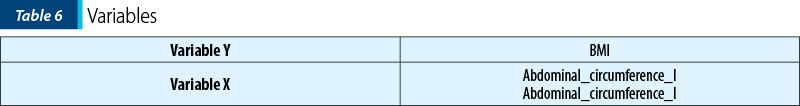
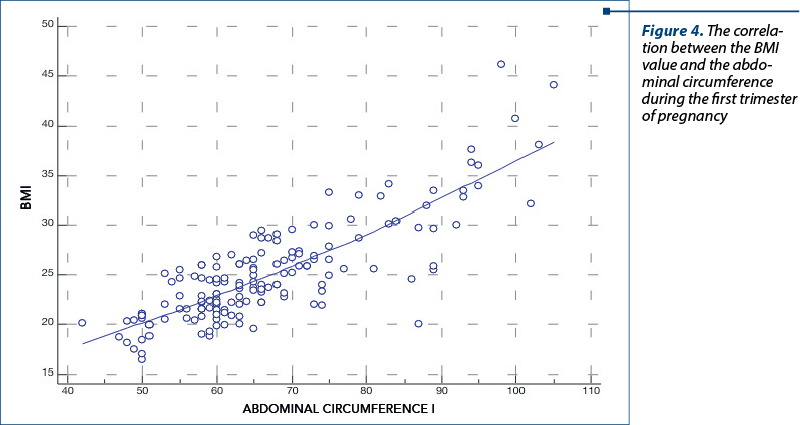
There is a directly proportional and statistically significant correlation between the BMI and the abdominal circumference during the first trimester of pregnancy (r=0.82).
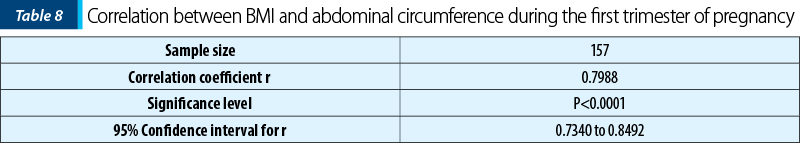
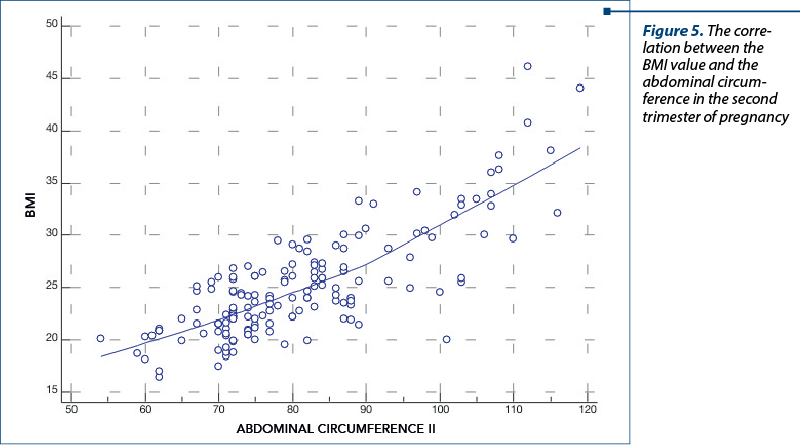
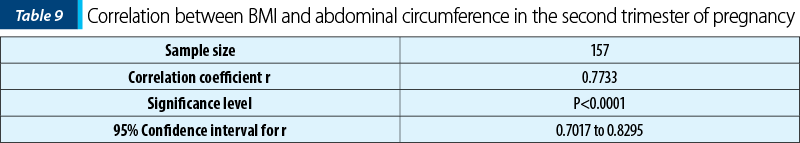
There is a directly proportional and statistically significant correlation between the BMI value and the abdominal circumference in the second trimester of pregnancy (r=0.79).
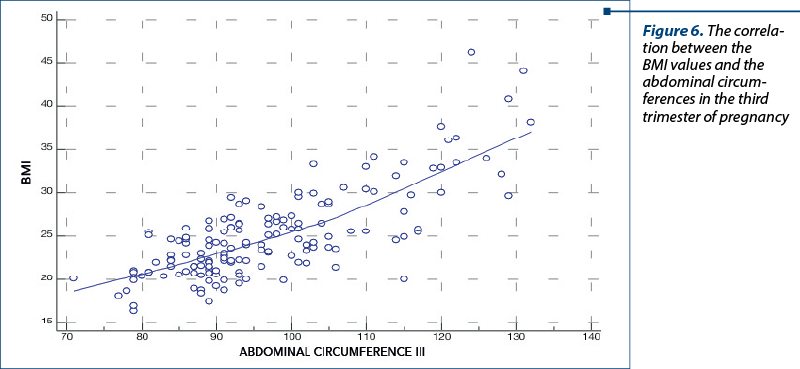
There is a directly proportional and statistically significant correlation between the BMI value and the abdominal circumference in the third trimester of pregnancy.
