The identification of prognostic and predictive biomarkers in oncological pathology is a desideratum of translational research in cancer. The neutrophil-lymphocyte ratio (NLR) and the platelet-lymphocyte ratio (PLR) were considered suggestive to characterize both cell-mediated immune status and inflammation in cancer, thus being potential biomarkers. Due to the high rate of therapeutic failure even in the case of a treatment with curative potential, head and neck cancers are a priority in the research of potential biomarkers that allow a stratification of risk groups in order to adapt the therapy. The aim of the study is the dynamic evaluation of NLR and nadir PLR and during chemotherapy cycles for patients with multimodal, nonsurgically treated head and neck cancers. The mean NLR and PLR values vary during treatment, but the mean nadir value is not significantly different from the mean NLR and PLR values before the last cycle of chemotherapy. If there is solid evidence regarding the role of NLR nadir as a biomarker, the evaluation of NLR and PLR dynamics requires further research to confirm the possibility of being validated as a prognostic or predictive biomarker of response to chemotherapy and radiotherapy in head and neck squamous cell carcinoma.
Evoluţia raportului neutrofile-limfocite (NLR) şi a raportului trombocite-limfocite în timpul polichimioterapiei în cancerele capului şi gâtului
The evolution of the neutrophil-lymphocyte ratio (NLR) and the platelet-lymphocyte ratio during polychemotherapy in head and neck cancers
First published: 24 aprilie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.55.2.2021.5014
Abstract
Rezumat
Identificarea unor biomarkeri prognostici şi predictivi în patologia oncologică este un deziderat al cercetării translaţionale în cancer. Raportul neutrofile-limfocite (NLR) şi raportul trombocite-limfocite (PLR) au fost considerate sugestive pentru a caracteriza atât statusul imun mediat celular, cât şi inflamaţia în cancer, fiind astfel potenţiali biomarkeri. Prin rata mare de eşec terapeutic, chiar şi în cazul unui tratament cu potenţial curativ, cancerele capului şi gâtului sunt o prioritate în cercetarea unor potenţiali biomarkeri care să permită o stratificare a grupelor de risc în scopul adaptării terapiei. Obiectivul studiului este evaluarea în dinamică a NLR şi a PLR nadir şi în timpul ciclurilor de chimioterapie ale pacienţilor cu cancere ale capului şi gâtului tratate multimodal nonchirurgical. Valorile medii ale NLR şi PLR variază pe parcursul tratamentului, dar valoarea medie nadir nu este semnificativ diferită faţă de valorile medii NLR şi PLR înaintea ultimului ciclu de chimioterapie. Dacă în ceea ce priveşte rolul NLR nadir ca biomarker există evidenţe solide, evaluarea dinamicii NLR şi PLR necesită cercetări suplimentare pentru a confirma posibilitatea de a fi validate ca biomarker prognostic sau predictiv al răspunsului la chimioterapie şi radioterapie în carcinoamele cu celule scuamoase ale capului şi gâtului.
Introduction
Rudolf Virchow is credited for the first correlations of chronic inflammation with cancer since the 19th century. The relationship between inflammation and cancer is one in both directions, inflammation being indirectly associated with DNA damage and carcinogenesis, but at the same time cancer activates inflammation, proliferation, angiogenesis and decreased apoptosis. Thus, the identification of biomarkers as specific as possible for cancer-associated inflammation could indirectly lead to the identification of predictive and prognostic biomarkers in oncology. Head and neck cancers are of particular interest in predicting evolution, given the high rate of therapeutic failure, especially in the locally advanced and metastatic stages. Head and neck squamous cell carcinoma (HNSCC) represents the majority of cases of head and neck cancer, being associated with heavy smoking, but also with human papillomavirus (HPV) infection, especially in young patients. The association of HPV etiology was correlated with a favorable prognosis and a superior response to nonsurgical treatment (chemotherapy and radiotherapy). The identification of other biomarkers could stratify patients for a personalized approach in order to adapt the treatment by escalation or de-escalation. The neutrophil-lymphocyte ratio (NLR) and the platelet-lymphocyte ratio (PLR) have been identified as a potential biomarker not only in cancer but also in other diseases, including diabetes, pneumonia, myocardial infarction and rheumatic inflammatory diseases. In this context, the increasingly intense exploration of these ratios in oncology is a topic of interest in research due to the advantages of accessibility and low cost. We analyzed data obtained from 20 patients treated between 2016 and 2019 in the Oncology Clinic of the Craiova County Emergency Clinical Hospital in order to evaluate NLR and PLR nadir (before chemotherapy treatment) and before each cycle of chemotherapy(1-15).
