Chronic abdominal pain (CAP) represents one of the most frequent medical problems in pediatrics, both for patients and their families (affecting their quality of life), and for doctors and the healthcare system. In Western countries, its reported prevalence varies between 0.3% and 19% of children. When approaching CAP, doctors usually focus on visceral causes of the pain. If they are excluded, then implicitly the pain is considered to be functional (since the usual blood tests and the abdominal ultrasonography are normal). Parietal (somatic) causes of abdominal are usually ignored. Anterior cutaneous nerve entrapment syndrome (ACNES) represents a chronic neuropathic pain due to the compression of the anterior cutaneous branches of the thoracic intercostal nerves (Th 7-12), which penetrate the lateral margin of the rectus abdominis muscle. Although frequent, ACNES is rarely diagnosed, subjecting the patients to numerous unnecessary investigations (often invasive), leading to an improper management and increased medical costs. We present a scientific update on ACNES, regarding epidemiology, etiopathogenesis, physiopathology, pathology, diagnosis, therapeutic options and prognosis. We emphasize that ACNES represents a pure clinical diagnosis, no investigational technique being able to assess it. Early and correct recognition of ACNES is essential for pediatricians in their daily medical practice.
O cauză uitată a durerii cronice abdominale la copii: sindromul de compresiune a nervului cutanat anterior
A forgotten cause of chronic abdominal pain in children: anterior cutaneous nerve entrapment syndrome
First published: 22 octombrie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Pedi.59.3.2020.3897
Abstract
Rezumat
Durerea abdominală cronică (DAC) reprezintă una dintre cele mai frecvente probleme în pediatrie, atât pentru pacienţi/familie (afectând calitatea vieţii), cât şi pentru medici şi sistemul de sănătate. Frecvenţa DAC este de 0,3-19% în ţările vestice, la copiii de vârstă şcolară. În diagnosticul DAC, medicii pun accent pe cauzele intraabdominale organice; ceea ce nu este organic este considerat implicit funcţional (date fiind testele uzuale sanguine şi ecografia abdominală normală), ignorându-se durerea parietală (somatică). Sindromul de compresiune a nervului cutanat anterior (ACNES) reprezintă o durere cronică neuropatică şi este datorat compresiunii terminaţiilor nervoase anterioare ale nervilor intercostali toracici 7-12, care penetrează marginea laterală a muşchiului drept abdominal. Deşi frecvent, ACNES este rar diagnosticat, astfel încât pacienţii sunt frecvent supuşi multor investigaţii inutile, invazive şi unor terapii neadecvate, ducând la suferinţă prelungită şi la creşterea costurilor în sistemul de sănătate. Prezentăm date actuale legate de caracteristicile epidemiologice, etiopatogenetice, fiziopatologice, patologice, diagnostice, terapeutice şi prognostice ale acestui sindrom. Subliniem faptul că ACNES este un diagnostic pur clinic, astfel încât nu poate fi evidenţiat prin tehnici investigaţionale, oricât de sofisticate. Recunoaşterea precoce şi corectă a ACNES este absolut esenţială în practica medicilor pediatri.
Introduction
Chronic abdominal pain (CAP) in adults and children represents a debilitating condition. Its prevalence in children from Western countries is reported between 0.3% and 19%, hence the importance of this problem(1,2). Depending on its origin, pain may be classified as visceral (due to intraabdominal organ pathology), parietal (originating from the abdominal wall), or functional(1). A frequent cause of abdominal wall pain is represented by the anterior cutaneous nerve entrapment syndrome (ACNES), is defined as a chronic neuropathic pain syndrome due to the entrapment of anterior cutaneous terminal branches of thoracic intercostal nerves (Th 7-12), penetrating the rectus abdominis muscle, at its lateral border(3-5). Its diagnosis is based on patient’s history, pain characteristics, clinical bedside examination and a diagnostic injection of local anesthetics(1,6,7). However, this syndrome is underdiagnosed and undertreated, due to various reasons, such as: lack of ACNES description in current textbooks (including surgery, gastroenterology, neurology or gynecology), with consecutive lack of knowledge by both primary care physicians and gastroenterologists; absence of any anomaly of serological markers and of findings of other techniques (imaging, endoscopy etc.), as well as the consideration of only organic and functional causes of CAP, ignoring the somatic ones(1,4,6,8-13). Generally, when an organic cause is excluded, CAP is considered implicitly as being functional, resulting in inappropriate investigations and treatment(1). Thus, most children with ACNES had multiple useless investigations, often invasive, and improper therapy, including surgery, leading to unnecessarily increased costs of the medical care. On top of that, both patients and their families suffer from increased stress and discomfort(2).
