Strategii terapeutice în cancerul laringian avansat. Partea I: Tratament radical
Therapeutic strategies for locally advanced laryngeal cancer. Part 1: Radical treatment
Abstract
According to the Union for International Cancer Control (UICC)/ American Joint Committee on Cancer (AJCC), staging system for the locally advanced laryngeal cancer generally denotes stage III or IV, stage III being represented by T3 or N1 tumors and the non-metastatic stage IV including N2-N3 or T4 tumors. The main therapeutic goals are local control and survival, but also the functional organ preservation (speech, swallowing and airway patency), if possible. To achieve these objectives, the management should be established by a multidisciplinary tumor board, based on the analysis of patient-specific factors (age, performance status, comorbidities, and psychosocial support), cancer topography and staging, but also the physician expertise and the availability of rehabilitation services. Regarding the larynx preservation, there are two major therapeutic strategies: total laryngectomy (associated with adjuvant radio- and chemotherapy) and larynx preservation strategy, which includes neoadjuvant chemotherapy followed by exclusive radiotherapy or concurrent radio-chemotherapy or radio-biotherapy. Total laryngectomy can be performed by open surgery or, in order to avoid a wide surgical field and reduce the local morbidity, by transoral techniques. After laryngectomy, the recurrence can be local, at the resection site, nodal, at cervical lymph nodes, or distal, the lung being the most common site of recurrence as a distant metastasis. To improve locoregional control and survival, adjuvant treatments are proposed, including radiotherapy, chemo- and biotherapy.Keywords
advanced cancerstaging(total) laryngectomyadjuvant treatmentbiotherapyRezumat
Potrivit Uniunii Internaţionale de Control al Cancerului/ Comitetului American de Stadializare a Cancerului, cancerul avansat de laringe este reprezentat, în general, de stadiile III şi IV. Stadiu III este reprezentat de tumorile T3 sau N1, iar stadiul IV include tumorile N2-N3 sau T4. Principalele obiective terapeutice sunt controlul local şi supravieţuirea pe termen lung, dar şi menţinerea/păstrarea funcţiilor laringelui (fonaţie, deglutiţie, respiraţie) atunci când este posibil. Pentru a putea atinge aceste obiective, strategia terapeutică ar trebui stabilită de o echipă multidisciplinară care să aibă în vedere factorii ce ţin de pacient (vârstă, comorbidităţi, sprijin psihosocial), localizarea şi stadializarea cancerului, experienţa medicilor şi accesul la servicii de reabilitare/recuperare. Există două metode de tratament al cancerului avansat de laringe: laringectomia totală (asociată cu radio-chimioterapie adjuvantă) şi prezervarea laringelui, care presupune chimioterapie neoadjuvantă, urmată de radioterapie exclusivă sau radio-chimioterapie concomitentă ori radio-bioterapie. Laringectomia totală poate fi realizată prin chirurgie deschisă (abord cervical) sau prin abord transoral, pentru a evita complicaţiile locale ce pot să apară ca urmare a unei plăgi extinse. Recurenţa post-laringectomie poate fi locală (la nivelul zonei de rezecţie), ganglionară (la nivelul reţelei ganglionare cervicale) sau distală (mai ales la nivel pulmonar). Pentru a îmbunătăţi controlul loco-regional şi supravieţuirea pe termen lung, sunt propuse tratamente adjuvante, precum radioterapie, chimioterapie sau bioterapie.Cuvinte Cheie
cancer avansatstadializarelaringectomie (totală)tratament adjuvantbioterapieLaryngeal cancer is one of the most common head and neck malignancies, representing 40% of all cases, and it is correlated mainly with smoking and alcohol, but also with low immunity, HPV infections, diet, and family history(1).
More than 90% of laryngeal cancers are squamous cell carcinomas, but other histological forms are described: adenocarcinomas, sarcomas, neuroendocrine carcinomas, or undifferentiated carcinomas(2).
Depending on the location of the lesion, the laryngeal cancer can be classified as:
Glottic carcinoma: it involves the true vocal folds (vocal fold and 1 cm inferiorly) in 50-60% of cases;
Supraglottic carcinoma: confined to the supraglottic area, laryngeal surface of epiglottitis, aryepiglottic fold, arytenoids, vestibule in 30-40% of cases;
Subglottic carcinoma: it extends or arises more than 10 mm below the free margin of the true vocal fold up to the inferior border of the cricoid cartilage;
Transglottic carcinoma: it originates from the center of ventricle where it spreads to the transglottic region (it crosses the ventricle from the supraglottic area to involve the true and false vocal folds or involves the glottis and extends subglottically more than 10 mm or both). There are fundamental differences between transglottic carcinoma and transglottic invasion of laryngeal carcinoma in the late stage of the lesion(2,3).


