The utility of prophylactic salpingectomy – case report
Utilitatea salpingectomiei profilactice – prezentare de caz
Abstract
We present an informative case of a relatively young patient in which it was accidentally discovered a serous tubal intraepithelial carcinoma, after a hysterectomy with bilateral salpingectomy for a benign condition. The diagnosis was substantiated by immunomarkers p53 and Ki-67. Our case supports the concept that salpingectomy can be performed at the time of benign gynecological surgeries. It is a simple and rapid procedure that can be done with ease and does not influence the overall status of the patient. In terms of complications, it appears to be safe, as it does not increase them. The examination of the fallopian tubes samples is important, as serous tubal intraepithelial carcinoma (STIC) is one of the precursor lesions of the high-grade pelvic serous carcinoma. The mechanism of STIC development is yet neither fully understood, nor described. The investigation of p53 and Ki-67 are part of the immunohistochemistry workup that brings more information about the disease. Women who achieved reproduction and undergo pelvic surgery are recommended to have both fallopian tubes removed, but the decision should be taken by the patient, based on the benefits and risks that the medical team must explain before the procedure.Keywords
salpingectomyserous tubal intraepithelial carcinomaimmunohistochemistryRezumat
Prezentăm un caz informativ al unui paciente relativ tinere, la care a fost diagnosticat un carcinom tubar seros intraepitelial, după o histerectomie cu salpingectomie bilaterală, pentru o afecţiune benignă. Diagnosticul a fost susţinut de imunomarkerii p53 şi Ki-67. Cazul nostru pledează în favoarea conceptului în care salpingectomia poate fi efectuată în momentul intervenţiilor chirurgicale ginecologice benigne. Este o procedură simplă, rapidă, care poate fi efectuată cu uşurinţă şi nu influenţează starea generală a pacientei. În ceea ce priveşte complicaţiile, pare a fi sigură şi nu creşte riscurile acestora. Examinarea trompelor uterine este importantă, carcinomul tubar seros intraepitelial (STIC) fiind una dintre leziunile precursoare ale carcinomului seros pelvian de grad înalt. Mecanismul STIC nu este încă pe deplin înţeles şi descris. Investigarea p53 şi Ki-67 face parte din evaluarea imunohistochimică, ce aduce mai multe informaţii despre patologie. Pacientelor care şi-au încheiat viaţa reproductivă şi care beneficiază de o intervenţie chirurgicală pelviană li se recomandă extirparea ambelor trompe, dar decizia trebuie luată de pacientă, în funcţie de beneficiile şi riscurile pe care echipa medicală trebuie să le explice înainte de procedură.Cuvinte Cheie
salpingectomiecarcinom tubar seros intraepitelialimunohistochimieIntroduction
Pelvic high-grade serous carcinoma – including ovarian carcinoma, tubal carcinoma and primary peritoneal carcinoma – has an important clinical significance because of the rapid progression and extension of the disease at the time of diagnosis and the late presentation, when there is a poor prognosis due to the advanced stage(1).
Before 2001, the pathogenesis of ovarian cancer was seen to be at the ovarian surface epithelium or cortical epithelial inclusions that occurred during ovulation, with different subtypes due to cellular metaplasia. In 2001, there were published reports on the high rate of tubal neoplastic lesions in the risk-reducing bilateral salpingo-oophorectomy specimens from high-risk women(2,3). According to other reports with similar findings, the idea that fallopian tubes were the site of origin for various serous ovarian cancers was suggested by Crum et al.(4)
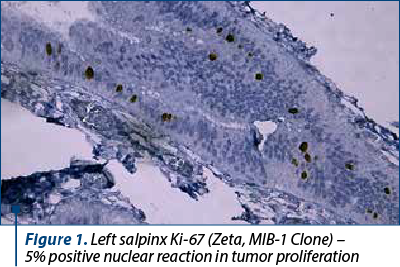
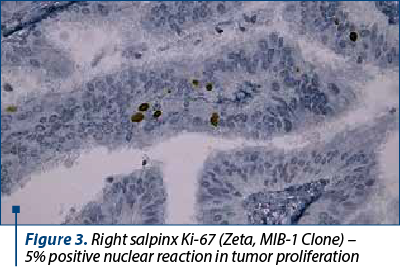
Nowadays there are theories regarding the epithelium of the fallopian tubes to be regarded as the origin of epithelial ovarian cancer. The distal fallopian tube has been documented as the site origin in BRCA1 or BRCA2 positive tumors(5,6). The precursors lesions detected by examining fallopian tubes samples both by histomorphology and by immunohistochemistry with p53 and Ki-67 are important to investigate, given the origin of pelvic serous cancers and their complexity(5,7).