The aim of our narrative review is to raise awareness on ACNES, in order to ensure its proper diagnosis and management among the medical community. By summarizing the currently available scientific literature, we provide updated knowledge on all aspects concerning ACNES (epidemiology, etiopathogenesis, anatomic pathology, physiopathology, positive and differential diagnosis, therapeutic options and prognosis on the short and long term).
Epidemiology
Incidence and prevalence
The general incidence in the general population is relatively unknown. A dedicated Dutch pain clinic estimated the incidence of ACNES to be 1/8000 in the general population (adults and children)(9).
Depending on different definitions and diagnostic criteria, out of all patients with CAP, ACNES is reported in 15-30% of them(4,14,15). In an emergency department, 2% of the patients presenting with acute abdominal pain were reported to have ACNES(9). The same Dutch pain clinic reported one out of eight adolescents (13%) to be diagnosed with ACNES(7). In our European area, the frequency of ACNES must be quite high, as a single pediatric center from Croatia reported 38 children, during a follow-up median time of 1.7 years (1-2.7 years)(6). Most reports from literature present between 1 and 3 cases(10); however, there are also studies reporting on 7(16), 8(8), 9(17), 12(7) and even 71(1) and 85 patients(18). Probably, its true incidence and prevalence are underestimated(1).
Gender
All pediatric studies show a definite predominance in females, ranging from 76%(18), 77%(1), 78%(17) to 86%(16) and 92%(7), without providing a clear explanation.
Age at onset
Most published studies report a mean or a median of 15 years old, with extremes of 10 and 18 years old(7), 9 and 16 years old(8), 11 and 16 years old(14), and 8 and 17 years old(16).
Etiopathogenesis and pathology
The exact cause of ACNES is unknown, such as most of its triggers (75% in pediatrics)(1). Other researchers reported either sports activities or previous surgical or medical events, such as appendectomy, inguinal hernia repair, cholecystectomy, infections (gastrointestinal, urinary tract, respiratory)(1,2,4), trauma(1,19), or oral contraceptives(20,21).
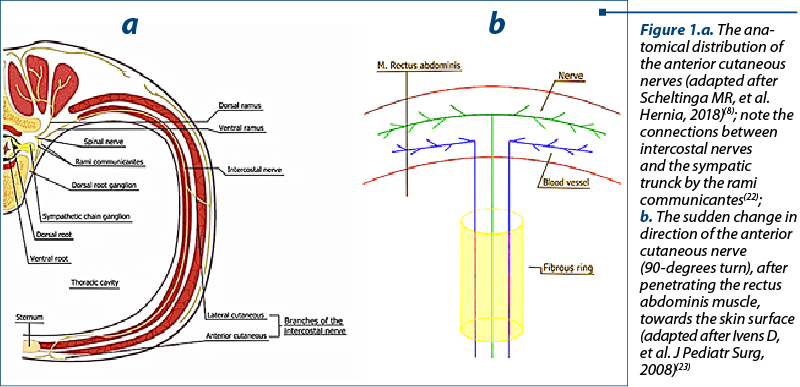
The supposed mechanism is represented by peripheral nerve entrapment, at the lateral border of the rectus abdominis muscle(4). Just underneath the rectus abdominis muscle, the intercostal nerves make a 90-degree turn toward the skin and tunnel outward through fibrous tunnels in the muscle(1,10) to innervate the skin. This sharp turn anchors the nerves at that location, making them vulnerable to injury. The compression or stretching of a nerve or its tunnel can result in severe pain(4). The simplified scheme of the area anatomy, including the fibrous ring and the 90-degree angle, is presented in Figure 1.
