Helicobacter pylori infection is aquired in childhood, affects more than half of the world population and is associated with chronic gastritis. The majority of the infected children are asymptomatic. The most frequently used tests for the detection of Helicobacter pylori are ¹³C urea breath test and stool antigen test. Objective. In this study, we evaluated the accuracy and the utility of the ¹³C urea breath test and Helicobacter pylori stool antigen test in young children. We performed a prospective observational study of 52 symptomatic children, mostly with uninvestigated dyspepsia suggestive for an organic disease. The ¹³C urea breath test was used as gold standard method for the diagnosis of Helicobacter pylori infection. Forty-two of the 52 studied children had a positive ¹³C urea breath test, respectively 21 of 42 Helicobacter pylori infected children presented a positive rapid stool antigen test for Helicobacter pylori. Our study did not reveal a strong agreement between Helicobacter pylori rapid stool antigen test and ¹³C urea breath test. The management of Helicobacter pylori infection in children remains a problem in clinical practice, therefore testing for Helicobacter pylori infection has become a very important part of the diagnostic process. Another multicenter study from our country is recommended.
Diagnostic accuracy of noninvasive tests for pediatric Helicobacter pylori infection
Acurateţea testelor neinvazive la copii pentru precizia diagnosticului de infecţie cu Helicobacter pylori
First published: 30 iunie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Pedi.70.2.2023.8306
Abstract
Rezumat
Dobândirea infecţiei cu Helicobacter pylori se produce precoce în copilărie, infecţia fiind regăsită la peste jumătate din populaţia lumii. Majoritatea pacienţilor pediatrici infectaţi sunt asimptomatici. Diagnosticul infecţiei cu Helicobacter pylori la copil poate fi realizat prin tehnici neinvazive (testul respirator cu uree marcată cu C¹³, precum şi determinarea antigenelor fecale). Studiul evaluează acurateţea şi utilitatea metodelor neinvazive în diagnosticul infecţiei cu Helicobacter pylori la copil. Autorii au realizat un studiu observaţional, prospectiv, care a inclus 52 de copii cu simptomatologie digestivă sugestivă pentru o cauză organică. În studiul nostru, testul respirator cu uree marcată cu C¹³ a fost utilizat ca metodă gold standard de diagnostic al infecţiei cu Helicobacter pylori. 42 din cei 52 de copii evaluaţi au avut testul respirator cu uree C¹³ pozitiv, în timp ce 21 din cei 42 de copii infectaţi cu Helicobacter pylori au prezentat antigen fecal pozitiv. Studiul nostru nu a evidenţiat o concordanţă puternică între cele două teste, respectiv între antigenul fecal pentru Helicobacter pylori şi testul respirator cu uree C¹³. Managementul infecţiei cu Helicobacter pylori la copii rămâne o problemă importantă în practica clinică pediatrică, de aceea sunt necesare studii multicentrice în ţara noastră.
Introduction
Helicobacter pylori (H. pylori) infection is one of the most common gastrointestinal infections, afflicting more than half of the human population worldwide.
H. pylori infection is acquired during childhood and causes chronic gastritis which can progress to peptic ulcer, gastric adenocarcinoma and gastric mucosa-associated lymphoid tissue lymphoma (MALT)(1).
The majority of H. pylori infected children are asymptomatic. The clinical manifestations are nonspecific, and the digestive manifestations include: persistent chronic abdominal pain without any alarm sign or symptoms, epigastric pain, nausea, gastroesophageal reflux with or without heartburn, halitosis, vomiting or gastrointestinal bleeding. H. pylori may play a role in some extraintestinal disease, such as unexplained iron deficiency anemia, chronic immune thrombocytopenic purpura, Henoch-Schönlein purpura, inflammatory bowel disease, asthma, allergic diseases, growth retardation and impaired cognitive function(2).
An accurate diagnosis of H. pylori infection in children is essential and is required before treatment. Several diagnostic invasive and noninvasive methods are used for the detection of H. pylori infection in children.
