Aspecte tehnologice în confecţionarea gutierelor cu utilizare dentară (Partea a II-a)
Technological aspects in the manufacturing of custom-fitted mouthguard (Part II)
Abstract
In this material, the importance of custom-fitted mouthguard is highlighted, because they are used in almost all specialties related to dentistry, including orthodontics and dental prosthetics, being used to solve as many problems as possible, such as: relaxing the TMJ muscles, correcting TMJ disorders, preserving and especially maintaining the position of the teeth after the orthodontic treatment, protection during performance sports, teeth whitening etc.Keywords
custom-fitted mouthguardtemporomandibular jointdentistryRezumat
În acest material, am încercat să evidenţiem importanţa gutierelor dentare, deoarece acestea sunt utilizate în aproape toate specialităţile aferente stomatologiei, inclusiv în ortodonţie şi în protetica dentară, fiind întrebuinţate în rezolvarea cât mai multor probleme, cum ar fi: relaxarea musculaturii ATM, corectarea tulburărilor ATM, păstrarea şi mai ales conservarea poziţiei dinţilor după tratamentul ortodontic, protecţie în timpul practicării unui sport de performanţă, albirea dinţilor etc.Cuvinte Cheie
gutiere dentarearticulaţie temporomandibularăstomatologieIntroduction
Mouthguards have multiple uses. They are used with great efficiency both in orthodontics and dentofacial orthopedics to preserve the therapeutic result, in prosthetic practice for the therapy of bruxism phenomena (it has the role of protecting and repositioning the dental structures), and for performing teeth whitening procedures (support role for substances used for teeth whitening)(1-4). However, the main benefit of mouthguards is the fact that they balance the distribution of occlusal forces to all components of the masticatory system. They can reduce the frequency, but not the intensity, of parafunctional episodes, and they act to prevent the complications determined in the dentomaxillary area(1-4).
The situations in which the use of mouthguard is indicated are(1-4):
-
after the orthodontic treatment
-
for teeth whitening
-
in the case of patients with bruxism
-
in patients who practice various sports, especially contact sports
-
within complex dental treatments, with a diagnostic role.
In the second part of this article, the readers’ attention will be directed to several novel aspects that intervene in the technological flow of manufacturing mouthguards that must be used by patients with bruxism, as well as mouthguards for use in orthodontic practice.

Case presentations
Occlusal splint (night guard) – protective device for patients with bruxism
A 38-year-old patient presented himself in the dental office, where he was diagnosed with bruxism. The dentist, in agreement with the patient, decided to make a mouth guard for the treatment of bruxism.
The materials and equipment used to fabricate night guards are: 1.5-mm soft thermoplastic film (it has a soft surface and a hard surface); device for heating thermoplastic films (Song Young model); materials (type II and type III dental stone, bowl and spatula for mixing the plaster, vibrating table); equipment and tools for processing and polishing (dental technique motor, burrs, disc, fluff etc.); special box for packaging and transport. To all these, written and/or verbal instructions for the use and storage of the night guard must be added.
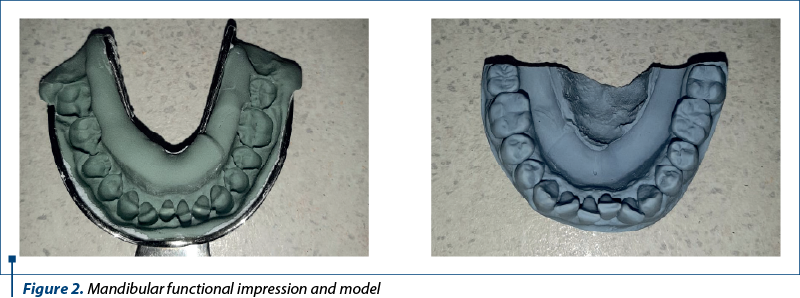
In a first stage, the functional impression of the mandibular arch was taken, using a standard impression tray and a condensation silicone material of putty consistency. The impression has the role of registering the entire mandibular prosthetic field of the patient. Before being sent to the dental laboratory, the impression is washed under running tap water for 15 seconds and then decontaminated by immersion in a disinfectant solution based on quaternary ammonium salts, following the manufacturer’s instructions. Afterwards, the impression is sent to the technical department, where the dental technician manufactures the functional model (working model). The working model was cast using type III dental stone and the instruments and equipment previously presented.
