Lamboul bicoronal în traumatologia craniofacială
Bicoronal approach in craniofacial traumatology surgery
Abstract
Orbital and cranial bone traumas are considered medical and surgical emergencies and the surgical treatment should be considered immediately. The bicoronal flap offers a wide exposure to the frontal and temporal regions and the upper and middle face. Furthermore, the craniofacial bone fracture sites are clearly exposed and the aesthetic impairment is minimal.Keywords
bicoronal flaporbit fracturecraniofacial traumaRezumat
Leziunile calvariei şi orbitei din traumatologia craniofacială reprezintă urgenţe medico-chirurgicale, adeseori timpul chirurgical trebuind să fie de primă intenţie. Lamboul bicoronal reprezintă un abord chirurgical ce facilitează expunerea adecvată a regiunilor frontotemporale şi etajelor superior şi mijlociu ale feţei. De asemenea, focarele de fractură din traumatismele craniofaciale sunt bine evidenţiate, cu un prejudiciu estetic postoperatoriu minimal.Cuvinte Cheie
lambou bicoronaltraumatism craniofacialetaj superior facialIntroduction
The main goals of craniofacial trauma surgery are anatomical bone reduction and rigid fixation, along with ad integrum restitution of functions with minimal morbidity. These can be achieved by a proper surgical exposure and access.
The bicoronal flap was initially introduced in neurosurgery at the beginning of the last century, but the eminent surgeon Tessier(1) made it popular in the early 1970s in the field of craniofacial surgery, in craniostenosis management.
There are two main goals in the management of craniofacial trauma: a minimal morbidity and the restitution of the biologic and mechanical architecture of the facial structure. Initially, the bicoronal flap was used for treating frontal nasal complex fracture, and was later extended for the trauma management of the frontal bone, roof of the orbit, and zygoma complex.
The design of the flap depends on the hair line insertion. When dealing with male partial bald patients, a careful planning should be taken into consideration and the incision should be placed 3-4 centimetres further posterior. Depending of the region involved, the incision can be extended inferiorly pre- or postauricular to access the temporomandibular joint space or the zygoma bone. In order to achieve better flap reposition, the design of the flap can be modified into a step ladder, zigzag, saw tooth or sinusoidal(2).
The main advantage of the bicoronal flap is the wide exposure of the frontal, parietal and temporal regions and the upper and middle face, necessary in trauma, congenital malformation, and reconstructive surgery, with a good aesthetic outcome.
Case 1
A 30-year-old patient was admitted in the intensive care unit (ICU), transferred from a district hospital, diagnosed with severe politraumatism due to a road accident (the motorcycle driver not wearing safe equipment).
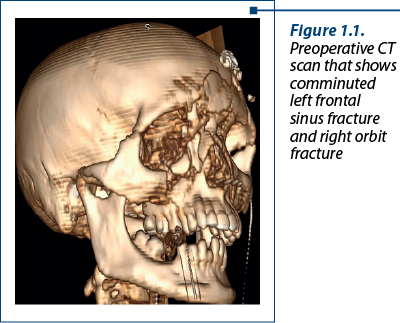
After a careful clinical and imagistic examination, the patient was diagnosed with multiple comminuted fractures of the face: anterior left frontal sinus, right inferior orbital rim, right floor of the orbit (Figure 1.1). Also, there were signs of cerebral oedema, subcortical haemorrhagic contusions, bilateral inflammatory injury of the posterior lung segments, and bilateral liquid collections in the pleura.
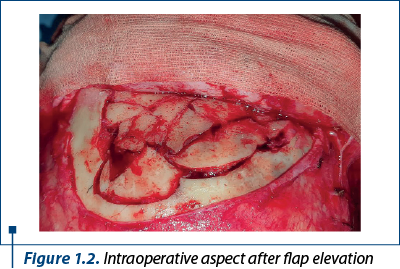
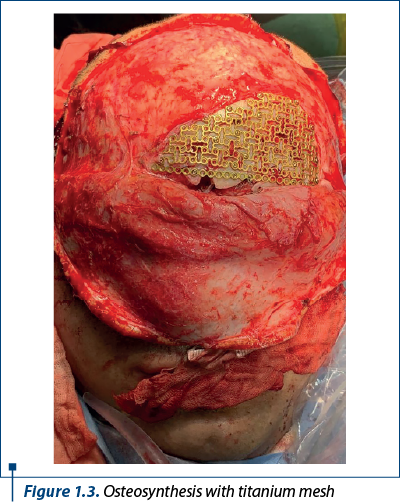
After an almost total resolution of the haemorrhagic cerebral lesions and of the inflammatory pathology of the lungs, a surgical procedure could be initiated. A bicoronal flap was necessary in order to gain access to the left frontal region, where a comminuted frontal sinus and upper orbital rim fracture was observed (Figure 1.2). The fractures were reduced and rigidly fixed with a titanium mesh tailored to the fracture site (Figure 1.3). An infraorbital incision was conducted for the exposure of the right inferior orbital rim; the bone fragments were reduced and fixed with titanium mesh and plates.