Laryngeal cancer staging
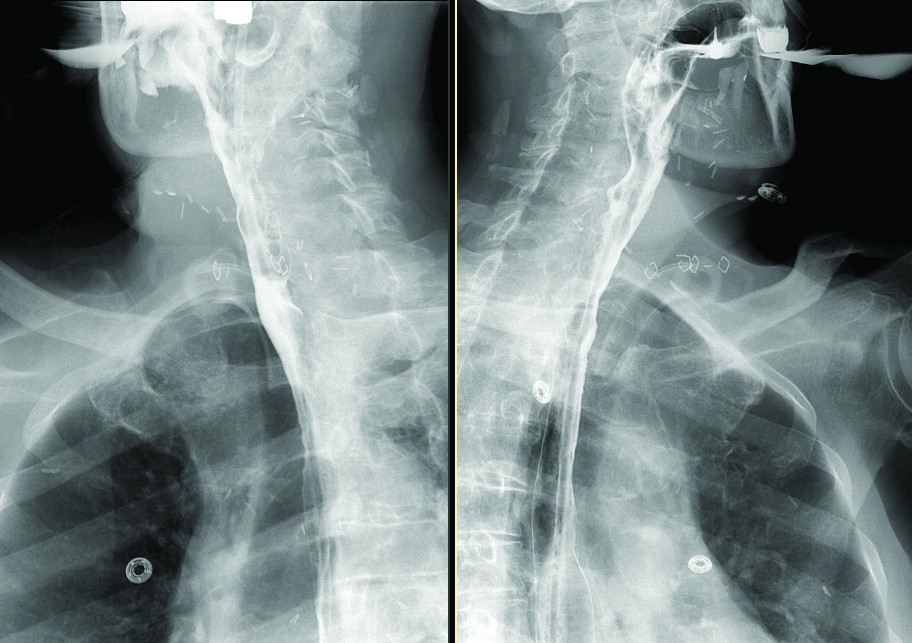
Initial evaluation of the primary tumor is based on a thorough history and combination of inspection, palpation, indirect mirror examination, or direct endoscopy. A fiber optic laryngoscopy and panendoscopy under anesthesia should generally be performed to take biopsies for a tissue diagnosis and to determine the clinical extent of the local disease(4). To evaluate the degree of local infiltration, the presence of regional lymph nodes and distant metastases or second primary tumors, CT, MRI and PET/CT are used. Computed Tomography can identify cervical lymph nodes metastasis and evaluate the bone cortex invasion and destruction. MRI allows a better discrimination of tumor from healthy tissues, perineural spread and cartilage invasion identification, particularly for non-ossified cartilages, but, unlike CT-scan, it does not show precise bony details(5).
The Positron Emission Tomography (PET) commonly uses 2-deoxy-2fluoro-(F-18)-D-glucose (FDG), an analogue of glucose that accumulates itself unspecifically in all glucose-dependent tissues, hence FDG uptake reflects metabolic activity of tumor lesions. The value of 18F-FDG uptake (Standardized Uptake Values, SUVs) depends mainly on tumor histology, proliferation and tissue hypoxia(6). PET-CT appears to be at least as sensitive and specific as CT and MRI in detecting primary head and neck tumors, but superior for detecting regional nodal metastases, as well as distant metastases and second primary tumors(7-9).Therefore, PET scan should be considered in patients at high risk for metastatic disease or with equivocal findings on CT or MRI scan, and also can be indicated for patients at increased risk of second malignancy (especially those with a smoking history) who will not have an operative panendoscopy (laryngoscopy, esophagoscopy, bronchoscopy)(10,11).
Staging depends on tumor location in one of the three anatomical regions: the glottis (true vocal cords, anterior and posterior commissures); the supraglottis (epiglottis, arytenoids and aryepiglottic folds, and false cords); and the subglottis. The term advanced laryngeal cancer generally denotes stage III or IV according to the Union for International Cancer Control (UICC)/American Joint Committee on Cancer (AJCC) staging system(3).
Stage III is represented by T3 or N1 tumors.
A T3 tumor is a tumor that remains limited to larynx but invades adjacent anatomical laryngeal regions, possibly causing vocal cord fixation. Independently of the initial tumor location (glottis, the supraglottis or subglottis), the fixation of the vocal cords always defines a T3 tumor, corresponding to deeply invasive lesions. The cervical lymph nodes are classified N1 if the metastasis is clinically detected in a single ipsilateral lymph node and the maximum diameter does not exceed 3 cm.
The non-metastatic stage IV includes N2-N3 or T4 tumors.
The metastatic lymph nodes are classified as N2 in case of lymph node 3 to 6 cm in its greatest dimension (N2a: single and ipsilateral, N2b: multiples and ipsilateral and N2c: bilateral or contralateral lymph nodes) and as N3 for more than 6 cm in the greatest dimension. Regarding the tumor classification, the T4a tumor invades through the thyroid cartilage and/or invades the tissues beyond the larynx (trachea, soft tissues of neck, including deep extrinsic muscle of the tongue, strap muscles, thyroid, or esophagus) and a T4 b tumor invades prevertebral space, encases carotid artery, or invades mediastinal structures.
Due to the importance of the larynx’s functions, advanced laryngeal cancer and its treatment are associated with significant morbidity and mortality, with important detrimental effect on the quality of life for the patient and increased financial costs for society.
Treatment strategy
The management of the advanced laryngeal cancer is complex and should be established by a multidisciplinary tumor board. The main goals are local control and survival, but also the functional organ preservation (speech, swallowing and airway patency), if possible. The main decision factors for the therapeutic strategy are: the patient-specific factors (age, performance status, comorbidity, psychosocial support), the cancer topography and staging, but also the physician expertise and the availability of rehabilitation services(12,13).
