Regarded as a lethal condition, pentalogy of Cantrell is a rare congenital syndrome that presents in its complete form the following five defects: defect of the abdominal wall closure at the superior part, sternal fusion defect, cardiac malformations, defect of the diaphragm, and defect of the pericardium. Using data from reported cases of survivors who have received complex treatments for the anomalies, this article aims at describing the possible ways of monitoring these pregnancies and of predicting prenatal and postnatal outcomes. The optimal treatment conditions require supervision by multidisciplinary teams in a third-level maternity with neonatal intensive care units and maternal-fetal departments and neonatal surgery department. Moreover, establishing the chronology for the corrections of the defects, solving anaesthetic problems and postnatal ventilator support are necessary for the correct treatment of this syndrome.
Prognosticul în cazul pentalogiei lui Cantrell
Prognosis of pentalogy of Cantrell
First published: 16 martie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.68.1.2020.3031
Abstract
Rezumat
Pentalogia lui Cantrell este un sindrom congenital rar, considerat letal, care asociază în forma sa completă următoarele cinci defecte: defect la nivelul peretelui abdominal anterior superior, defect de închidere a sternului, malformaţii cardiace şi defecte ale diafragmului şi ale pericardului. Deoarece au fost raportate cazuri de supravieţuitori după tratamentul complex al anomaliilor din pentalogia lui Cantrell, acest articol îşi propune să prezinte modalitatea de monitorizare a acestei sarcini şi stabilirea prognosticului pre- şi postnatal. Supravegherea sarcinii în centre supraspecializate de către echipe pluridisciplinare, naşterea într-o maternitate de nivel III şi posibilităţile de reanimare neonatală asigură condiţii optime de tratament. Stabilirea cronologiei corectării defectelor, rezolvarea problemelor anestezice şi suportul ventilator postnatal sunt necesare pentru tratamentul corect al acestui sindrom.
Pentalogy of Cantrell is a rare congenital syndrome, with around 250 cases described in the medical reports until 2015(1). Pentalogy of Cantrell is considered and classified as an abdominal wall closure defect. This syndrome associates five defects: defect in the closure of the anterior superior abdominal wall, defect in the sternal fusion, heart malformations, defect of the diaphragm and defect of the pericardium. The heart is located intrathoracic, but dextrorotated and the heart pulsations can be palpable at the level of the omphalocele through the umbilical cord.
In the last 20 years, the survival of some children with pentalogy of Cantrell has been made possible by the technological developments of minimally invasive surgical techniques from neonatal and pediatric surgery.
While it is not possible to speak from experience regarding this rare syndrome, which is considered lethal, discussion and clarification of the reported cases can be useful in situations where practitioners are confronted with this pathology and parents desire to continue the pregnancy.
In this article, we aim to reiterate the definition of the pentalogy of Cantrell and to describe the pre- and postnatal diagnosis and the management of pregnancy, including prenatal counseling and parameters of establishing the prognosis. More than one hundred years ago, Neil Stenonis described a child with an open chest (sternum) through which the heart, spleen and liver came out(2). The name of the syndrome appeared in 1958, when James Cantrell, Haller and Ravitch published three cases of children with this pathology(3), considering it to be a peritoneal diaphragmatic pericardial hernia. Although the prenatal diagnosis in our country is well-rated, only two cases with poor prognosis were reported(4,5).
The following five malformations are described in the pentalogy of Cantrell(6):
1. Defect of abdominal wall closure at the epigastric level.
2. Defect of the closure of the sternum.
3. Defect of the anterior diaphragm.
4. Defect of the diaphragmatic pericardium.
5. Heart malformations.
This syndrome must be differentiated from ectopia cordis. In the case of pentalogy of Cantrell, the heart is normally positioned within the chest, but it is dextrorotated with the apex towards the parietal defect and covered by the skin or peritoneal membrane.