The recent guidelines of the European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) do not recommend the diagnostic testing for H. pylori infection in children with functional abdominal pain disorders. The children with periodontal disease, otitis media, upper tract respiratory infections, food allergy, short stature or children with family history for gastric cancer should be tested for H. pylori infection(3).
According to the ESPGHAN and NASPGHAN guidelines, revised in 2016, H. pylori diagnostic require at least two invasive tests: a positive culture or a histopathologic finding of H. pylori gastritis, accompanied by rapid urease test.
Noninvasive assessment methods, such as urea breath test (UBT) and H. pylori fecal antigen test, are reserved to determine the active infection before and after therapy. Because the antibodies of H. pylori persist for a long time after eradication, the antibody-based tests do not allow to differentiate between current and past infection(4).
The ¹³C urea breath test (¹³C UBT) is an easy, safe and most accurate noninvasive test for the detection of H. pylori infection, with a high sensitivity and specificity (from 90% to 100%)(5). The test specificity of UBT decreases in children under 6 years old, because it requires active cooperation of the patients. H. pylori is a Gram-negative bacterium that produce urease, an enzyme that discompose urea in the stomach and release carbonic acid and ammonia. UBT test uses the urease activity to detect the H. pylori infection.
According to the American College of Gastroenterology guidelines, UBT can be used for the diagnosis of H. pylori infection in children(6).
H. pylori fecal antigen test detects the antigen of the bacterium and is able to diagnose an ongoing infection. It is a noninvasive quick test, with no age dependency, which has a good sensitivity and specificity.
Objective
The aim of this study was to assess the accuracy and the utility of the ¹³C UBT and H. pylori fecal antigen test. Another objective of our study was to investigate if the two noninvasive tests have a good concordance in young children.
The exclusion criteria were: the administration of antibiotics within 4-6 weeks or the administration of proton pump inhibitors within two weeks before testing.
Materials and method
The patients were fasted for at least 4 hours and then ¹³C labeled urea dissolved in water was given without taking any test meal. To reduce the effect of urease producing oral bacteria, patients rinsed their mouth with water immediately after the ingestion of ¹³C urea. Breath samples were collected before and after the ingestion of the ¹³C urea. The H. pylori fecal antigen test was performed using the H. pylori antigen rapid test.
The statistical software SPSS version 16.0 and EpiInfo 7.2.5.0. were used for data analysis. The sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) were calculated.
We conducted a prospective observational study, from July to September 2020, that included 52 symptomatic children (33 girls, respectively 63.46%; sex ratio 1.73; mean age 11.36 years old; range age 6-18 years old). The patients were admitted in our hospital for various symptoms, mostly with uninvestigated dyspepsia suggestive for an organic disease.
The clinical manifestations, the nutritional status and socioeconomic data were recorded.
Discussion
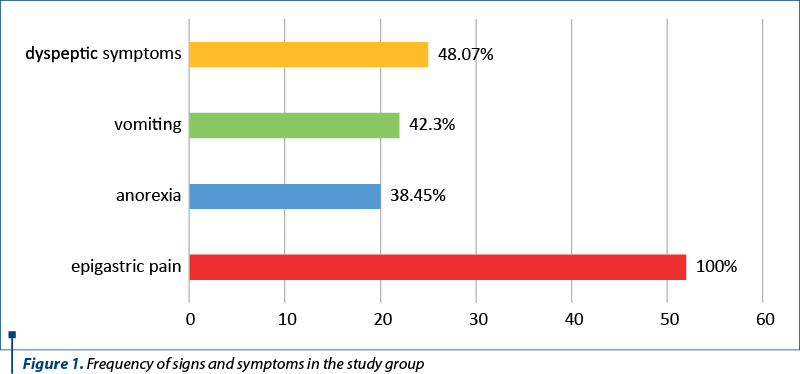
Chronic abdominal pain with epigastric localization was the leading admission symptom in all investigated children (52 of 52 cases; 100%).