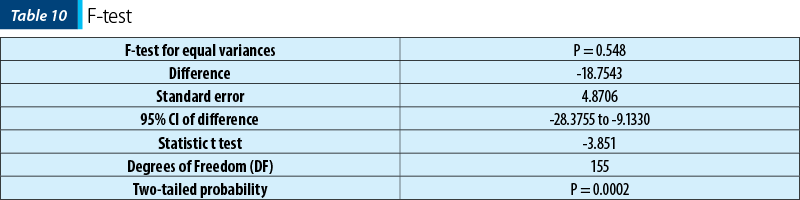
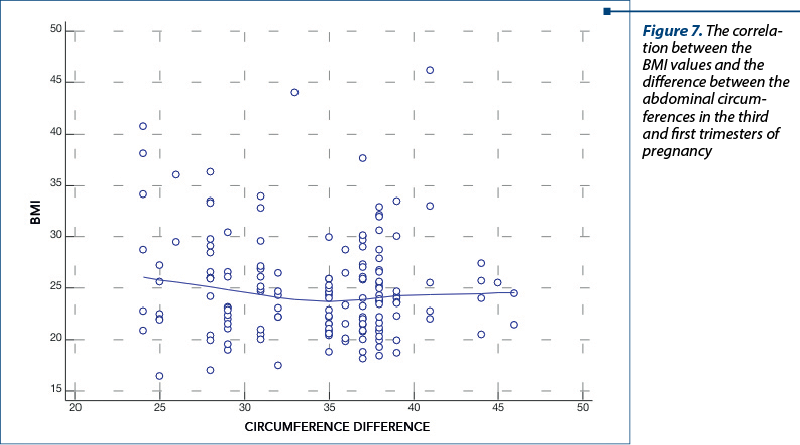
Although there seems to exist an inversely proportional variation trend between the BMI value and the abdominal circumference elevation curve, this difference is not statistically significant.
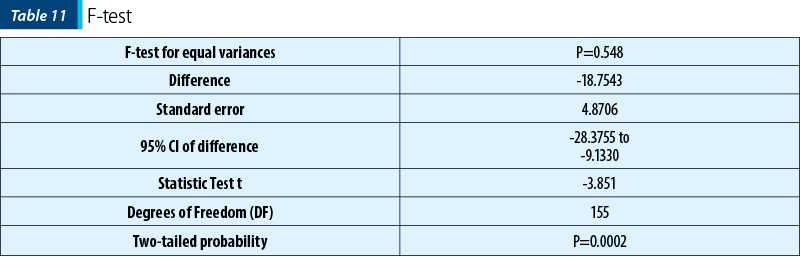
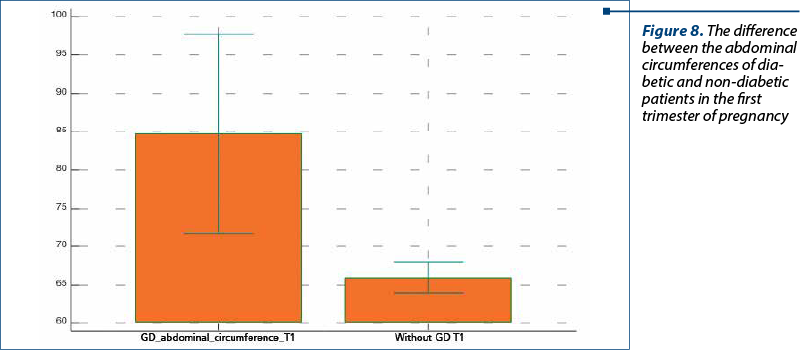
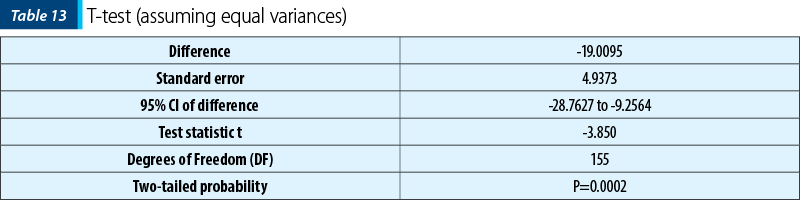
There is a statistically significant difference between the abdominal circumferences of diabetic patients in their first trimester of pregnancy (184.71 cm versus 65.96 cm; p=0.0002).