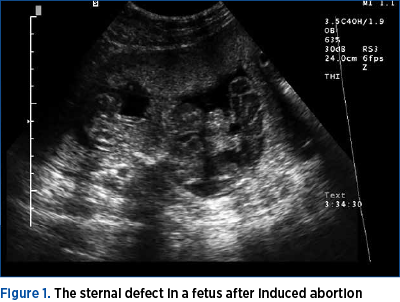
The etiology of pentalogy of Cantrell is multifactorial, involving genetic mutations, chromosomal abnormalities (trisomy 18 and Turner syndrome), chemical and physical teratogens(7,8). The variety of mutations associated with pentalogy of Cantrell include deletions or duplications of the PORCN gene, thoracoabdominal syndrome (TAS), ALDH 1A2 and teneurin-4 (TENM4) genes. All studies agree that it occurs early in pregnancy, between days 14 and 18 of the embryological development, and that it is caused by the developmental failure of the mesoderm and by the failure of the ventral migration of primitive mesoderm structures(4-8). The prenatal diagnosis is made through ultrasound, beginning with the first trimester of pregnancy. Thus, the observation of the closure defect of the abdominal wall at the epigastric level (omphalocele/gastroschisis) associated with sternal defect raises the suspicion of pentalogy of Cantrell (Figures 1 and 2). The sternal cleft, diaphragmatic hernia and pericardial defects are difficult to visualize in the first trimester of pregnancy.
Pentalogy of Cantrell is classified as(9):
-
Class 1 – defined diagnosis, associating the five defects.
-
Class 2 – probable diagnosis, associating four defects.
-
Class 3 – an incomplete expression of this syndrome, which necessarily associates the sternal defect and sometimes the abdominal wall defect and the dextrorotated cord.
Cardiac malformations in pentalogy of Cantrell
Pentalogy of Cantrell in the classical form is associated with cardiac malformations in about 80% of cases(4,6): ventricular septal defect (65-100% of cases), atrial septal defect, tetralogy of Fallot, hypoplasia of the pulmonary artery, left ventricular diverticulum and others. For example, a series of 21 cases reported by J. Rubens Figueora(2) had dextrocardia especially in cases without ventricular diverticulum and the association of several structural heart defects, double outlet in the right ventricle (24%), tricuspid stenosis, hypoplastic left syndrome, hypoplastic left ventricle, Taussig-Bing syndrome, pulmonary atresia, single atrium, atrioventricular discordance and others. The heart in the pentalogy of Cantrell is located within the fetal chest (thoracoabdominal ectopia cordis). An association with ectopia cordis (cervical, thoracic, abdominal) is possible, and such cases have a very poor prognosis. The heart is covered by peritoneum or skin. The prognosis is better for noncomplex heart defects, ventricular septal defect (28%), the persistence of ductus arteriosus or atrial septal defect. Postnatally, an echocardiography and/or magnetic resonance evaluation can be indicated before surgery.
Abdominal wall defects in pentalogy of Cantrell
The omphalocele vary in size and can contain intestinal loops, liver and spleen. The fetal karyotype is indicated in case of cardiac structural malformations, omphalocele, or other structural abnormalities. Less commonly, gastroschisis has been reported in the pentalogy of Cantrell.
Other associated anomalies have been described in case reports series: cranial malformations (encephalocele, myelomeningocele, anencephaly), facial abnormalities (cleft lip and cleft palates, anoftalmia)(6,10), limb anomalies(11), kyphoscoliosis, OEIS syndrome (omphalocele – exstrophy – imperforate anus – spinal defects)(12-14). The diagnosis of a chromosomal abnormality, a major structural heart defect incompatible with survival or even the wish of the parents can indicate a therapeutic abortion (up to 24 weeks in our country) (Penal code)(15).
The fetal prognosis is established through the following ultrasound elements:
-
The width and content of omphalocele.
-
Type of heart malformations. Type 3 pentalogy of Cantrell with no associated cardiac malformations/or DSV, DSA has a better prognosis.
-
Associated anomalies.
-
Genetic and chromosomal disorders that have a poor prognosis.
Association with intrauterine growth restriction.
Complications of the omphalocele: its rupture, polyhydramnios or the complications of gastroschisis and its association with intestinal atresia.
No cases of spontaneous intrauterine fetal death have been described and many of the reported cases were diagnosed late in pregnancy or postnatally, despite the prenatal diagnosis by ultrasound screening evaluation.