There are two major therapeutic strategies:
a) Total laryngectomy associated with adjuvant radio and chemotherapy.
b) Larynx preservation, including neoadjuvant chemotherapy followed by exclusive radiotherapy or concurrent radio-chemotherapy or radio-biotherapy.
A) Open Total Laryngectomy
Total laryngectomy, the surgical removal of the larynx with definitive tracheal stoma, remains the initial treatment choice for locally advanced laryngeal cancer.
Tumor surgery
Total laryngectomy is appropriate for patients that may not recover vocal or respiratory function if a larynx-preservation therapy is performed or for older and/or fragile patients, with poor compliance and functional status who do not fit for chemo-radiotherapy because of important risk for major toxicities.
The main surgical technique is the cranio-caudal laryngectomy. Retrograde laryngectomy is preferred for glottic or supraglottic tumors because it eliminates the risk of trans-tumoral laryngeal resection and ensures an adequate suprahyoid resection margin(14,15).
The total laryngectomy ensures protection against aspiration, easier swallowing and the possibility to speak with the help of a tracheoesophageal prosthesis. Its main disadvantage is the permanent tracheostomy. The laryngectomy is an absolute indication for:
1) tumors with cartilage destruction and anterior spread outside the larynx;
2) posterior commissure or bilateral arytenoid joint involvement;
3) circumferential submucosal disease;
4) subglottic extension with extensive invasion of the cricoid cartilage.
The neck dissection depends on cervical lymph nodes involvement and can be prophylactic, for early NO/N1 stages, or radical neck dissection for more advanced N2/N3 stage, and can be ipsilateral (in glottic carcinoma) or bilateral (supraglottic, medial wall of pyriform fossa, bilateral glottis carcinoma). According to the Committee for Head and Neck Surgery and Oncology of the American Academy of Otolaryngology - Head and Neck Surgery, the cervical lymph nodes dissections are classified in:
Radical neck dissection, the standard procedure, it means the removal of lymph node levels I-V, sternocleidomastoid muscle, spinal accessory nerve, and internal jugular vein.
Modified neck dissections
a) extended radical dissection: removal of additional lymph node or non lymphatic structures (retropharyngeal lymph nodes, hypoglossal nerve, portions of the prevertebral musculature, or the carotid artery);
b) modified radical dissection: preservation of non lymphatic structures - spinal accessory nerve, internal jugular vein, and/or sternomastoid muscle;
c) selective dissection: preservation of lymphatic structures - one or more lymph node groups normally removed in a radical neck dissection are preserved, in order to keep intact the anatomical and functional state, and minimize the risks of cervico-facial lymphedema(16).
Total laryngectomy complications
The complications of total laryngectomy are classified in immediate and long term complication. Acute complications are represented by bleeding, hematoma, seroma, wound dehiscence or infection, lymphatic fistulas, pharyngotracheal or pharyngocutaneous fistulas. Long term complications are mainly stomal stenosis, pharyngoesophageal stenosis, cervico-facial lymphedema (in radical neck dissection), hypothyroidism, voice and loss of smell(14).
B) Minimally invasive surgery techniques
To avoid a wide surgical field and reduce the local morbidity, two transoral techniques have been developed:
B.1) Transoral robotic surgery (TORS), introduced in clinical practice in 2007, adapted the open technique surgical steps to an endoscopic approach, permitting the direct intraoral view in order to achieve a maximal mucosa - sparing resection with minimal pharyngotomy defect and limiting the lateral exposure of the cervical vessels(17).
As a rule, the application of transoral surgery should never compromise the ability to completely remove the tumor, the issues of concern including prior tracheotomy, severe soft tissue fibrosis and adequate evaluation of the cervical lymph nodes(18).
B.2) Transoral Endoscopic Ultrasonic Total Laryngectomy (TOUSS-TL) is a transoral, endoscopic but non-robotic approach possible only for patients with laryngeal cancer without indication for neck dissection and no invasion through the thyroid cartilage or soft tissues of the neck (T4a) or major extralaryngeal invasion (T4b)(19).
Recurrence after total laryngectomy
The recurrence can be local, to the resection site, nodal, to cervical lymph nodes, or distal, the lung being the most common site of recurrence as a distant metastasis. The median time of recurrence following laryngectomy is 13.3 months, more rapid for nodal recurrence (median: 9.4 months) than for local recurrence (median: 12 months). Lung metastases had the longest time to recurrence (median: 20 months)(20). The main three factors associated with an increased risk of locoregional recurrence after surgery are tumor stage (T3-T4 tumors), lymph nodes stages (two or more positive lymph nodes and/or extracapsular extension) and surgical margins (positive or close resection margins)(21,22). Preoperative tracheostomy, correlated with advanced tumor stage, is a significant risk factor for local recurrence. With regard to pattern of local recurrence, stomal recurrence is correlated with preoperative tracheostomy and pathological nodal status, whereas positive margins are significant risk factors for pharyngeal recurrence(23).
Adjuvant treatments
The aim of adjuvant treatment is to improve locoregional control and survival by eradicating microscopic remains of cancerous cells.