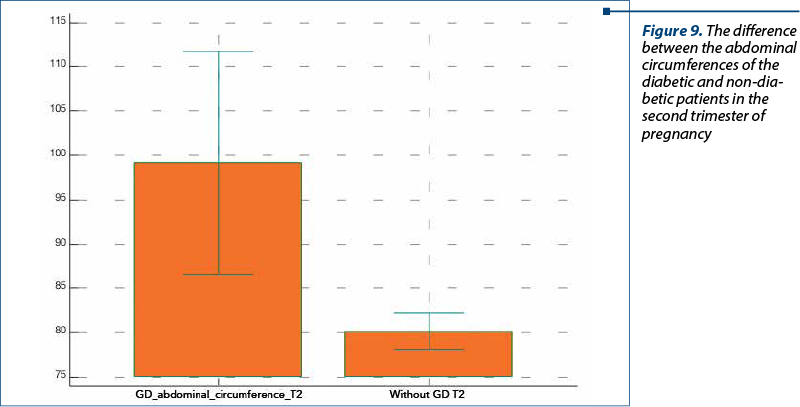
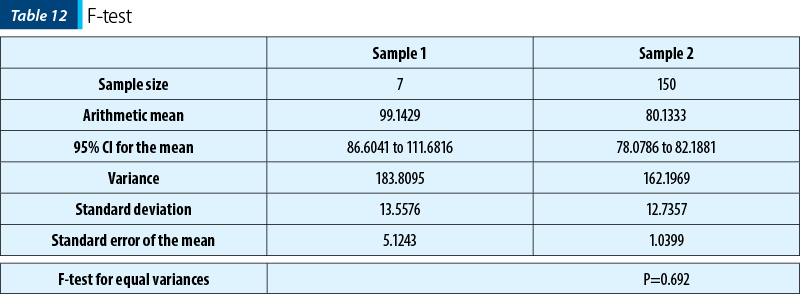
There is a statistically significant difference between the abdominal circumferences of diabetic patients in their second trimester of pregnancy (99.14 cm versus 80.13 cm; p=0.0002).
A study by Galliano and Bellver (2013) showed that pre-pregnancy obesity and excessive gestational weight gain increase miscarriage rates and obstetric and neonatal complications, leading to a lower rate of healthy live births(11).
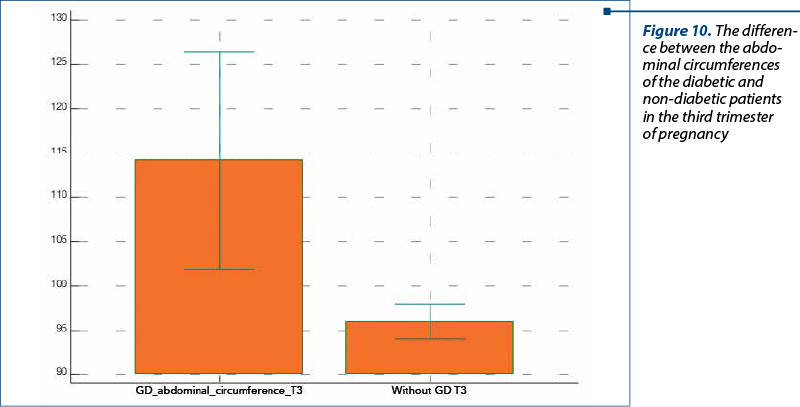
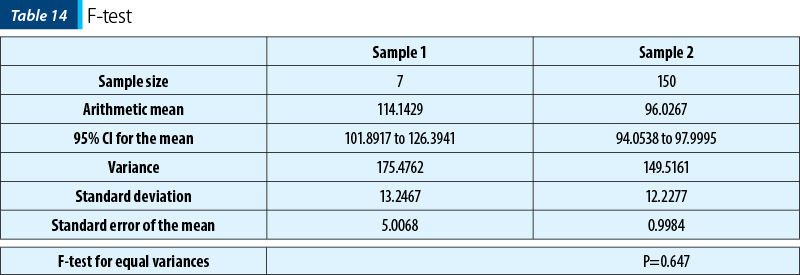
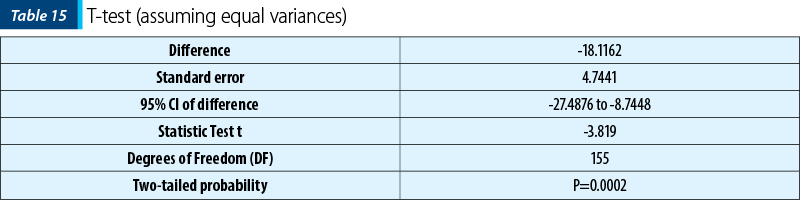
There is a statistically significant difference between the abdominal circumferences of the diabetic patients during the third semester of pregnancy (114.14 cm versus 96.92 cm; p=0.0002).
A study from 2011 showed that the prevalence of obesity in pregnancy is increasing exponentially(12). The study revealed that obesity is associated with an increased risk of maternal mortality, gestational diabetes, thromboembolism, preeclampsia and postpartum hemorrhage.