Birth plan and management
Childbirth must be performed in third-level perinatal care maternity units, including neonatal intensive care unit and neonatal surgery. There are no prospective studies to compare vaginal versus caesarean section deliveries for these cases. All the authors agree with caesarean section only in case of large omphalocele or in case of obstetrical indications.

Postnatal treatment
The postnatal surgical treatment has been performed only in superspecialized neonatal and pediatric surgery departments with a neonatal intensive care unit. The steps to correct cardiac and/or abdominal wall defects undergo more surgical interventions. As well, the time for the correction of the defects must be determined precisely, since prognosis depends on it. It should be emphasized that these patients have pulmonary immaturity with low pulmonary and ventilator capacities. Patients with pentalogy of Cantrell have been shown to tolerate intraabdominal pressure up to 25-35 cm H2O(16). T. Saito et al. assert that surgery on the first day after birth causes mortality in 100% of cases(17). Some of the cases described in literature postponed the repair of the omphalocele(18,19) and in other cases it was performed the early repair by integrating the heart into the physiological position and closing all pericardial and diaphragm defects(20). There are also cases described in literature involving an initial repair of the pericardial and diaphragmatic defect and reintegration of the heart into the chest(16), followed by the closing of the abdominal defect. Due to significant clinical changes in the hemodynamic parameters and changes in thoracic and abdominal volumes, the evolution is usually unfavorable(16). Anaesthesia is a major challenge(17), as the closure of each defect may severely compromise the function of the underlying organ. Hemodynamic instability and respiratory management require attention and ability due to pulmonary immaturity, cardiac structural defects, and high intrabdominal pressure. The intraoperative complications are related to hemodynamic variations, with the possibility of cardiac arrhythmias. Postoperatively, the main cause of mortality is the prosthetic patch: the materials used to close the defects or repair techniques of parietal defects. They represent the main risk for sepsis.
The fetal death of patients can be either at birth – in case of abnormalities incompatible with life – or in the postpartum period. On a series of 21 patients operated before 2009, only four survivors are described, the cause of death being sepsis, synthetic materials and abdominal wall closure techniques, cardiogenic shock, multiple organ failure; the patients were usually intubated postoperatively(2). After repairing the defects and creating near-normal living conditions, many of these children and adults require respiratory ventilation support at home.
Conclusions
The management of pentalogy of Cantrell represents a great multidisciplinary challenge, involving maternal-fetal medicine specialist, obstetrician, anesthesiologist, cardiovascular and pediatric surgeons, geneticist and neonatal intensive care specialist. Being a rare pathology, one cannot talk about prospective studies; however, the reported cases were from superspecialized centres, both in prenatal diagnosis and neonatal surgery, in which the postnatal investigations accurately established the type of abnormalities and the optimal time for surgical resolution. When present, the pentalogy of Cantrell requires great efforts from multidisciplinary teams, with survival highly depending on the evolution from diagnosis to treatments, on the cardiac malformations, but also on the tolerance of closing the defects.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
2. de Rubens Figueroa J, Sosa Cruz EF, Díaz García L, Carrasco Daza D. Cardiac malformations in patients with pentalogy of Cantrell and ectopia cordis. Rev Esp Cardiol. 2011 Jul; 64(7):615-8.
3. Cantrell JR, Haller JA, Ravitch MM. A syndrome of congenital defects involving the abdominal wall, sternum, diaphragm, pericardium, and heart. Surg Gynecol Obstet. 1958 Nov; 107(5):602-14.
4. Mărginean C, Mărginean CO, Gozar L, et al. Cantrell Syndrome – A Rare Complex Congenital Anomaly: A Case Report and Literature Review. Front Pediatr. 2018; 6:201- 6.
5. Grigore M, Furnică C, Esanu C, Gafiţeanu D. Pentalogy of Cantrell associated with unilateral anophthalmia. Case report and literature review. Medicine. 2018; 97(31): p e 11511.
6. Bianchi D, Crombleholme TM, D’Alton ME. Pentalogy of Cantrell. In: Fetology. Diagnosis & Management of the fetal patient. Ed. McGraw-Hill, Medical Publishing Division.