A) Adjuvant radiotherapy
A retrospective analysis on 8795 patients with lymph node-positive head and neck carcinoma (Surveillance, Epidemiology, and End Results database) treated either with surgery alone or surgery and radiotherapy between 1988 and 2001 shows that adjuvant radiotherapy improves the 5-year overall survival (from 33.4% to 43.2%; p<0.001) and cancer-specific survival (from 42.1% to 50.9%, p<.001). Adjuvant radiotherapy is a significant predictor of improved survival, resulting in an approximately 10% absolute increase in 5-year cancer-specific survival and overall survival for lymph node-positive patients compared with surgery alone(24).
B) Adjuvant chemo-radiotherapy
B.1) Sequential adjuvant chemo-radiotherapy
The Intergrup Study 0034 randomizes 442 patients with completely resected head and neck tumors between chemotherapy followed by postoperative radiotherapy or postoperative radiotherapy alone. The study included 127 patients with laryngeal cancer, 61 in the radiotherapy arm and 66 in the combination arm. The chemotherapy consisted on three cycles of Cis-platinum 100 mg/m2 on day 1 and infusion 5-FU 1 g/m2 over 24 hours on days l-5. This chemotherapy regimen was administered every 21 days. The radiation therapy was the same on each arm, 50-54 Gy delivered to “low risk” volumes and 60 Gy to “high-risk” volumes (the surgical margin was 5 mm or less, in presence of extra capsular nodal extension, and/or carcinoma in situ at the surgical margins). The association of chemotherapy to adjuvant radiotherapy produces a significant benefit in term of lymph node failure (decrease from 10% to 5%) and distant metastases (from 23% to 15%), but without significant benefit for the 4-year overall survival (44% on the RT arm versus 48% on the CT/RT arm) or disease-free survival (38% on the RT arm compared to 46% on the CT/RT arm). In terms of toxicity, the chemotherapy was well tolerated and did not affect the ability to deliver the subsequent radiotherapy(25).
B.2) Concomitant adjuvant chemo-radiotherapy
1) Cisplatin-based chemo-radiotherapy. Two prospective phase III clinical randomized trials have demonstrated that adjuvant cisplatin-based chemotherapy associated with radiotherapy improves local control compared with the same radiotherapy used alone in patients with poor prognosis of head and neck carcinomas, including advanced laryngeal cancer
European Organisation for Research and Treatment of Cancer (EORTC) 22931 study
From February 1994 to October 2000, 334 patients with high-risk head and neck cancers (oral cavity, oropharynx, larynx, or hypopharynx) treated by surgery were randomized between radiotherapy alone (38 laryngeal cancer patients included) or radiotherapy combined with concomitant cisplatin chemotherapy (37 laryngeal cancer patients included). All patients received the same postoperative radiotherapy, 54 Gy in 27 fractions to the primary site and all draining lymph nodes at risk and 66 Gy in 33 fractions to the regions that were at high risk for malignant dissemination or had inadequate resection margins. For the experimental arm, the chemotherapy consisted of 100 mg/m2 of Cisplatin on days 1, 22, and 43 of the course of radiotherapy. The results at 5 years show that concomitant chemoradiation significantly improves the progression-free survival from 36% to 47% and the overall survival from 40% to 53%(26).
Radiation Therapy Oncology Group (RTOG) 95-01 study
Between 1995 and 2000, 459 patients with high-risk head and neck cancers (oral cavity, oropharynx, larynx, or hypopharynx), totally resected, were randomly assigned to receive radiotherapy alone or in combination with concurrent Cisplatin (100 mg/m2) on days 1, 22, and 43. There were 12 patients with laryngeal cancer in the radiotherapy arm and 13 in combination therapeutic arm. The radiotherapy began as soon after surgery as adequate healing had occurred, 4-6 weeks after the surgical procedure, and delivered 60 Gy in 30 fractions with or without a boost of 6 Gy in 3 fractions to high-risk sites. The study proves that combined treatments significantly improve the locoregional control from 72% to 82% at 2 years, but that overall survival does not differ significantly(27).
Regarding toxicity, it was found that Cisplatin-based chemotherapy doubles the incidence of grade 3 or greater acute adverse effects (from 21-34% to 41-77%), in the RTOG study - four patients who received combined therapy died as a direct result of the treatment. A meta-analysis of the RTOG and EORTC trials identifies the patients who benefited significantly from the addition of chemotherapy to the radiation therapy, namely the patients with positive resection margins and/or nodal extracapsular extension(28).
2) Mitomycine C-based chemotherapy. There are two prospective phase III clinical randomized trials that used Mitomicyne C-based chemotherapy to compare the potential benefit in adjuvant setting in combination with external radiotherapy.
In a Slovenian prospective randomized clinical trial, 114 patients with stage III or IV squamous cell head-and-neck carcinoma were randomized to receive postoperative radiotherapy alone (two-dimensional, 2 Gy daily dose, 5 times weekly up to a total dose 56-70 Gy) or in combination with simultaneous Mitomycin C (15 mg/m2) and Bleomycin (5 mg twice a week) during the radiation therapy. There were 12 laryngeal cancer patients included in the radiotherapy arm and 14 in the combination arm. The radiochemotherapy group had better locoregional control (86% versus 69%, p=0.037), disease-free survival (76% vs. 60%, p=0.099) and overall survival (74% vs. 64%, p=0.036) compared with the radiotherapy alone. The association of chemotherapy increased the acute toxic effects, especially mucositis (grade 4 in 17 patients compared with only 1 for radiotherapy alone), but also dermatitis and infection, that were more frequent for these patients(29).
