Cardiac tamponade is a state of hemodynamic compromise that results from heart compression by a variety of factors and conditions, including tumoral pericarditis or tumor cardiac compression. The aim of this article is to evaluate and discuss the added value of CT imaging findings of impending cardiac tamponade in patients with thoracic and hematologic malignancies. We reviewed our database for a period of six years, between January 2015 and April 2021, and we selected five patients with clinical, hemodynamic state and CT imaging features of cardiac tamponade in oncologic pathology, four of them diagnosed with hematologic malignancies. We included postradiotherapy pericardial complications in the case of one patient. Although echocardiography represents the modality of choice to diagnose patients with suspected cardiac tamponade, computed tomography can provide valuable and supplementary information regarding the extension of the tumoral pericardial involvement or the type of pericardial effusion. Considering that the early diagnosis of an impending cardiac tamponade and the treatment are crucial in preventing mortality and poor outcomes, radiologists have an important role in recognizing this entity.
Aspecte imagistice în sindroamele compresive pericardice – tamponada cardiacă în patologia oncologică
Imaging of pericardial compressive syndromes – cardiac tamponade in oncologic patients
First published: 24 aprilie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.55.2.2021.5015
Abstract
Rezumat
Tamponada cardiacă reprezintă alterarea statusului hemodinamic, produsă prin compresia cardiacă determinată de o varietate de factori şi afecţiuni, inclusiv pericardita tumorală şi compresia tumorală cardiacă. Obiectivul acestui articol este de a evalua şi discuta aportul examenului CT în tamponada cardiacă iminentă în cazul patologiei tumorale intratoracice şi hematologice. Am revizuit baza noastră de date pe o perioadă de şase ani, între ianuarie 2015 şi aprilie 2021, şi am selectat cinci pacienţi cu tablou clinic, status hemodinamic şi imagistică CT sugestive pentru tamponadă cardiacă în patologia oncologică, patru dintre pacienţi prezentând patologie tumorală hematologică. Am inclus un pacient cu patologie pericardică secundară radioterapiei. Deşi ecocardiografia reprezintă metoda de elecţie în cazul pacienţilor cu suspiciune de tamponadă cardiacă, examinarea computer-tomografică oferă informaţii importante şi suplimentare legate de extensia pericardică a proceselor tumorale sau de tipul epanşamentului pericardic. Luând în considerare că diagnosticul şi tratamentul cât mai rapid ale unei iminente tamponade cardiace sunt extrem de importante în reducerea mortalităţii şi în îmbunătăţirea prognosticului bolii, radiologii au un rol major în recunoaşterea acestei entităţi.
Introduction
Cardiac tamponade represents a life-threatening condition characterized by impaired ventricular filling with decreased cardiac output and hemodynamic instability caused by fluid accumulation in the pericardial sac or cardiac tumor compression(1,2,3). It can occur as initial presentation of an unknown malignancy or in patients with established tumoral pathology(4). Pericardial effusion in oncologic patients can be secondary to tumor extension/metastases(5,6), may develop as a complication to radiation and chemotherapy(4), or in case of opportunistic infections(5). CT imaging features of cardiac tamponade in oncologic patients include: anterior heart compression by a mediastinal tumor or loculated/large pericardial effusion(5), angulation and bowing of the interventricular septum(2), enlargement of SVC and IVC (with diameter larger than the one of thoracic aorta)(6), reflux of contrast material into the IVC or azygos vein, periportal edema(1), compression of the coronary sinus(7). CT evaluation can provide valuable information regarding the tumoral pericardial involvement and extension, and the type of pericardial effusion(2).
Materials and method
We made a retrospective study for a period of six years (between January 2015 and April 2021), and we selected 119 oncologic patients with signs of pericardial disease, five patients with clinical, hemodynamic and CT imaging findings suggestive for cardiac tamponade. CT imaging was performed on 16 or 64 multidetector (MD) CT scanners in all cases, with one non-enhanced CT phase (NECT), to measure attenuation values of the pericardial colection and two phases in arterial (25 seconds) and delayed phase (100 seconds) post iodinated contrast material injection, at the injection ratio of 2-3 ml/s, in a quantity of approximately 1-1.5 ml/kg b.w., to evaluate pericardial thickness and enhancement, neoplastic pericardial involvement and heart structural anomalities. The physical parameters used for CT consisted in axial thickness slices of 5 mm, with 1.25 or 1.5 mm reconstruction interval. Different planes reconstructions (coronal, sagittal, oblique views) have been performed in order to have an optimal visualization of the cardiovascular structures.