Materials and method
We analyzed data obtained from 20 patients treated between 2016 and 2019 in the Oncology Clinic of the Craiova County Emergency Clinical Hospital. The primary tumor sites of locally advanced, relapsed or metastatic HNSCC were nasopharynx, oropharynx, oral cavity, hypopharynx and larynx. The inclusion criteria were: HNSCC, at least three chemotherapy courses with at least two agents, including a platinum salt, complete blood count obtained before each cycle of chemotherapy. From the complete blood count, NLR was calculated as the ratio between the absolute number of neutrophils and the absolute number of lymphocytes. PLR was calculated as the ratio between the absolute number of platelets and the absolute number of lymphocytes. Both the nadir value and the value calculated from complete blood count recorded before each chemotherapy cycle, during a maximum of six cycles, were evaluated.
The aim of the study was the dynamic evaluation of NLR and PLR nadir and during the cycles of chemotherapy of patients with locally advanced and metastatic head and neck cancers treated multimodally by chemotherapy and radiotherapy.
Results
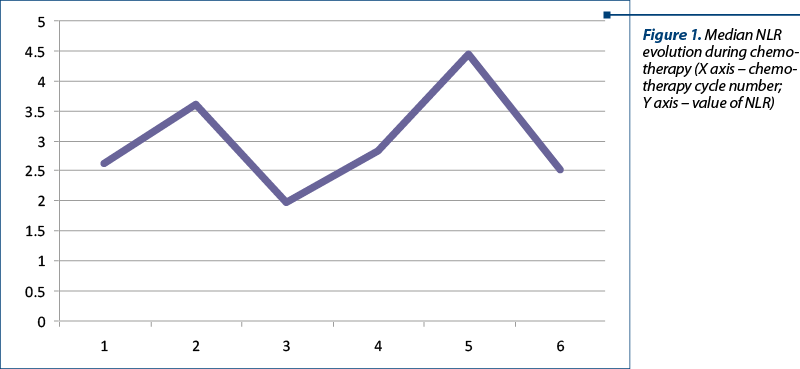
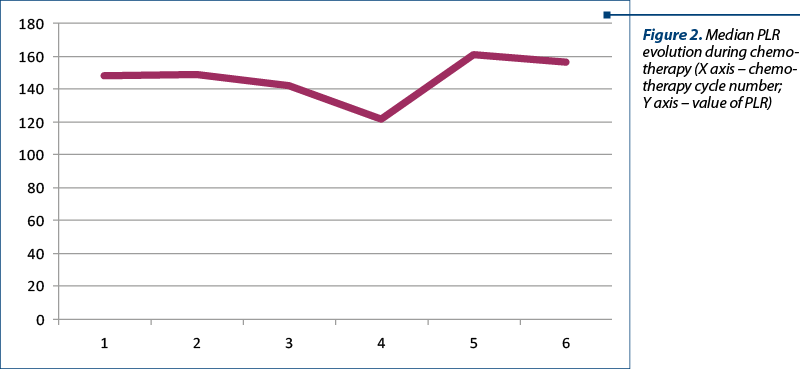
All patients included in the studies were aged between 53 and 68 years old and had primary tumors stages III-IV (stage T between T2 and T4, stage N between N0 and N3, and stage M0); only one patient was initially treated after locoregional recurrence. Sixteen of the 20 patients received radiotherapy at a total dose of 50 Gy in 25 fractions, 5 fractions per week, and received between 4 and 6 cycles of chemotherapy with carboplatin, 5-fluorouracil, docetaxel, paclitaxel and gemcitabine. In cases where concomitant radiotherapy with chemotherapy was administered, carboplatin was used in all cases. Only one patient received cetuximab and carboplatin at relapse. The mean value of NLR nadir was 2.6, with a minimum value of 1.19 and a maximum value of 4.7. The mean nadir value of PLR was 147.7, with a minimum of 86.3 and a maximum of 205.3. The minimum mean NLR was 1.96 and was obtained before the third cycle of chemotherapy and the maximum value was 4.4 and was obtained before the fifth cycle of chemotherapy. The minimum mean PLR value was obtained before the fourth cycle of chemotherapy and had a value of 120.9, and the maximum value was obtained before the fifth cycle of chemotherapy and had a value of 160.6. After the last cycle of chemotherapy for which the evaluation was performed, the mean value of NLR was 2.50, with a maximum value of 5.2 and a minimum value of 1.35. The mean value of PLR before the sixth cycle of chemotherapy was 155.7, with a minimum value of 53.9 and a maximum value of 246.1 (Figures 1 and 2).