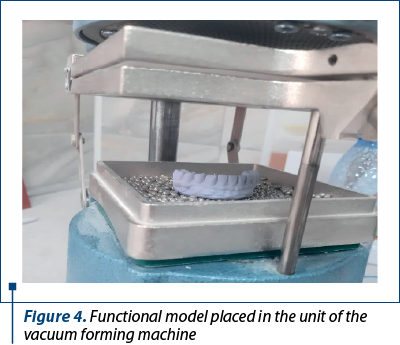
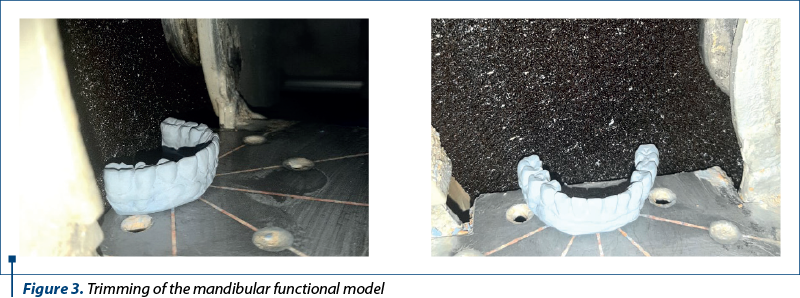
After trimming, the functional model is placed in the middle of the vacuum forming machine support. The foil is heated till the indicated thermoforming temperature at which is lowered on the functional model for the thermoforming process.

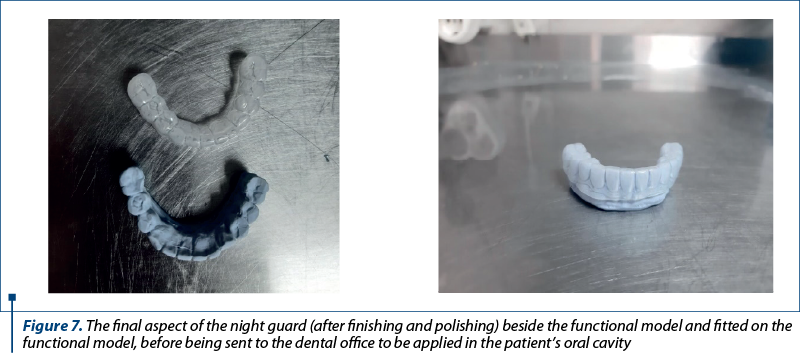
After removing the foil from the vacuum forming machine, it shows excess material, which will be removed using finishing discs and burrs. After removing the excess material, the night guard will be polished and finished so that it has a smooth glossy appearance with round edges in order not to damage the patient’s oral mucosa. In the end, the night guard will be washed, disinfected, packed and sent to the dental office for try in.

Thermoplastic retainer – orthodontic retention device
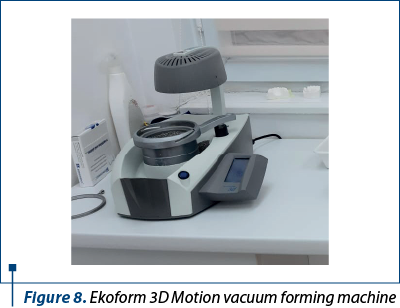
A 30-year-old patient presented herself in the dental office at the end of orthodontic treatment with a fixed appliance. In agreement with the patient, the orthodontic specialist decided to make a thermoplastic retainer to maintain the orthodontic result. As materials and equipment used for manufacturing the retainer, the following should be mentioned: thermoplastic foil, orthodontic plaster, Ekoform 3D Motion vacuum forming machine, bowl and spatula for mixing the plaster, vibrating table, equipment and tools for processing and polishing (dental technique motor, burs, disc, fluff etc.); special box for packaging and transport. To all these, written and/or verbal instructions for the use and storage of the retainer must be added.