Results
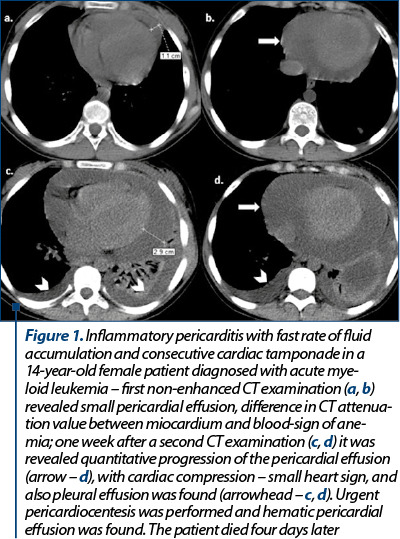
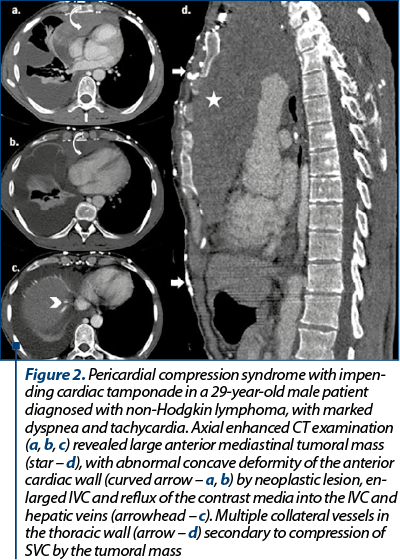
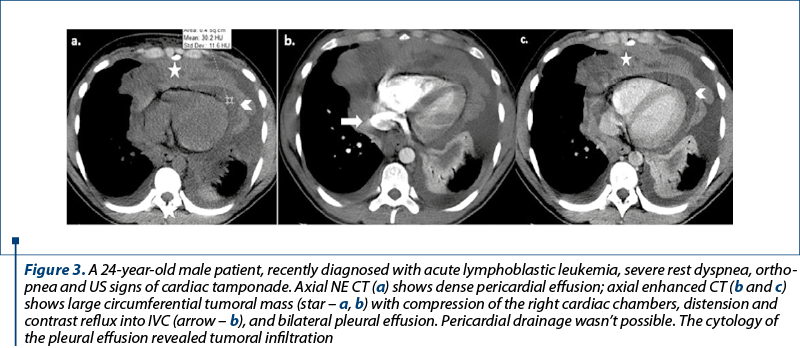
We selected five cases of oncologic patients (two females and three males), with ages between 14 and 50 years old, all patients with clinical, hemodynamic and CT imaging findings suggestive for cardiac tamponade. Among our patients, one female patient was diagnosed with breast cancer and the other four patients were diagnosed with hematologic malignancies (one case with acute myeloid leukemia, one case with acute lymphoblastic leukemia, one case with Hodgkin lymphoma, and one case with non-Hodgkin lymphoma). Large pericardial effusion with attenuation values between 12 and 24 UH caused cardiac compression and consecutive cardiac tamponade in three patients, and in one case pericardiocentesis revealed hemopericardium – Case 1, Figure 1. Structural heart compression by a large mediastinal tumor was found in two patients (Case 2, Figure 2, and Case 3, Figure 3), with anterior heart compression, deformity and concave appearance of the anterior cardiac wall (Case 2, Figure 2, curved arrow – a, b) and small heart sign (Case 3, Figure 3). Indirect signs of cardiac tamponade with the enlargement of SVC and IVC (with diameter larger than the one of thoracic aorta) were found in all cases. In three cases, reflux of contrast material into the IVC or hepatic veins was noted (Case 2, Figure 2, arrowhead – c). Bowing of the interventricular septum and marked coronary sinus compression, although considered important imaging signs in cardiac tamponade, were not seen in our patients. In one case, we found associated the superior vena cava syndrome.