Discussion
Increasing data support the concept that NLR and PLR are associated with immune dysregulation and simultaneously with the proinflammatory or antiinflammatory response. These reports demonstrate the potential of NLR and PLR to be prognostic and predictive biomarkers in various diseases, from infections, sepsis to diabetes, heart diseases and cancer. The immunomodulatory and modulatory role of inflammation by releasing proinflammatory cytokines, but also by the potential effect of the platelet relationship with NK cells, macrophage and T lymphocytes, is already known. Lymphocytes are also associated with an affected inflammatory response and, thus, the two ratios represent a better indicator of an impairment of the balance between cell-mediated immune status, on the one hand, and acute and chronic inflammation, on the other hand. If elevated NLR is a predictor of a negative evolution or an unfavorable prognosis, in the case of PLR the results are contradictory. Elevated PLR have been identified as an unfavorable prognostic biomarker for colorectal cancer, as demonstrated by a systematic review and meta-analysis conducted by Zhang et al., including six studies that have demonstrated the association of PLR with the prognosis. In the case of overall survival (OS), five studies, including 966 patients, and three studies, including 471 cases with endpoint disease free survival (DFS), were analyzed. In the case of OS, no correlation was identified between the PLR value and the prognosis. In case of NLR, on a sample including several studies and several patients (13 studies and 4628 patients), the analysis of some subgroups did not correlate OS with NLR, but with a cutoff value of 5, NLR was correlated with DFS. Takenaka et al. identified both thrombocytosis and higher PLR as being associated with the unfavorable prognosis of HNSCC, by analyzing data from nine studies and 2327 patients(1-3,5,6).
A study that evaluated the prognostic potential of NLR and PLR in head and neck cancers compared data from 170 histopathologically diagnosed patients and a control group of 80 subjects. The study highlighted the positive correlation of NLR and PLR values with a high degree of differentiation and advanced TNM stages, both an advanced T and N stage being positively correlated with increased values of the two ratios. The authors recommend the use of elevated NLR and PLR values in head and neck cancers as a marker for poor prognosis, but they recommend evaluation in a larger patient group, and suggested the need for evaluation and predictive potential of response to therapy. Analyzing data from 186 patients with squamous cell carcinomas of the oropharynx, oral cavity, hypopharynx and larynx treated with primary or adjuvant (chemo-) radiation, Bojaxhiu et al. demonstrated the correlation of NLR with OS, but PLR was not identified as correlated with treatment toxicity and with patients’ outcomes. The authors consider NLR a good predictor of OS, but without having a disease specificity (cancer or, more precisely, HNSCC)(17-18).
The potential of NLR variation during treatment (delta-NLR) to predict the evolution and response to treatment of different cancers remains controversial. NLR variation during treatment (delta-NLR) – representing posttreatment NLR minus pretreatment NLR – was associated with the rate of complete pathological response (pCR) after neoadjuvant chemotherapy (NACT) in breast cancer, as evidenced by data from 242 patients treated with NACT and then treated surgically. If, so far, the value of NLR nadir pretreatment has been identified as a factor associated with pCR, this study also demonstrates the association of delta-NLR<0 with an increased rate of pCR in NACT-treated breast cancer followed by surgery. Analyzing the data obtained from a group of 354 patients diagnosed with stage I-III colon cancer operated with curative intent, delta-NLR using preoperative NLR and postoperative NLR were evaluated as possible predictors of OS. The rate of OS at one, three and five years, if delta-NLR<0 and delta-NLR>0 was 98.2%, 90.7%, 83.6%, respectively 98.4%, 96.9% and 95.3%, the study thus demonstrating a favorable result for patients with delta-NLR>0. In the case of head and neck cancers, data on the dynamic and biomarker assessment of delta-NLR and delta-PLR variation are limited, but NLR before chemoradiotherapy has been associated with TNM according to AJCC stage and prognosis in the oral squamous cell carcinoma. A low value of NLR was associated with long survival in this case(19-21).