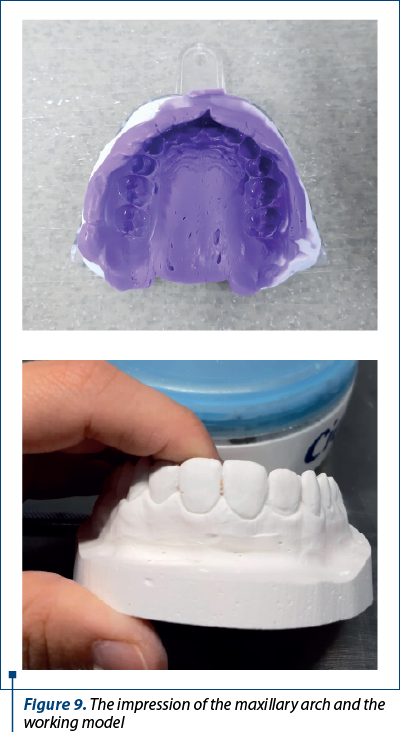
After the functional impression of the maxillary arch in two steps, with the help of a standard impression tray using addition silicone materials in double consistency, putty and light body, the impression was sent to the technical compartment, where the dental technician obtained the working model. Previously, before being sent to the dental laboratory, the impression was washed and decontaminated in disinfectant, following the manufacturer’s instructions. The working model was cast using type III orthodontic plaster.
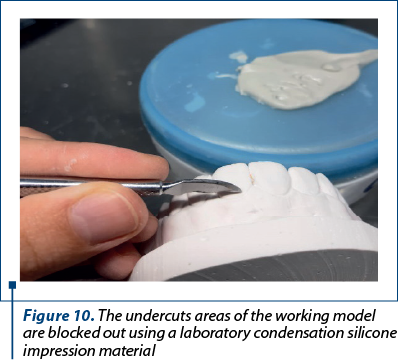
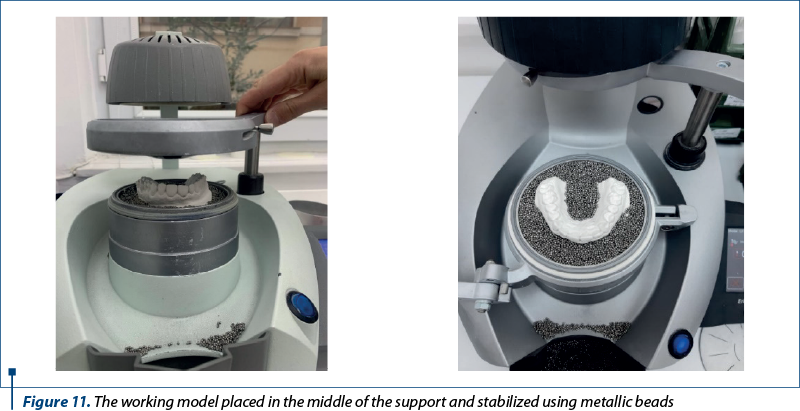
The working model is placed on the support of the Ekoform 3D Motion device. The model will be positioned so that it does not change position during the application and molding of the thermoplastic film. The beads from the support of the vacuum forming machine have the role of stabilizing the working model. The heating of the thermoplastic foil will begin, the device will announce the moment when the foil reaches the optimum temperature, and the molding process should begin. Using vacuum, the foil is molded on the working model.