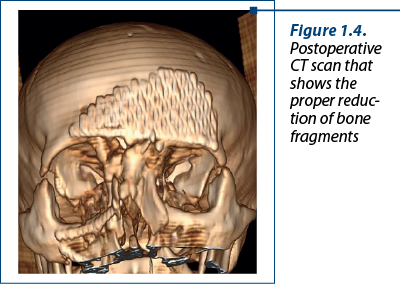
After surgery, a CT scan was conducted, revealing the anatomic reduction of the fracture sites (Figure 1.4).
The prognosis was favourable and the patient was recommended for clinical follow-up.
Case 2
A 34-year-old patient was admitted in our department with craniofacial trauma during a football competition that took place two weeks prior to the admission. The patient noted that he had been unconscious for a short period after the incident.
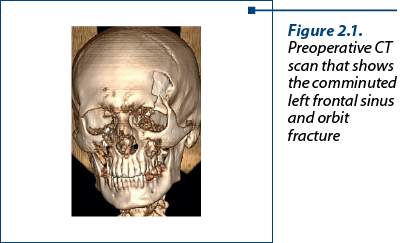
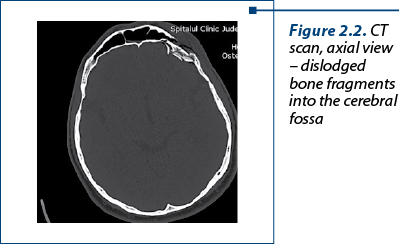
After a careful clinical and imagistic examination, the patient was diagnosed with multiple comminuted fractures of the frontal sinus (Figure 2.1), both the anterior and posterior cortex were involved, with two bone fragments being dislocated in the anterior cerebral fossa (Figure 2.2). The roof of the left orbit presented a comminuted fracture.
A team of maxillofacial surgeons and neurosurgeons was assembled.
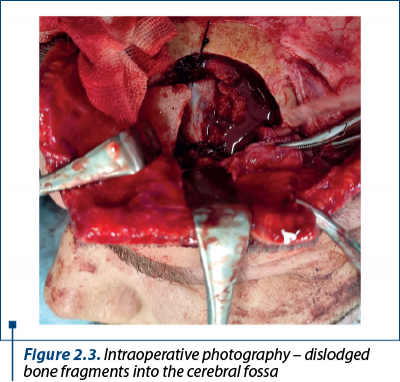
In order to get access to the frontal region, a bicoronal flap was performed. The fracture site was visualised and the anterior bone fragments were temporary removed from the site. The posterior dislocated fragments were then observed (Figure 2.3) and, after a careful dissection, they were taken away from the cerebral fossa. The dura mater was not injured and a couple of suspension sutures were placed by the neurosurgeon. The anterior cortex of the frontal bone was methodically reconstructed; the bone fragments were aligned and fixed with titanium miniplates. The bone fragments from the roof of the orbit were reduced in the right position and rigid fixation was applied (Figure 2.4).

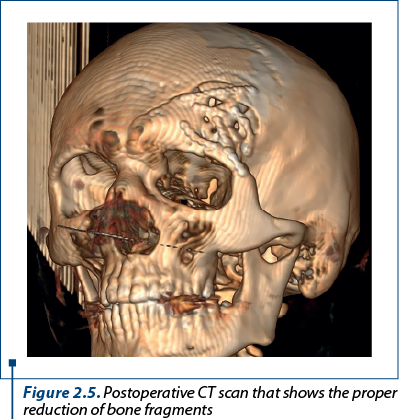
After surgery, a CT scan was conducted, showing the anatomic reduction of the fracture sites (Figure 2.5).
The prognosis was favourable and the patient was recommended for clinical follow-up.
Discussion
The bicoronal flap allows for an adequate exposure of the frontal calvaria and the upper and middle face.
In order to obtain a good haemostasis of the surgical site, a vasoconstrictor such as adrenaline can be delivered in a subgaleal plane.
The classic incision starts in the helix region, ascends coronal to the vertex and descends to the opposing helix. The incision is usually placed 3 to 4 centimetres behind the hair line.
In order to gain access to the zygoma or the temporomandibular joint, the incision can be extended pre- or retroauricular.