Case report
A 47-year-old patient presented in March 2023 to the Obstetrics and Gynecology Department of the “Sf. Ap. Andrei” County Emergency Clinical Hospital, Constanţa, with menometrorrhagia, reported as occurring the previous year. She had no relevant medical history. The patient had two vaginal births, no abortions or miscarriages, and menarche at 13 years old.
The gynecological clinical exam revealed a healthy cervix, an enlarged uterus, non-painful adnexal areas and normal Douglas pouch. The vaginal ultrasound showed an inhomogeneous anterior myometrial texture, globular uterus (95/81/87 mm), with normal adnexa. Dilatation and curettage were first performed, for diagnostic and hemostatic purpose. The histopathologic report concluded for the tissue sample to be part of an endometrial polyp. The patient returned to the hospital in May 2023 with the same menometrorrhagia. The laboratory test included complete blood count, coagulation profile, AST, ALT, urea, creatinine, and glycemia levels. The blood results revealed hypochromic microcytic anemia (11 g/dL), and the glycemia level was 115 mg/dL. Pap smear was negative for intraepithelial or malignant lesions.
According to the patient’s age, the symptoms and her informed option and consent, the treatment chosen was total hysterectomy with bilateral salpingectomy, taking into consideration the age of the patient and her desire to preserve the hormonal status of the ovaries until menopause. Intraoperatively, an enlarged uterus was found, with normal appearing ovaries and salpinges.
The patient was discharged from the hospital two days later, in good overall condition, with moderate anemia (9.8 g/dL). The macroscopic description of the hysterectomy specimen was uterus with the mass of 470 g, dimensions 130/120/50 mm, uterine cavity lined by an endometrium for the most part, with the exception of an area with a maximum diameter of 30 mm both on the anterior and posterior surface, with a slightly irregular appearance, with whitish color; intramyometrially, on the anterior face, a nodular lesion was identified, which was imprecisely delimited on the section. Left salpinx of elastic consistency with a length of 45 mm and a diameter of 7 mm, smooth serous with obvious vascularization and right salpinx with the same characteristics, but length of 55 mm and a diameter of 6 mm. The final histopathological result (on paraffin sections) of the hysterectomy specimen was endometrial polyp residue, adenomyoma with the largest diameter of 20 mm and papillary cervicitis.
Both salpinges revealed restricted areas of serous tubal intraepithelial carcinoma (STIC), and the immunohistochemistry confirmed bilateral STIC with Ki-67 – positive nuclear reaction in approximately 5% in the tumor proliferation, and p53 with weakly positive nuclear reaction (Figures 1-4). Thoracopulmonary examination performed with X-rays revealed no evolutionary pleuro-pulmonary lesions.
Following the histopathological and immunohistochemistry results, the definitive treatment by laparoscopic bilateral oophorectomy was performed. The patient was discharged the following day, in a good overall condition, with a well-balanced hemodynamic status and without surgical complications. The histomorphological result revealed both ovaries with normal histological structure. The patient is yet to be tested for the BRCA1 and BRCA2 mutations, with the follow-up of the patient being in progress.