An extra hard bur is used to remove the excess material. The retainer is processed on the gingival line of the tooth or as close as possible to it, depending on the requirements of the orthodontic specialist. During processing, it is taken into account that the retainer does not have sharp edges, but rounded, so as not to cause discomfort and injuries to the patient.
Discussion
The use of occlusal splints was first specified in the literature in 1901 by Dr. Karolyi (Vienna)(5,6). Since that time, clinical and technical research has led to the development of different types of materials for obtaining occlusal splints (night guards). For a long period of time, occlusal splints were made of acrylic materials, mainly on the maxillary arch, to reduce the patients’ discomfort(7,8). However, acrylate is a rigid material that cannot take the occlusal pressures present in bruxism. The use of slightly elastic materials appeared in the early ’90s through the use of thermoplastic materials(9). They present a degree of rigidity that allows the manufacturing of small-volume occlusal splints, which brings superior comfort to patients, but with a thickness that can be controlled by the thickness of the thermoplastic film.

The appearance and use of thermoplastic foils for the treatment of bruxism created the opportunity to develop and use similar devices in maintaining the results obtained following the orthodontic treatment. If initially fixed tooth retainers were used after orthodontic treatment(10-12), thermoplastic retainers were used to reduce discomfort, worn by the patient especially at night. The use of these materials is not yet at a high level. In a recent study by Hamran et al. (2022), among orthodontists in Scandinavian countries, they found that the most used retainers were the fixed one, used on the maxilla and/or mandible, while thermoplastic retainers were used only on the maxillary(13). This study also showed that only six respondents reported adverse effects to the thermoplastic material(13).
As in the case of bruxism occlusal splints, the biggest problem is related to the resistance over time of the material which, due to wear, at some point gives way and requires replacement of the retainer. Grünheid and Bitner, in a study carried out in 2023(14), that was based on the analysis of the degree of wear for thermoplastic retainers made of three different materials in tests that simulated the use equivalent to a year, concluded that, in normal use, the retainers get a degree of wear less than 0.2 mm, but no fractures appear in the mass of the material(14-22).
Conclusions
This article highlights the importance of mouth guards, as they are used in almost all specialties related to dentistry, including orthodontics and dental prosthetics, being used to solve as many problems as possible, such as:
-
reducing stress in the TMJ muscles
-
correction of TMJ disorders
-
retaining the position of the teeth after the orthodontic treatment
-
protection while practicing a performance sport
-
teeth whitening
-
occlusion correction
-
orthodontic treatment.
The manufacturing process for mouth guards is not expensive, does not present a complex technological flow, and it requires a short production time.
It should also be highlighted that the patient must be very well informed about how to use and store the mouth guards.
Thus, it is more than necessary to know all the information related to mouth guards, information on aspects such as the role, the importance, the method of manufacturing, but also the indications and contraindications, the use and storage.
Acknowledgement: Viorel Ştefan Perieanu and Bogdan Alexandru Dimitriu are corresponding authors (Viorel Ştefan Perieanu: viorelperieanu@yahoo.com; Bogdan Alexandru Dimitriu: bogdan.dimitriu@umfcd.ro). Irina-Adriana Beuran and Radu-Cătălin Costea have equally contribution with the first author.
Corresponding authors:
Viorel Ştefan Perieanu
E-mail: viorelperieanu@yahoo.com;
Bogdan Alexandru Dimitriu
E-mail: bogdan.dimitriu@umfcd.ro
Conflict of interest: none declared.
Financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.
Bibliografie
- Cristache CM, Bunea I, Şelaru EP. Albirea dentară între mit şi realitate – Scurt review. Dental Target. 2016;11(38):10-16.
- Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35(7):476-94.
- Ojovan A, Burlacu V, Cartaleanu A, Cuşnir A, Bălan E. Optimizarea alegerii tratamentului în hipersensibilitatea ţesuturilor dure ale dintelui. Medicina stomatologică. 2010;16(3):62-64.