Yale Mitomycin Randomized Trials analyzed 195 eligible patients randomized to receive radiation therapy with or without Mitomycin (trial 1) or Mitomycin/Dicumarol (trial 2). There were 13 laryngeal cancer patients allocated in the radiotherapy arm, and 14 in the combination arm. The radiotherapy, identical for the two arms, delivered a total dose of 60-66 Gy with 1.8-2 Gy daily fraction, 5 days a week. The Mitomycin C was administered intravenously at a dose of 15 mg/m2 following radiation on the fifth day of the radiotherapy course. In the second trial, patients receiving Mitomycin also received a total of 500 mg of Dicoumarol (an anticoagulant similar to warfarin) administered orally, with 300 mg given the day before Mitomycin C and 200 mg given on the day of Mitomycin C. The trial conclusion is that concomitant administration of Mitomycin C with radiation therapy significantly improves the 5-year disease-free survival from 44% to 67% (p<.03), but without a 5-year overall survival benefit (56% vs. 41%). Hematologic toxicities were more frequently noted in the drug-treated arms, but were acceptable with no drug-related treatment deaths(30). Thus, due to its toxicity, Mitomicyn C cannot be routinely recommended in association with radiotherapy for head and neck cancers.
3) Cetuximab-based systemic treatment
Cetuximab, a monoclonal antibody targeting the epidermal growth factor receptor (EGFR), is an effective anti-neoplastic molecule that also plays a role in increasing radiosensitization(31,32). Cetuximab initial dose is 400 mg/m2 administrated intravenously (i.v.) over 120 minutes followed by cetuximab, 250 mg/m2 intravenously (i.v.) over 60 minutes on a weekly schedule(33).
Cetuximab as adjuvant for patients with intermediate-risk pathologic features
In order to evaluate whether the addition of cetuximab to radiation therapy improves overall survival in postoperative patients with intermediate risk pathologic features, RTOG opened a randomized phase III trial (RTOG 0920) that compared 60 Gy/30 fractions with the same radiotherapy associated with concomitant and adjuvant Cetuximab. The intermediate risk factors are perineural invasion, lymphovascular invasion, single lymph node >3 cm or ≥2 lymph nodes (all <6 cm) (but without extracapsular extension), close surgical margin(s) or pT3/T4a primary tumors. The results are not available yet(34).
Cetuximab as adjuvant for patients with high-risk pathologic features
The addition of concurrent chemo-radiotherapy with Cetuximab in the postoperative treatment of patients with squamous cell carcinoma of the head and neck with high-risk pathologic features was analyzed in RTOG 0234 randomized phase II clinical trial. The high-risk factors are extracapsular nodal extension, positive surgical margins and two or more metastatic lymph nodes. In this study, 203 analyzable patients (including 21 patients with advanced laryngeal cancer) were randomly assigned to 60 Gy radiation with Cetuximab once per week plus either Cisplatin 30 mg/m2 or Docetaxel 15 mg/m2 once per week. The Docetaxel regimen shows favorable outcome with improved 2-year disease-free survival (DFS 66% against 57% for Cisplatin arm) and overall survival (OS 79% against 69% for Cisplatin arm), with decreased hematologic toxicity (grade 3 to 4 myelosuppression in 14% of patients versus 28% for cisplatin arm). In conclusion, the delivery of postoperative chemo-radiotherapy (using Cisplatin or Docetaxel once per week plus 60 Gy radiation) with concurrent once per week Cetuximab is feasible and tolerated with predictable toxicity(35).
The interval between surgery and adjuvant radiotherapy
The time between surgery and adjuvant radiotherapy (normally, 4-6 weeks), necessary for postoperative wound healing, may allow the proliferation of residual tumor cells because of the growth factor increased concentrations in surgical bed(36). The postoperative recovery interval is also an opportunity for tumor cells to become radiation refractory, because resistance is proportional to the number of surviving cells(37).
To evaluate the practical possibility of an early postoperative chemotherapy, 70 resected patients with locally-advanced stages III to IV head and neck squamous carcinoma (positive surgical margins and/or extracapsular nodal extension and/ or multiple positive nodes) are treated in the RTOG 0024 trial by 3 early chemotherapy cycles followed by concurrent chemoradiotherapy. Early-adjuvant chemotherapy consists of Paclitaxel 80 mg/m2 for three weekly cycles starting from the first or second week after surgery (i.e., postoperative day 7 through 14). Concurrent chemotherapy was Paclitaxel 30 mg/m2 i.v. followed immediately by Cisplatin 20 mg/m2 i.v. once weekly for three cycles (i.e., cycles 4 through 6) given in the last 3 weeks of radiotherapy (60 Gy in 30 fractions). The fourth grade non hematologic toxicity produced by the early-adjuvant chemotherapy is represented by mucosal and cutaneous fistulae (3 patients), mucositis (2 patients), and superficial skin dehiscence (3 patients). After adjustment for the prognostic factors, the regimen in RTOG 0024 may be superior to either adjuvant radiotherapy or to radiotherapy with concurrent chemotherapy, with an estimated reduction in risk for disease-free survival and death of approximately 30% to 40%. The locoregional control benefit is greater, with estimated reductions in risk of 41% versus chemo-radiotherapy and 60% versus radiotherapy alone(38).