Discussion
Prophylactic salpingectomy is a preventive surgery in which the removal of the entire fallopian tubes with hysterectomies is performed for women to decrease the risk of ovarian or peritoneal serous cancers in patients already undergoing the surgical procedure for a benign disease. Since screening and early detection of such malignancies are difficult to be achieved, the removal of the fallopian tube is being targeted as a method of prevention(1). Precursor lesions inside the fallopian tube or ovary cannot be sufficiently early detected by the current imaging technologies (ultrasound, CT and MRI scans).
It is suggested that tubal intraepithelial carcinoma is associated with one-third to almost half of pelvic serous carcinomas. This leads to the belief that some carcinomas that appear to arise from ovarian or peritoneal tissue might be of tubal origin instead. Mouse model studies testify the origin of pelvis high-grade serous carcinoma (HGSC) in the fallopian tube. Furthermore, the removal of the fallopian tube prevented cancer initiation, whereas bilateral oophorectomy had no effect(8).
The epithelium of the fallopian tube consists in a mixture of secretory cells predominantly in the tubal isthmus and ciliated cells at the fimbriated end(9). One of the entities originating from secretory cells that have been described is STIC, which is the most atypical. The assessment of the morphological and immunohistochemical features constitutes the basis of the STIC diagnosis. It is recognized that the optimal diagnosis of serous tubal intraepithelial carcinoma needs more data than the histologic assessment. Therefore, immunohistochemical expression of p53 and Ki-67 improved the reproducibility of the diagnosis. Tests for p53 and increased Ki-67 proliferative activity index features help in the identification of the respective abnormalities.
The fimbriated end of the uterine tube is the most frequent site of serous tubal intraepithelial lesions and tubal intraepithelial lesions, while secretory cell outgrowths are distributed throughout the tube.
The mechanism of serous tubal intraepithelial carcinoma developing into invasive pelvic serous carcinoma is neither described yet, nor understood. STIC is mostly described from the pathomorphological point of view, not focusing properly on the clinical significance or treatment(10). STICs are tubal precursor lesions of ovarian carcinoma, not metastases from ovarian carcinoma (as they express different telomere lengths between STICs and ovarian cancers)(11).
Women with inheritance of a germline mutation in a cancer predisposing gene, such as BRCA1 or BRCA2(12), are recommended to have prophylactic salpingectomy and oophorectomy once childbearing is completed(13,14). A staged procedure begins with the bilateral salpingectomy and, subsequently, continues with the bilateral oophorectomy, in case of abnormal salpingeal histopathological results. This strategy had the benefit of avoiding the morbidity of premature menopause, but it comes with the cost of an uncertain impact on the overall mortality or on the breast cancer risk reduction. Risk reducing bilateral salpingectomy followed by delayed oophorectomy has the highest quality-adjusted life expectancy(15). Still, no prospective data exist about the efficacy of bilateral salpingectomy in reducing mortality in high-risk women, but it might be probably superior than no surgery approach. Moreover, salpingectomy at the time of hysterectomy for benign diseases appears to be safe, and the postoperative complications (infections, blood transfusions) are similar to the ones in case of hysterectomy alone. The results on surrogate serum markers or on their response to in vitro fertilization suggest that ovarian function is not altered(16).
The surgical technique should involve the complete removal of the tube from the uterotubal junction to its fimbriated end; the interstitial portions of the tubes do not need to be removed. Complete salpingectomy is preferred over fimbriectomy because throughout all the fallopian tube precursors to fallopian or ovarian cancer can be found. If fimbrial attachments on the ovary can still be found, they should be removed or cauterized(11).
Conclusions
We present an informative case of a relatively young patient in which it was accidentally discovered a serous tubal intraepithelial carcinoma, after a hysterectomy with bilateral salpingectomy for a benign condition.