- Frazier KB, Haywood VB. Teaching nightguard bleaching and other tooth-whitening procedures in North American dental schools. J Dent Educ. 2000;64(5):357-64.
- Karolyi M. Beobachtungen über Pyorrhea Alveolaris. Oesterreich-Ungarische Vieteljahrsshrift für Zahnheilkunde. 1901;17:279-83.
- DuPont JS Jr, Brown CE. Occlusal splints from the beginning to the present. Cranio. 2006;24(2):141-5.
- Kass CA, Tregaskes JN. Occlusal splint fabrication. J Prosthet Dent. 1978;40(4):461-3.
- Lundeen TF. Occlusal splint fabrication. J Prosthet Dent. 1979;42(5):588-91.
- Weinberg LA. A new material and technique for appliance therapy. N Y State Dent J. 1989;55(1):36-8.
- Zachrisson BU. Clinical experience with direct-bonded orthodontic retainers. Am J Orthod. 1977;71(4):440-8.
- Diamanti-Kipioti A, Gusberti FA, Lang NP. Clinical and microbiological effects of fixed orthodontic appliances. [Erratum in: J Clin Periodontol 1990 Jan;17(1):66].
- J Clin Periodontol. 1987;14(6):326-33.
- Artun J, Spadafora AT, Shapiro PA, McNeill RW, Chapko MK. Hygiene status associated with different types of bonded, orthodontic canine-to-canine retainers. A clinical trial. J Clin Periodontol. 1987;14(2):89-94.
- Hamran T, Čirgić E, Aiyar A, Vandevska-Radunovic V. Survey on retention procedures and use of thermoplastic retainers among orthodontists in Norway, Sweden, and Denmark. J World Fed Orthod. 2022;11(4):114-119.
- Grünheid T, Bitner TF. Wear and fatigue resistance: An in vitro comparison of three polyethylene terephthalate glycol and thermoplastic polyurethane materials for vacuum-formed retainers. Int Orthod. 2023;21(2):100748.
- Bodnar DC, Dimova C, Bodnar T, Cristache CM, Burlibaşa M, Sfeatcu R. Dental management of patient with psychiatric disorders. Modern Medicine. 2010;17(10):538-543.
- Burlibaşa M, Burlibaşa L, Gavrilă LB, Gavrilă VR, Gavrilă L. microRNA a macro revolution in medical biotechnologies. Roum Biotech Lett. 2008;13(6):3977-3983.
- Bodnar DC, Pantea M, Bodnar T, Burlibaşa M, Dumitru SG, Cristache CM. Patologia mucoasei orale la pacienţii vârstnici – studiu clinico-statistic. Acta Medica Transilvanica. 2012;2(2):56-60.
- Cristache CM, Totu EE, Burlibaşa M, Tănase G, Iorgulescu G, Burlibaşa L. Preliminary study on genotoxicity assessment of an innovative topical treatment for periodontal disease. Revista de Chimie. 2020;71(2):145-150.
- Totu EE, Cristache CM, Perieanu VS, Burlibaşa M, Petre DC, Burlibaşa L. Are nano TiO2 inclusions improving biocompatibility of photocurable polydimethylsiloxane for maxillofacial prothesis manufacturing?. Applied Sciences. 2021;11(9):3777.
- Totu EE, Cristache CM, Isildak I, Yldirim R, Burlibaşa M, Nigde M, Burlibaşa L. Citotoxicity and genotoxicity assessment of the PMMA-TiO2 nanocompozites for stereolithographic complete dentures manufacturing. Revista de Chimie. 2018;69(5):1160-1165.
- Burlibaşa M, Cristache CM, Georgescu SR, Dumitriu AS, Neamţu R. Toxicity of titan and nikel-cobalt-chromium alloys. Metalurgia International. 2009;14:20-22.
- Cristache CM, Burlibaşa M, Tănase G, Niţescu M, Neamţu R. Titanium as dental implant material. Metalurgia International. 2009;14:14-16.