When dealing with trauma of the inferior orbital rim or floor of the orbit, infraorbital or transconjunctival incisions are associated. For tripod fixation of the zygoma bone, the surgical access can be gained by intraoral incisions.
For bone exposure of the frontal sinus region, orbit or the NOE complex, after flap elevation, the periosteum is incised approximately 3 centimetres cranial to the superior orbital rim and a periostal flap is elevated downwards which later will cover the fracture site and the osteosynthesis materials.
The incision for bicoronal flap is usually a straight line, but it has one main disadvantage: it can cause hair loss on the surgical scar. In order to avoid this, a modification can be made to the incision design, turning it from a line into a zigzag. Of course, this can lead to a relative lengthening of the surgical time, but besides the improved cosmetic appearance, the suture time is more precise with the step pattern of the incision. Also, there is no need in shaving the patient’s head, which can sometimes cause a psychological distress.
Postoperative alopecia(4) is a direct consequence of hair follicle injury. It can also occur when there is prolonged ischemia due to a more extensive surgical time. The risk of alopecia at the scar line can be diminished by more restricted electrocoagulation and an incision design parallel with the hair follicles. Improper scar formation and alopecia can be triggered even when using fine needle electrocoagulation such as the Colorado tip. Some authors suggest than even the Raney clips can cause hair follicle injuries in prolonged surgeries(4).
The neurological complications are considered the most important in bicoronal approach. They can occur by injury to the supraorbital, supratroheali nerves or the superior branches of the facial nerve. A careful anatomic knowledge of the surgical site can help preserve the supraorbital nerve structures. In order to avoid facial nerve damage, a subfascial dissection in the temporal muscle region can be carried when accessing the zygoma bone. If paralysis occurs even in these cases, it’s more likely due to flap manipulation and postoperative oedema, and it will resolve in time.
Injury to the supraorbital or supratroheali nerves can lead to sensory impairment or anaesthesia of the frontal skin. Once they are isolated in the surgical site, these structures can be preserved by releasing them from their bone orifices using hand instruments such as osteotom or rotary instruments like diamond burs(5).
There is a risk area for damaging the superior branch of the facial nerve, located between the lateral edge of the eyebrow and the tragus (roughly 2 centimetres above the orbit). When conducting a dissection in the temporal area in order to reach the zygoma, a diagonal incision in the temporal fascia should be preferred above that line(6).
Haematoma and infections should be considered rare complications, caused more likely by the improper handling of the flap than by the pattern of the flap itself. In order to reduce haematoma formation, an active drain should be placed, that can be usually removed after two or three days.
Palpebral ptosis and epiphora are rare complications, caused by unaddressed or improperly managed NOE complex fractures. Trismus is rarely seen, rather being a result of posttraumatic oedema.
Conclusions
The bicoronal flap with or without a pre-/retroauricular extension assures the optimal surgical site exposure in craniofacial trauma. It also provides good access to donor site for bone plates or fascia flap transfer when dealing with tissue loss. From an aesthetic point of the view, because it can be hidden between the hair lines, it represents the best choice in the management of upper face fractures.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
- Tessier P, Guiot G, Derome P. Orbital hypertelorism. II. Definite treatment of orbital hypertelorism (OR.H.) by craniofacial or by extracranial osteotomies. Scand J Plast Reconstr Surg. 1973;7(1):39–58.
- Frodel JL, Mabrie D. Optimal elective scalp incision design. Otolaryngol Head Neck Surg. 1999; 121(4):374-377.
- Fox AJ, Tatum SA. The coronal incision. Archives of Facial Plastic Surgery. 2003 May;5(3):259-262. http://doi.org/10.1001/archfaci.5.3.259
- Kadakia S, Badhey A, Ashai S, Lee TS, Ducic Y. Alopecia Following Bicoronal Incisions. JAMA Facial Plast Surg. 2017;19(3):220-224.
- Mishra M, Singh G, Singh H, Tewari A. Bicoronal Approach in Correction of Post-traumatic Frontal Bone Deformity: Report of Two Cases. The Traumaxilla. 2019;1(1):38-41.
- Kumar VS, Rao NK, Mohan KR, et al. Minimizing complications associated with coronal approach by application of various modifications in surgical technique for treating facial trauma: A prospective study. Natl J Maxillofac Surg. 2016;7(1):21-28.
- Rajmohan S, Tauro D, Bagulkar B, Vyas A. Coronal/Hemicoronal Approach – A Gateway to Craniomaxillofacial Region. J Clin Diagn Res. 2015 Aug;9(8):PC01-5.