Conclusions and recommendations regardind post laryngectomy adjuvant treaments
For each patient, a multidisciplinary treatment schedule should be established. The patient’s nutritional status must be corrected and maintained, and dental rehabilitation is indicated before radiotherapy(39).
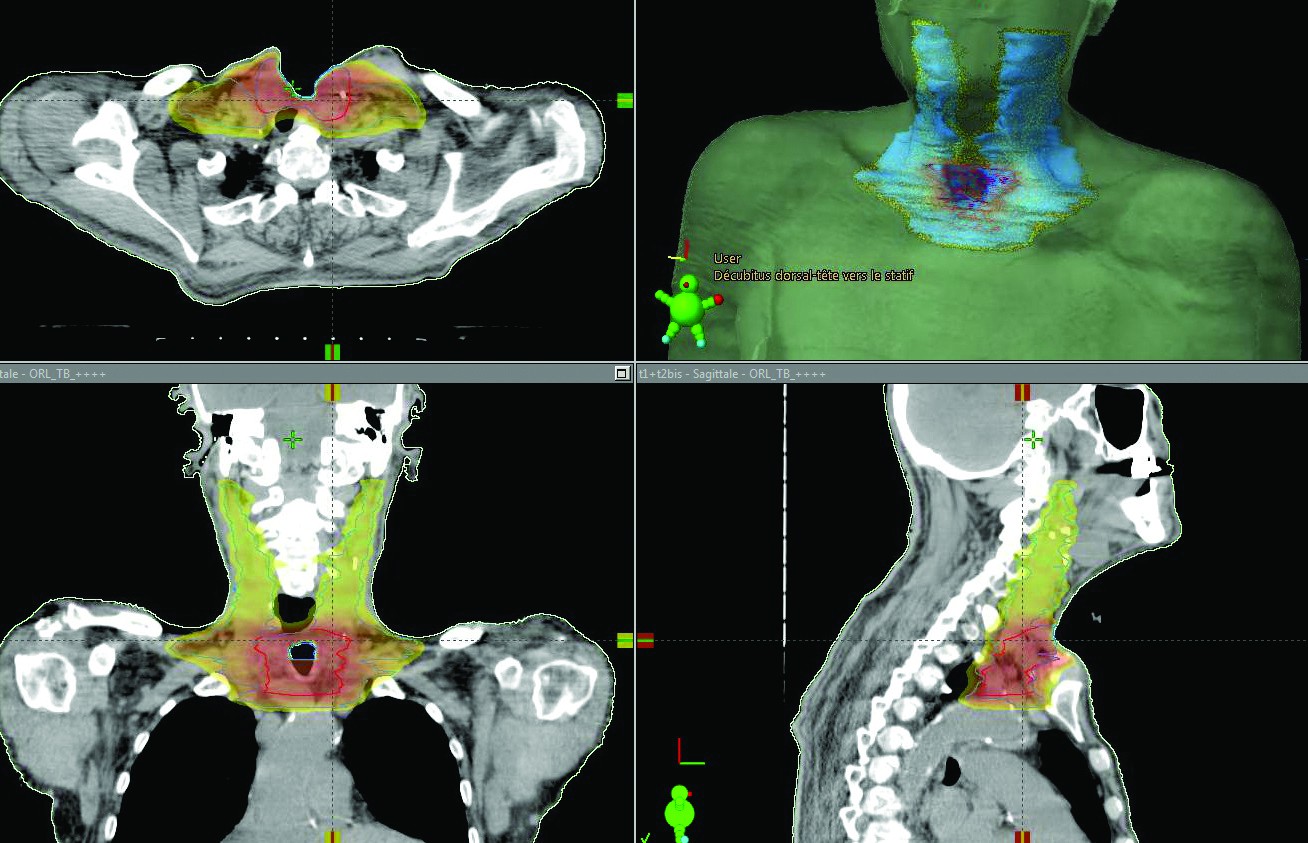
The 2016 guideline of National Comprehensive Cancer Network (NCCN) recommends adjuvant concurrent chemoradiation therapy for significant nodal disease (multiple positive neck nodes-N2-N3, extracapsular extension) and/or large and infiltrative pT4 tumors. Postoperative exclusive radiotherapy is indicated if any two of the following factors are present: close surgery margins (<5 mm), 1 positive lymph node, multicentric primary or peri-neural invasion. The adjuvant radiotherapy is preferable to begin before 6 weeks after surgery and to deliver 60-66 Gy in 2 Gy/fraction to nodal and laryngeal area that are at risk for local/regional recurrence(40).
The recommended adjuvant chemo-radiotherapy regimen uses Cisplatin 100 mg/m2 administered every 21 days for three cycles (days 1, 22, and 43) concurrently with standard doses of conventionally fractionated radiotherapy(41).
Bibliografie
1. Karatzanis AD, Psychogios G, Waldfahrer F, Kapsreiter M, Zenk J, Velegrakis GA, Iro H: Management of locally advanced laryngeal cancer. J Otolaryngol Head Neck Surg. 2014 Jan 28; 43:4.