7. Parvari R, Weinstein Y, Ehrlich S, Steinitz M, Carmi R. Linkage localization of the thoraco-abdominal syndrome (TAS) gene to Xq25-26. Am J Med Genet. 1994 Feb 15; 49(4):431-4.
8. MacTaggart B, Bowen C, Markowitz M, Chong J, Bamshad M, Ma X, Adelstein RS. Using whole-exome sequencing to identify genetic variants in patients diagnosed with pentalogy of Cantrell; Proceedings of the 30th Annual Showcase of NIH Intramural Research; Bethesda, MD, USA. 14 September 2016.
9. Toyama WM. Combined congenital defects of the anterior abdominal wall, sternum, diaphragm, pericardium, and heart: a case report and review of the syndrome. Pediatrics. 1972; 50(5) 778–786.
10. Whahab S, et al. Prenatal diagnosis of pentalogy of Cantrell in a case with craniorachischisis. Current Pediatric Research. 2017; 21, Issue 1.
11. Uygur D, Kis S, Sener E, Gunce S, Semerci N. An infant with pentalogy of Cantrell and limb defects diagnosed prenatally. Clin Dysmorphol. 2004; 13:57–8.
12. Carmi R, Boughman JA. Pentalogy of Cantrell and associated midline anomalies: a possible ventral midline developmental field. Am J Med Genet. 1992; 42:90–5.
13. Polat I, Gul A, Aslan H, et al. Prenatal diagnosis of pentalogy of Cantrell in three cases, two with craniorachischisis. J Clin Ultrasound. 2005; 33:308–11.
14. Chen PG. Syndromes and disorders associated with omphalocele (II): OEIS complex and Pentalogy of Cantrell. Taiwan J Obstet Gynecol. 2007: 46(2): 103-110.
15. New Penal code. Article 201. Available at: https://lege5.ro/Gratuit/gezdmnrzgi/art-201-intreruperea-cursului-sarcinii-codul-penal accessed on 12.02.2020
16. Costa JVS, Melonio CEC, Vieira CB. Anesthesia for surgical repair of the pentalogy of Cantrell: case report. Revista Brasileira de Anestesiologia. 2019; 69(3): 322-325.
17. Saito T, Suzuki A, Takahata O, et al. Anesthetic management of a patient with Cantrell’s pentalogy diagnosed prenatally. Can J Anaesth. 2004; 51:946-947.
18. Wheeler DS, St Louis JD. Pentalogy of Cantrell associated with hypoplastic left heart syndrome. Pediatr Cardiol. 2007 Jul-Aug; 28(4):311-3.
19. Saxena AK, van Tuil C. Delayed three-stage closure of giant omphalocele using pericard patch. Hernia. 2008 Apr; 12(2):201-3.
20. Divkovic D, Kvolik S, Sipl M, Sego K, Puseljic S, Rakipovic-Stojanovic A, Kovacic B. A successful early gore-tex reconstruction of an abdominal wall defection a neonate with Cantrell pentalogy: a case report and literature review. Clin Case Rep. 2015 Jan; 3(1):19-23.
Articole din ediţiile anterioare
Provocări în evaluarea feţei fetale – diagnostic şi management
The ultrasound assessment of the fetal face is the first way of interaction of the parents with their unborn baby, therefore recent achievements in...
Sarcina cicatricială după operaţia cezariană – o continuă dilemă terapeutică. Serie de cazuri şi review al literaturii
Sarcina cicatricială după operaţie cezariană (CSP) este o tulburare iatrogenă care pune viaţa în pericol, cu o incidenţă tot mai mare, din cauza cr...
Managementul prenatal şi postnatal în tetralogia Fallot
Anomaliile morfologice ale aparatului cardiovascular reprezintă o cauză majoră de morbiditate şi mortalitate neonatală. O ecografie fetală de rutin...
Consilierea în agenezia ductului venos secundară venei cave inferioare întrerupte
The ultrasound (US) examination of the fetal venous system has exposed a wide spectrum of malformations.