Our study group associated also other clinical manifestations, such as anorexia (20 of 52 cases; 38.45%), regurgitation/vomiting (22 of 52 cases; 42.3%), dyspeptic symptoms (25 of 52 cases; 48.07%).
Twenty-two of 52 children (42.30%) had more than one sign and symptoms, and the rest (30 of 52 cases; 57.69%) complained of just one symptom, respectively epigastric pain.
The frequency of signs and symptoms in the study group are presented in Figure 1.
The assessment of the patient’s nutritional status revealed that a significant proportion of patients had a good nutritional status (35 of 52 cases; 67.30%), respectively 17 of 52 cases were underweight (32.69%).
Out of the 52 studied children, 42 (80.77%) had a positive ¹³C UBT.
In our study group, according with the ESPGHAN and NASPGHAN recent data, the ¹³C UBT was considered as the gold standard method to define H. pylori infection (sensitivity: 80.76%).
The H. pylori rapid fecal antigen test was positive in 21 (50%) of 42 H. pylori infected children and negative in 21 cases (50%).
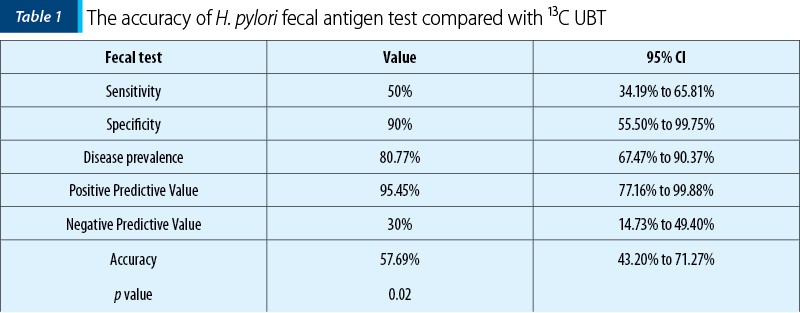
In our study, the sensitivity and specificity of rapid fecal antigen test in the detection of H. pylori infection compared with ¹³C UBT were 50% (CI 95%; 34.19% to 65.81%) and 90% (CI 95%; 55.50% to 99.75% respectively. Table 1 shows the accuracy of H. pylori fecal antigen test compared with ¹³C UBT.
Our study did not reveal a strong agreement between H. pylori rapid fecal antigen test and ¹³C UBT (k coefficient 0.28 fair level of agreement).
Conclusions
The management of Helicobacter pylori in children is a long-standing problem. Therefore, testing for H. pylori infection has become a very important part of the diagnostic process for gastroduodenal disease. The fecal antigen test and the urea breath test are reliable and noninvasive approaches for detecting H. pylori infection, and they have a potential use as screening tests in the pediatric population.
The monoclonal fecal test has a better diagnostic accuracy compared with the rapid fecal antigen test, although more studies are necessary to definitively recommend its use for the confirmation of H. pylori eradication success. The false-negative test results of rapid fecal antigen test have been due to low colonization of bacteria in the stomach, leading to a low concentration of antigens of H. pylori in the feces and to the inability to react in the test(7). It is important to note that there are studies demonstrating a high accuracy of the fecal antigen test, especially of the monoclonal fecal antigen test.
In our study, the ¹³C UBT had a sensitivity rate of 80.76%, which can be compared to results from other studies. A recent meta-analysis of Imrie et al. showed a sensitivity of 96.16% and a specificity of 97.7% in children above 6 years old(5).
False-positive and false-negative results of UBT are unlikely and may be noted in patients who are not compliant(8). Another possibility is that the children used proton pump inhibitors or antibiotics before the test.
A more frequent loss of infection might also explain a higher rate of disagreement between the two noninvasive tests, because the elimination of H. pylori antigens in the stool may take longer.