2. Nikolaos S Mastronikolis, Theodoros A Papadas, Panos D Goumas, Irene-Eva Triantaphyllidou, Dimitrios A Theocharis, Nikoletta Papageorgakopoulou, Demitrios H Vynios: Head and Neck: Laryngeal tumors: an overview, Atlas Genet Cytogenet Oncol Haematol. 2009; 13(11):888-893.
3. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trott: Larynx. In, AJCC Cancer Staging Manual 7th ed. New York, NY: Springer, 2010, pp 57-62.
4. Tandon S, Shahab R, Benton JI, et al. Fine-needle aspiration cytology in a regional head and neck cancer center: comparison with a systematic review and meta-analysis. Head Neck 2008; 30:1246.
5. Sakata K, Hareyama M, Tamakawa M, Oouchi A, Sido M, Nagakura H, Akiba H, Koito K, Himi T, Asakura K: Overview of the diagnosis and staging of head and neck cancer, Int J Radiat Oncol Biol Phys. 1999; 43(2):273.
6. Kelloff GJ, Hoffman JM, Johnson B, Scher HI, Siegel BA, Cheng EY, Cheson BD, O’shaughnessy J, Guyton KZ, Mankoff DA, Shankar L, Larson SM, Sigman CC, Schilsky RL, Sullivan DC: Progress and promise of FDG-PET imaging for cancer patient management and oncologic drug development, Clin Cancer Res. 11: 2785–2808.
7. Rudmik L, Lau HY, Matthews TW, Bosch JD, Kloiber R, Molnar CP, Dort JC : Clinical utility of PET/CT in the evaluation of head and neck squamous cell carcinoma with an unknown primary: a prospective clinical trial. Head Neck. 2011; 33(7):935.
8. Johnson JT, Branstetter BF 4th: PET/CT in head and neck oncology: State-of-the-art 2013, Laryngoscope. 2014 Apr; 124(4):913-5. Epub 2014 Feb 10.
9. Escott EJ: Role of positron emission tomography/computed tomography (PET/CT) in head and neck cancer. Radiol Clin North Am. 2013 Sep; 51(5):881-93. Epub 2013 Jul 12.
10. Ng SH, Yen TC, Chang JT, et al. Prospective study of [18F]fluorodeoxyglucose positron emission tomography and computed tomography and magnetic resonance imaging in oral cavity squamous cell carcinoma with palpably negative neck. J Clin Oncol 2006; 24:4371.
11. Myers LL, Wax MK. Positron emission tomography in the evaluation of the negative neck in patients with oral cavity cancer. J Otolaryngol 1998; 27:342.
12. Kelly SL, Jackson JE, Hickey BE, et al. Multidisciplinary clinic care improves adherence to best practice in head and neck cancer. Am J Otolaryngol 2013; 34:57.
13. Wheless SA, McKinney KA, Zanation AM. A prospective study of the clinical impact of a multidisciplinary head and neck tumor board. Otolaryngol Head Neck Surg 2010; 143:650.
14. Ceachir O, Hainarosie R, Zainea Viorel: Total Laryngectomy – Past, Present, Future, Maedica (Bucharest). 2014 Jun; 9(2): 210–216.
15. Johan Fagan: Total laryngectomy, The open acces atlas of otolaryngology, head and neck operative surgery guides, University of Cape Town, Division of Otolaryngology http://www.entdev.uct.ac.za/guides/open-access-atlas-of-otolaryngology-head-neck-operative-surgery/
16. Robbins KT, Indications for selective neck dissection: when, how, and why. Oncology (Williston Park). 2000 Oct; 14(10):1455-64; discussion 1467-9.
17. Mendelsohn AH, Remacle M: Transoral robotic surgery for laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg. 2015 Apr; 23(2):148-52.
18. Smith RV. Transoral robotic surgery for larynx cancer. Otolaryngol Clin North Am. 2014 Jun; 47(3):379-95.
19. Fernández-Fernández MM, Montes-Jovellar L, Parente Arias PL, Ortega Del Alamo P: TransOral endoscopic UltraSonic Surgery (TOUSS): a preliminary report of a novel robotless alternative to TORS. Eur Arch Otorhinolaryngol. 2015 Dec; 272(12):3785-91.
20. J. Levi Chazen, Christine M. Glastonbury: Total laryngectomy for squamous cell carcinoma: recognizing disease patterns to aid detection of tumor recurrence, Clinical Imaging, Volume 38, Issue 5, September - October 2014, Pages 659-665.
21. Yuen AP, Wei WI, Ho WK, Hui Y: Risk factors of tracheostomal recurrence after laryngectomy for laryngeal carcinoma, Am J Surg. 1996 Sep; 172(3):263-6.
22. Zhao H, Ren J, Zhuo X, Ye H, Zou J, Liu S: Stomal recurrence after total laryngectomy: a clinicopathological multivariate analysis. Am J Clin Oncol. 2009 Apr; 32(2):154-7.
23. Naveed Basheeth, Gerard O’Leary, Habib Khan, Patrick Sheahan: Oncologic outcomes of total laryngectomy: Impact of margins and preoperative tracheostomy, HEAD & NECK Volume 37, Issue 6, June 2015, Pages: 862–869.