4. Conclusions
The objective of this paper was to analyze the metabolic model for the monitoring and management of gestational diabetes. This is a descriptive, retrospective and observational study, based on the medical records from the “Alessandrescu Rusescu” Institute for Maternal and Child Health database. There were included 157 patients who showed up for consult in every trimester of pregnancy.
It must be taken into consideration that the BMI value above 25 kg/m2 and the elevated abdominal circumference during all three trimesters represent negative prognostic factors for the pregnant women as well as for the fetus.
Pregnancy represents a critical period of growth, development and physiological change, providing an opportunity for early lifestyle intervention. The goal of identifying an effective lifestyle program for the gestational period that leads to healthy fetal development and subsequently to normal weight offspring less likely to develop obesity and its comorbidities is unique and could mitigate the intergenerational cycle of obesity.
Ultrasonography is used to identify congenital anomalies at the beginning of pregnancy. In 1990, Wolfe et al. showed that there was a significant impairment of adequate ultrasound visualization of fetal anatomy when BMI was greater than 36, viewing being down by 14.5%(13). A decrease in visualization was most marked for the fetal heart and spine.
The main objective in the management of obesity during pregnancy is prevention.
Fat accumulation during pregnancy is variable and may depend on the woman’s pre-pregnancy metabolic status and on other lifestyle variables such as diet and physical activity.
Basically, apart from preconceptional weight loss in the management of obese pregnant women, glucose screening should be considered in obese women in early pregnancy to rule out undiagnosed pre-gestational diabetes. Folate supplementation of grain products should be offered to obese women before conception or in early pregnancy.
Thus, the recognition of obesity as a risk factor for congenital anomalies remains an important factor to be considered by the clinician in the management of the obese pregnant women.

Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
-
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
-
Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff (Millwood). 2002;21(2):245–53.
-
WHO. Obesity: preventing and managing a global epidemic. World Health Organ Tech Rep Ser 2000;894:1–4. Available from: https://apps.who.int/iris/handle/10665/42330
-
Li G, Wei T, Ni W, Zhang A, Zhang J, Xing Y, et al. Incidence and risk factors of gestational diabetes mellitus: A prospective cohort study in Qingdao, China. Front Endocrinol (Lausanne). 2020;11:636.
-
Whitaker RC. Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics. 2004;114(1):e29–36.
-
Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. Rasmussen KM, Yaktine AL, editors. Washington (DC): National Academies Press (US); 2009. https://pubmed.ncbi.nlm.nih.gov/20669500/
-
ACOG committee opinion no. 549: obesity in pregnancy. Obstet Gynecol. 2013;121(1):213–7.
-
Carlhäll S, Bladh M, Brynhildsen J, Claesson I-M, Josefsson A, Sydsjö G, et al. Maternal obesity (Class I-III), gestational weight gain and maternal leptin levels during and after pregnancy: a prospective cohort study. BMC Obes. 2016;3(1):28.
-
Lahti-Pulkkinen M, Bhattacharya S, Wild SH, Lindsay RS, Räikkönen K, Norman JE, et al. Consequences of being overweight or obese during pregnancy on diabetes in the offspring: a record linkage study in Aberdeen, Scotland. Diabetologia. 2019;62(8):1412–9.
-
Ovesen P, Rasmussen S, Kesmodel U. Effect of prepregnancy maternal overweight and obesity on pregnancy outcome. Obstet Gynecol. 2011;118(2):305–12.
-
Galliano D, Bellver J. Female obesity: short- and long-term consequences on the offspring. Gynecol Endocrinol. 2013;29(7):626–31.
-
Norman JE, Reynolds RM. The consequences of obesity and excess weight gain in pregnancy. Proc Nutr Soc. 2011;70(4):450–6.
-
Wolfe HM, Sokol RJ, Martier SM, Zador IE. Maternal obesity: a potential source of error in sonographic prenatal diagnosis. Obstet Gynecol. 1990;76(3 Pt 1):339–42.
Articole din ediţiile anterioare
Interdisciplinary dental approach to a pregnant patient undergoing orthodontic treatment – case report
Dental treatment in pregnant women requires some particularities that limit and condition the therapeutic maneuvers(1). Endodontic pathologies in t...
Biomarkers used in the early prediction of gestational diabetes
With the increasing incidence of obesity in the general population, the incidence of gestational diabetes mellitus (GDM) has followed a similar upw...
Cervical ectopic pregnancy – case report
The definition of an ectopic pregnancy (EP) is that of a pregnancy where implantation occurs outside the endometrial cavity. Roughly 95% of EPs tak...
Lobar holoprosencephaly associated with maternal diabetes mellitus – case report
The term holoprosencephaly (HPE) describes a spectrum of cerebral and facial malformations that result from an absent or incomplete division of emb...