Discussion
Cardiac tamponade represents a life-threatening condition, the oncologic patients with cardiac tamponade caused by malignant disease having death rates exceeding 75% within 12 months(8). In oncologic patients, cardiac tamponade can be secondary to heart compression by a large pericardial effusion(4,5) or by an invasive cardiopericardial tumor with no evidence of pericardial effusion(2). Pericardial effusion in oncologic patients can be secondary to tumoral invasion of the pericardium, as side effect to the radiation and chemotherapy, or to opportunistic infections(9). Dyspnea, cough and chest pain are the most frequent symptoms of impending cardiac tamponade(4). Beck’s triad, with increased jugular vein distension, small and silent heart and hypotension, is rarely encountered in case of tumoral pericarditis(9,10). In our patients, moderate to severe dyspnea was the most frequent symptom. Electrocardiography most often reveals ST-T changes and low QRS voltages(4,11); in our patients, three of them presented ST-T changes and tachycardia. CT imaging signs suggestive for an impending cardiac tamponade are: cardiac compression by pericardial effusion, more common with fast fluid accumulation(1) (Case 1, Figure 1), flattened heart – anterior heart compression by a mediastinal tumor (Case 3, Figure 3), deformity with reduction of the anteroposterior cardiac diameter (Case 2, Figure 2) loculated/large pericardial effusion – in three of our patients (Case 1), angulation and bowing of the interventricular septum(2), enlargement of SVC and IVC (with diameter larger than the thoracic aorta) – seen in all our patients, reflux of contrast material into the IVC or azygos vein (Case 2, Figure 2; Case 3, Figure 3). According to literature, compression of the coronary sinus(7) and bowing of the interventricular septum(2), described as another signs of impending cardiac tamponade, were not seen in our patients’ CT examinations. Based on attenuation measurement, CT provides information about the posible nature of the pericardial effusion(2); high density values and a density greater than that of skeletal muscle suggest haemorragic pericarditis(12). All these imaging findings, in the presence of a large pericardial effusion, can strongly suggest an impending cardiac tamponade(2), therefore timely therapeutic intervention is mandatory in oncologic patients in proper clinical scenarios.
Conclusions
Although a rapid assessment of patients with clinical signs of impending cardiac tamponade is best made with echocardiography, in malignancies CT examinations provide valuable and supplementary information regarding the tumoral pericardial involvement and extension, the type of pericardial effusion and cardiac structural changes, with implications for the therapeutic choice regarding the opportunity of pericardiocentesis or pericardiectomy.
Bibliografie
-
Guimaraes M, et al. Imaging acute complications in cancer patients: what should be evaluated in the emergency setting? Cancer Imaging. 2014;14(1):18.
-
Restrepo CS, et al. Imaging findings in cardiac tamponade with emphasis on CT. Radiographics. 2007;27(6):1595-1610.
-
De Potter B, et al. Imaging of urgencies and emergencies in the lung cancer patient. Insights Imaging. 2018;9(4):463-476.
-
Halfdanarson TR, et al. Emergencies in Hematology and Oncology. Mayo Clin Proc. 2017;92(4):609-641.
-
Kathabathina VS, et al. Nonvascular, nontraumatic mediastinal emergencies in adults: a comprehensive review of imaging findings. RadioGraphics. 2011;31(4):1141-1160.
-
Maggiolini S, et al. The role of early contrast-enhanced chest computed tomography in the aetiological diagnosis of patients presenting with cardiac tamponade or large pericardial effusion. European Heart Journal – Cardiovascular Imaging. 2016 Apr;17(4):421–428.
-
Gold MM, et al. Coronary sinus compression: an early computed tomographic sign of cardiac tamponade. J Comput Assist Tomogr. 2008 Jan-Feb;32(1):72-7.
-
Stashko E, Meer JM. Cardiac Tamponade. [Updated 2020 Nov 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431090/
-
Shenoy S, et al. Cardiovascular Oncologic Emergencies. Cardiology. 2017;138:147-158
-
Roy CL, et al. Does this patient with a pericardial effusion has cardiac tamponade? JAMA. 2007 Apr 25;297(16):1810-8.
-
Adler Y, et al. European Society of Cardiology (ESC). 2015 ESC guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC). Endorsed by the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015 Nov 7;36(42):2921-64.
-
Peebles CR, et al. Pericardial disease – anatomy and function. The British Journal of Radiology. 2011;84 Spec no 3(Spec Iss 3):S324-37.
Articole din ediţiile anterioare
Constipaţia indusă de opioide
Opioidele, prescrise de medicii oncologi şi de cei de îngrijire paliativă pentru uşurarea durerii din cancer, au efecte secundare multiple, co...
Ocular toxicity of biological therapy in solid tumors
Cancerul este principala cauză de mortalitate în lume, cu peste 10 milioane de decese anual. Tratamentele medicale clasice, chimioterapia şi radio...
Abstracts for IOB Scientific DayS, 17-19 MAY 2018
Abstracts for IOB Scientific DayS, 17-19 MAY 2018
Radioterapia stereotactică - principii şi aspecte practice
Radioterapia stereotactică este o formă de iradiere externă care distribuie într-o şedinţă unică sau în câteva şedinţe doze mari de iradiere în vol...