UBT has similar sensitivity and specificity to gastroscopy and biopsies for diagnosing H. pylori infection, but it is not able to evaluate the potential complications, such as gastroduodenal ulcers/erosions or gastric intestinal metaplasia.
According to ESPGHAN and NASPGHAN guidelines, the Maastricht 2-2000 guidelines recommended the UBT as the gold standard method to confirm the eradication of H. pylori infection(9).
In conclusion, several noninvasive H. pylori tests are established in clinical routine, but at present there is no single noninvasive method that can be considered the gold standard for the diagnosis of H. pylori infection.
According to ESPGHAN, the gold standard diagnostic for H. pylori infection remains at least two invasive diagnostic tests. Another prospective multicenter study is recommended to evaluate the specificity, sensitivity, along with the positive predictive value and the negative predictive value in our country.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
- Ravikumara M. Helicobacter pylori in children: think before you kill the bug!. Therap Adv Gastroenterol. 2023;16:17562848231177610.
- Aguilera Matos I, Diaz Oliva SE, Escobedo AA, Villa Jiménez OM, Velazco Villaurrutia YDC. Helicobacter pylori infection in children. BMJ Paediatr Open. 2020;4(1):e000679.
- Jones NL, Koletzko S, Goodman K, et al. Joint ESPGHAN/NASPGHAN Guidelines for the Management of Helicobacter pylori in Children and Adolescents (Update 2016). J Pediatr Gastroenterol Nutr. 2017;64(6):991-1003.
- Broekaert IJ, Borrelli O, Dolinsek J, et al. An ESPGHAN Position Paper on the Use of Breath Testing in Paediatric Gastroenterology. J Pediatr Gastroenterol Nutr. 2022;74(1):123-137.
- Imrie C, Rowland M, Bourke B, Drumm B. Limitations to carbon 13-labeled urea breath testing for Helicobacter pylori in infants. J Pediatr. 2001;139(5):734-737.
- Gold BD, et al. Helicobacter pylori infection in pediatric patients: Introduction. Gastroenterol Hepatol. 2014;10(Suppl 6):3-8.
- Kuloğlu Z, Kansu A, Kirsaçlioğlu CT, et al. A rapid lateral flow stool antigen immunoassay and (14)C-urea breath test for the diagnosis and eradication of Helicobacter pylori infection in children. Diagn Microbiol Infect Dis. 2008;62(4):351-356.
- Gatta L, Vakil N, Ricci C, et al. Effect of proton pump inhibitors and antacid therapy on 13C urea breath tests and stool test for Helicobacter pylori infection. Am J Gastroenterol. 2004;99(5):823-829.
- Pellicano R, Fagoonee S, Palestro G, Rizzetto M, Figura N, Ponzetto A. La diagnosi dell’infezione da Helicobacter pylori: raccomandazioni dal Maastricht 2-2000 Consensus Report [The diagnosis of helicobacter pylori infection: guidelines from the Maastricht 2-2000 Consensus Report]. Minerva Gastroenterol Dietol. 2004;50(2):125-133.
Articole din ediţiile anterioare
Îmbunătăţirea motricităţii fine la copiii cu nevoi speciale utilizând terapia ocupaţională
Terapia ocupaţională încearcă să dezvolte calitatea vieţii oricărei persoane a cărei capacitate funcţională este limitată, acest obiectiv fiind...
Urticaria autoimună
Afecţiunile alergice pot fi considerate boli sistemice, având în vedere polimorfismul simptomelor şi afectarea mai multor organe şi sisteme concomi...
Evaluarea managementului respirator la copiii cu distrofie musculară Duchenne
Distrofia musculară Duchenne este o boală genetică cu transmitere X-linkată, care afectează gena implicată în sinteza distrofinei. Nivelurile ...
Portal cavernoma in children – complications and evolution
Tromboza de venă portă este o afecţiune rară, dar reprezintă o cauză importantă de hipertensiune portală în patologia pediatrică. Principalii facto...