Analyzing a systematic review and meta-analysis including 6479 patients and 24 articles selected from 241, Mascarella et al. identified a median hazard ratio for OS of 1.78 in patients with HNSCC, with a minimum hazard ratio of 1.55 for laryngeal cancers and a maximum of 2.36 for hypopharyngeal cancers that had elevated NLR. Thus, the authors validate NLR before initiating treatment as a prognostic biomarker, an increased value being associated with therapeutic failure. Cho and colleagues identified three ranges of NLR values (<2.2, 2.2 to 6 and ≥6) as being associated with patient survival, with high NLR values being associated with increased OS(22-23).
Conclusions
NLR and PLR are easy to evaluate and calculate indexes, having, in terms of accessibility and low cost, the advantage as possible biomarkers. Their evolution is oscillating during the treatment course, which indicates a change in the inflammation/immune response balance, but the final value does not differ significantly from the nadir value. If there is strong evidence for the role of NLR nadir as a biomarker, the evaluation of NLR and PLR dynamics requires further research to confirm the possibility of being validated as a prognostic or predictive biomarker of response to chemotherapy and radiotherapy in HNSCC.
Bibliografie
-
Dahiya K, Dhankhar R. Updated overview of current biomarkers in head and neck carcinoma. World J Methodol. 2016;6(1):77-86.
-
Iancu DT, Iancu RI. Paranasal sinuses cancers – modern and actual considerations. Romanian Journal of Functional & Clinical, Macro- & Microscopical Anatomy & of Anthropology/Revista Româna de Anatomie Funcţională şi Clinică, Macro- şi Microscopică şi de Antropologie. 2016;15(Issue 1):68-75.
-
Iancu DT, Iancu RI. Oral cavity cancers – general review. Romanian Journal of Functional & Clinical, Macro- & Microscopical Anatomy & of Anthropology/Revista Româna de Anatomie Funcţională şi Clinică, Macro- şi Microscopică şi de Antropologie. 2015;14(Issue 4):610-618.
-
Mocanu V, Haliga R, Paduraru O, Baran D, Bădoi D, Iancu R, Oboroceanu T, Bălănica A, Bădescu M. A Diet Rich in Whole Grain Flaxseeds has Antithrombotic Effects Without Increasing Oxidative Stress in Experimental Atherosclerosis. Journal of Biologically Active Products from Nature. 2011;1(3):144-159.
-
Chicos A, Negura L, Brăescu R, Morariu A, Negura A, Chicos A, Lupaşcu C. High frequency of BRCA recurrent mutations in a consecutive series of unselected ovarian cancer patients. Revista Română de Medicină de Laborator. 2020 June;28(3):257-266.
-
Bădulescu F, Bădulescu A, Crişan A, Popescu FC. Study of the diagnosis and treatment of cancer located in the head and neck and correlation with expression of prognostic markers. Rom J Morphol Embryol. 2013;54(3):487-97.
-
Bădulescu F, Crişan A, Bădulescu A, Schenker M. Recent data about the role of human papillomavirus (HPV) in oncogenesis of head and neck cancer. Rom J Morphol Embryol. 2010;51(3):437-40.
-
Iancu DT, Iancu RI. Utilizarea simulatorului în determinarea planurilor de tratament şi definirea volumelor ţintă în radioterapie [Use of simulator in treatment planning and determination and definition of treatment volume]. Rev Med Chir Soc Med Nat Iaşi. 2004 Jul-Sep;108(3):580-3 [Romanian].
-
Costea I, Diaconescu MR, Terinte R, Glod M, Chiriac R, Bulimar V. Antibioticoprofilaxia în chirurgia cancerului colorectal [Antibiotic prophylaxis in surgery for colorectal cancer]. Rev Med Chir Soc Med Nat Iaşi. 2003 Jul-Sep;107(3):609-12 [Romanian].
-
Iancu D, Iancu R. Nivelele limfatice ale capului şi gâtului – aspecte anatomoclinice în radioterapia conformaţională [Nodal levels – anatomic and clinical correlations in conformal radiotherapy]. Rev Med Chir Soc Med Nat Iaşi. 2004 Apr-Jun;108(2):275-80 [Romanian].
-
Buzea CG, Agop M, Moraru E, Stana BA, Gîrţu M, Iancu D. Some implications of Scale Relativity theory in avascular stages of growth of solid tumors in the presence of an immune system response. J Theor Biol. 2011 Aug 7;282(1):52-64.