24. Lavaf A, Genden EM, Cesaretti JA, Packer S, Kao J: Adjuvant radiotherapy improves overall survival for patients with lymph node-positive head and neck squamous cell carcinoma, Cancer. 2008 Feb 1; 112(3):535-43.
25. Laramore GE, Scott CB, al-Sarraf M, Haselow RE, Ervin TJ, Wheeler R, Jacobs JR, Schuller DE, Gahbauer RA, Schwade JG: Adjuvant chemotherapy for resectable squamous cell carcinomas of the head and neck: report on Intergroup Study 0034, Int J Radiat Oncol Biol Phys. 1992; 23(4):705-13.
26. Bernier J, Domenge C, Ozsahin M, Matuszewska K, Lefèbvre JL, Greiner RH, Giralt J, Maingon P, Rolland F, Bolla M, Cognetti F,Bourhis J, Kirkpatrick A, van Glabbeke M; European Organization for Research and Treatment of Cancer Trial 22931: Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004 May 6;350(19):1945-52.2
27. Cooper JS, Pajak TF, Forastiere AA, Jacobs J, Campbell BH, Saxman SB, Kish JA, Kim HE, Cmelak AJ, Rotman M, Machtay M,Ensley JF, Chao KS, Schultz CJ, Lee N, Fu KK; Radiation Therapy Oncology Group 9501/ Intergroup: Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004 May 6; 350(19):1937-44.
28. Bernier J, Cooper JS, Pajak TF, van Glabbeke M, Bourhis J, Forastiere A, Ozsahin EM, Jacobs JR, Jassem J, Ang KK, Lefèbvre JL: Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501), Head Neck. 2005 Oct; 27(10):843-50.
29. Smid L, Budihna M, Zakotnik B, Soba E, Strojan P, Fajdiga I, Zargi M, Oblak I, Dremelj M, LeSnicar H: Postoperative concomitant irradiation and chemotherapy with mitomycin C and bleomycin for advanced head-and-neck carcinoma, Int J Radiat Oncol Biol Phys. 2003 Jul 15; 56(4):1055-62.
30. Haffty BG, Son YH, Sasaki CT, Papac R, Fischer D, Rockwell S, Sartorelli A, Fischer JJ: Mitomycin C as an adjunct to postoperative radiation therapy in squamous cell carcinoma of the head and neck: results from two randomized clinical trials, Int J Radiat Oncol Biol Phys. 1993 Sep 30; 27(2):241-50.
31. Harding J, Burtness B: Cetuximab: an epidermal growth factor receptor chemeric human-murine monoclonal antibody. Drugs Today (Barc). 2005 Feb; 41(2):107-27.
32. Azria D, Larbouret C, Robert B, Culine S, Ychou M, Verrelle P, Dubois JB, Pèlegrin A: Radiotherapy and inhibitors of epidermal growth factor receptor: preclinical findings and preliminary clinical trials, Bull Cancer. 2003 Nov; 90 Spec No:S202-12.
33. Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB et al. : Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2009:354:567-78
34. National Cancer Institute: Radiation Therapy with or without Cetuximab in Treating Patients Who Have Undergone Surgery for Locally Advanced Head and Neck Cancer TRIAL; http://www.cancer.gov/about-cancer/treatment/clinical-trials/search/view?cdrid=651536
35. Harari PM, Harris J, Kies MS, Myers JN, Jordan RC, Gillison ML, Foote RL, Machtay M, Rotman M, Khuntia D, Straube W, Zhang Q, Ang K: Postoperative chemoradiotherapy and cetuximab for high-risk squamous cell carcinoma of the head and neck: Radiation Therapy Oncology Group RTOG-0234, J Clin Oncol. 2014 Aug 10; 32(23):2486-95.
36. Licitra LF, Perrone F, Tamborini E, et al: Effect of antityrosyne kinase agents on in vitro tumor cell proliferation induced by wound drainage fluids (WDFs) of head and neck cancer (HNSCC) patients. J Clin Oncol. 2008; 26(suppl):335s. abstr 6077).
37. DeVita VT Jr: The James Ewing lecture. The relationship between tumor mass and resistance to chemotherapy. Implications for surgical adjuvant treatment of cancer. Cancer. 1983 Apr 1; 51(7):1209-20.)
38. Rosenthal DI, Harris J, Forastiere AA, et al. Early Postoperative Paclitaxel Followed by Concurrent Paclitaxel and Cisplatin With Radiation Therapy for Patients With Resected High-Risk Head and Neck Squamous Cell Carcinoma: Report of the Phase II Trial RTOG 0024. Journal of Clinical Oncology. 2009; 27(28):4727-4732. )
39. Grégoire V1, Lefebvre JL, Licitra L, Felip E; EHNS-ESMO-ESTRO Guidelines Working Group.Squamous cell carcinoma of the head and neck: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2010; 21 (Suppl 5): vi184-vi186.)
40. NCCN Clinical Practice Guidelines in Onclology, Head and Neck cancers, vol I 2016 (https://www.nccn.org/professionals/physician_gls/f_guidelines_nojava.asp#site)
41. Bachaud JM, Cohen-Jonathan E, Alzieu C, et al. Combined postoperative radiotherapy and weekly cisplatin infusion for locally advanced head and neck carcinoma: final report of a randomized trial. Int J Radiat Oncol Biol Phys. 1996 Dec 1. 36(5):999-1004)