Our case supports the concept that salpingectomy, performed at the time of benign gynecological surgeries, is a simple and rapid procedure that can be performed with ease and involves minimal morbidity. Scientific community and boards are in favor of, or at least recommend the removal of both fallopian tubes in women who achieved reproduction and undergo pelvic surgery. This procedure is considered as a prophylactic measure against the development of high-grade serous cancer. More data from randomized studies can represent the key in the better understanding of the utility of salpingectomy. However, the decision should be taken by the patient, based on a previous discussion with the medical team about the choices and after fully understanding all the relevant benefits and risks.
Conflict of interest: none declared.
financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.
Bibliografie
-
Kar T, Kar A, Dhal I, Panda S, Biswal P, Nayak B, Rout N, Samantray S. Serous tubal carcinogenesis: the recent concept of origin of ovarian, primary peritoneal and fallopian tube high-grade serous carcinoma. J Obstet Gynaecol India. 2017;67(6):432-41.
-
Piek JM, van Diest PJ, Zweemer RP, et al. Dysplastic changes in prophylactically removed Fallopian tubes of women predisposed to developing ovarian cancer.
-
J Pathol. 2001;195(4):451–6.
-
Colgan TJ, Murphy J, Cole DE, Narod S, Rosen B. Occult carcinoma in prophylactic oophorectomy specimens: prevalence and association with BRCA germline mutation status. Am J Surg Pathol. 2001;25(10):1283–9.
-
Kindelberger DW, Lee Y, Miron A, et al. Intraepithelial carcinoma of the fimbria and pelvic serous carcinoma: Evidence for a causal relationship. Am J Surg Pathol. 2007;31(2):161–9.
-
Crum CP. Intercepting pelvic cancer in the distal fallopian tube: theories and realities. Mol Oncol. 2009;3(2):165–70.
-
Herrington CS, Mc Cluggage WG. The emerging role of the distal Fallopian tube and p53 in pelvic serous carcinogenesis. J Pathol. 2010;220(1):5–6.
-
Jarboe E, Folkins A, Nucci MR, et al. Serous carcinogenesis in the fallopian tube: a descriptive classification. Int J Gynecol Pathol. 2008;27(1):1–9.
-
Kim J, Coffey DM, Creighton CJ, et al. High-grade serous ovarian cancer arises from fallopian tube in a mouse model. Proc Natl Acad Sci USA. 2012;109(10):3921–6.
-
Lamps L (Ed.). Diagnostic Pathology: Normal Histology, 1st ed; Amirsys, Inc: Salt Lake City, UT, USA, 2013.
-
Weinberger V, Bednarikova M, Cibula D, Zikan M. Serous tubal intraepithelial carcinoma (STIC) – clinical impact and management. Expert Rev Anticancer Ther. 2016;16(12):1311-21.
-
Chene G, Rahimi K, Mes-Masson AM, et al. Surgical implications of the potential new tubal pathway for ovarian carcinogenesis. J Minim Invasive Gynecol. 2013;20(2):153–9.
-
Mavaddat N, Peock S, Frost D, et al. Cancer risks for BRCA1 and BRCA2 mutation carriers: results from prospective analysis of EMBRACE. J Natl Cancer Inst. 2013;105(11):812–22.
-
National Comprehensive Cancer Network (NCCN). Genetic/High-Risk familial Assessment: Breast and Ovarian. 2013;4.
-
National Institute of Health and Care Excellence (NICE) Familial Breast Cancer: Classification and Care of People at Risk of Familial Breast Cancer and Management of Breast Cancer and Related Risks in People with a Family History of Breast Cancer. 2023. https://www.nice.org.uk/guidance/cg164
-
Kwon JS, Tinker A, Pansegrau G, et al. Prophylactic salpingectomy and delayed oophorectomy as an alternative for BRCA mutation carriers. Obstet Gynecol. 2013;121(1):14–24.
-
ACOG Committee Opinion No. 774: Opportunistic Salpingectomy as a Strategy for Epithelial Ovarian Cancer Prevention. Obstet Gynecol. 2019;133(4):e279-e284.