-
D’Souza G, Anantharaman D, Gheit T, Abedi-Ardekani B, Beachler DC, Conway DI, Olshan AF, Wunsch-Filho V, Toporcov TN, Ahrens W, Wisniewski K, Merletti F, Boccia S, Tajara EH, Zevallos JP, Levi JE, Weissler MC, Wright S, Scelo G, Mazul AL, Tommasino M, Cadoni G, Brennan P. Effect of HPV on head and neck cancer patient survival, by region and tumor site: A comparison of 1362 cases across three continents. Oral Oncol. 2016 Nov;62:20-27.
-
Szilasi Z, Jósa V, Zrubka Z, et al. Neutrophil-To-Lymphocyte and Platelet-To-Lymphocyte Ratios as Prognostic Markers of Survival in Patients with Head and Neck Tumours – Results of a Retrospective Multicentric Study. Int J Environ Res Public Health. 2020;17(5):1742.
-
Kim KY, McShane LM, Conley BA. Designing biomarker studies for head and neck cancer. Head Neck. 2014;36(7):1069-1075.
-
Bazzi WM, Dejbakhsh SZ, Bernstein M, Russo P. Neutrophil-lymphocyte ratio in small renal masses. ISRN Urol. 2014 Mar 12;2014:759253.
-
Takenaka Y, Oya R, Kitamiura T, Ashida N, Shimizu K, Takemura K, Yamamoto Y, Uno A. Platelet count and platelet-lymphocyte ratio as prognostic markers for head and neck squamous cell carcinoma: Meta-analysis. Head Neck. 2018 Dec;40(12):2714-2723.
-
Seetohul YB, Singh V, Jain RK, Chaudhary AK. Prognostic Value of Neutrophil-Lymphocyte Ratio and Platelet-Lymphocyte Ratio in Head and Neck Malignancies. Indian J Otolaryngol Head Neck Surg. 2020 Mar;72(1):128-132.
-
Bojaxhiu B, Templeton AJ, Elicin O, Shelan M, Zaugg K, Walser M, Giger R, Aebersold DM, Dal Pra A. Relation of baseline neutrophil-to-lymphocyte ratio to survival and toxicity in head and neck cancer patients treated with (chemo-) radiation. Radiat Oncol. 2018 Nov 6;13(1):216.
-
Dan J, Tan J, Huang J, Zhang X, Guo Y, Huang Y, Yang J. The dynamic change of neutrophil to lymphocyte ratio is predictive of pathological complete response after neoadjuvant chemotherapy in breast cancer patients. Breast Cancer. 2020 Sep;27(5):982-988.
-
Li Z, Zhao R, Cui Y, Zhou Y, Wu X. The dynamic change of neutrophil to lymphocyte ratio can predict clinical outcome in stage I-III colon cancer. Sci Rep. 2018;8(1):9453.
-
Sun W, Gao M, Hu G, Yuan X. Inflammatory Marker Predicts Outcome of Oral Squamous Cell Carcinoma Receiving Chemo-Radiotherapy. Cancer Manag Res. 2020;12:12329-12335.
-
Mascarella MA, Mannard E, Silva SD, Zeitouni A. Neutrophil-to-lymphocyte ratio in head and neck cancer prognosis: A systematic review and meta-analysis. Head Neck. 2018 May;40(5):1091-1100.
-
Cho JK, Kim MW, Choi IS, Moon UY, Kim MJ, Sohn I, Kim S, Jeong HS. Optimal cutoff of pretreatment neutrophil-to-lymphocyte ratio in head and neck cancer patients: a meta-analysis and validation study. BMC Cancer. 2018 Oct 11;18(1):969.
Articole din ediţiile anterioare
Preliminary results of markers as predictors for the tissue response to radiochemotherapy in rectal cancer
Radiochimioterapia preoperatorie (p-CRT) este o tehnică utilizată pe scară largă pentru tratarea cancerului rectal local avansat, a cancerului esof...
CT imaging biomarkers – clues to the cause of pericardial effusions focused on tumoral pathology
O gamă largă de factori sunt demonstraţi a determina apariţia epanşamentelor pericardice, inclusiv în cazul pacienţilor cu patologie tumorală c...
Can we achieve successfully local control by IMRT radiotherapy in the treatment of male breast cancer? A case report
Această prezentare descrie un caz rar de cancer mamar la un pacient de gen masculin, patologie care are o incidenţă mai mică de 1% din toate cazur...
Două mecanisme de creştere în greutate în timpul chimioterapiei cancerului de sân
Statistic, pacienţii care îşi menţin greutatea stabilă pe durata tratamentului cancerului de sân au cel mai bun prognostic. Iar cei care se îngraşă...