Physiopathology
Besides the sudden 90-degrees turn, several other mechanisms may be involved. The pain can be additionally caused by muscle spasm, altered dimensions of fibrous ring due to the herniation of its content, nerve swelling and progressive entrapment, leading to a vicious cycle(3,4,8,24). This vicious cycle explains the chronic character of the pain, specific for ACNES. With regard to trauma or sports activities, these can generate stretching or twisting of the nerves, leading to severe pain. Oral contraceptives were also found to be involved in the occurrence of ACNES(20). Sexual steroids can produce local tissue edema, therefore causing ACNES. It is well known that estrogen promotes the accumulation of subcutaneous fat in contrast to visceral fat. Consequently, it was supposed that pain may occur as a result of the compression of the fat in the abdominal wall. The high prevalence of ACNES in adolescents can be explained by the increased endogenous sex steroids. This is associated with acute weight gain and fat deposition in the abdominal wall(21). Moreover, the anterior cutaneous nerves are accompanied in their way through the rectus muscle by an artery and vein, forming a bundle. The bundle can herniate in case of increased abdominal pressure, leading to mechanical irritation and pain. A recent study attempted to uncover the exact mechanism leading to ACNES, by analyzing the histopathological findings of the resected nerves from children with ACNES. All specimens presented nonspecific nerve degeneration. In the majority of the specimens, the immunohistochemical staining did not show any signs of inflammation. Therefore, these findings support the hypothesis that ACNES is produced by compression rather than inflammation or infection(25). The characteristic abdominal pain can be accompanied by pseudovisceral symptoms. These phenomena denote a segmental relationship between affected intercostal nerves and internal organs via splanchnic chains, as presented in Figure 1a(22).
Positive diagnosis
Clinical presentation
a. Acute or chronic abdominal pain (dominant symptom)
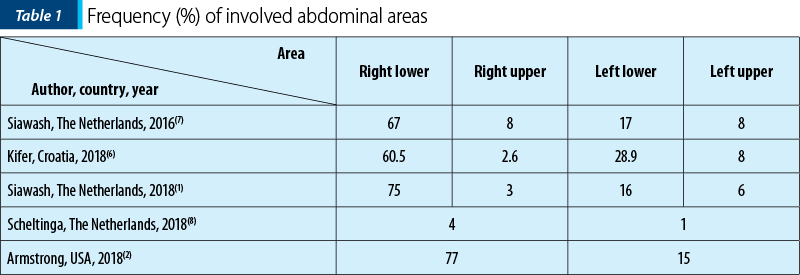
Location: usually unilateral (bilateral in <10% of cases, at an identical level)(1), localized (the same small spot of approximately 2 cm2, where the nerve is entrapped), reproducible, along the lateral margin of rectus abdominis muscle. In most cases, the thoracic 10-11 dermatomes are involved(1). The most frequent location is the lower right quadrant, ranging from 50% to 75%(1,7,25). However, all other quadrants can be involved and their frequency is presented in Table 1.
Irradiation: favoured by twisting, bending, stretching, lifting or coughing, the pain may irradiate along the ribs towards the back or towards the upper half abdomen (the same side)(4,8).
Sensation: perceived as superficial stabbing, burning or dull pain; altered perception of light touch (hypo-/hyperesthesia) or cold temperature may be associated(6,7).
Intensity: it varies from bearable to debilitating (7-10/10) and can be exacerbated by physical activity (body stretching, running, walking), coughing, sneezing or certain types of clothing. Lying down may relieve the pain (in most cases); however, occasionally it may worsen it(1,4,8).
Pattern: frequently described as a renal or biliary colic(4).
Timetable: both diurnal and nocturnal(4).
Chronic pain: unpredictable course; it can be present for a variable period of time (days, weeks), then disappear even for long periods (months, years) and then reappear again. This will render patients more anxious, hopeless and even attempt suicide(1,4).
b. Visceral or “pseudovisceral” symptoms
The most commonly reported symptoms include loss of appetite, nausea, vomiting, bloating, constipation or urgency to defecation. Consequently, patients may present with weight loss. Less often, sweating and dizziness are also reported(1,8,10). These symptoms/signs should be strongly remembered as possibly associated with ACNES, otherwise they may suggest an organic or functional cause, delaying the correct diagnosis.
Physical examination
There are several steps that aid the positive diagnosis of ACNES.
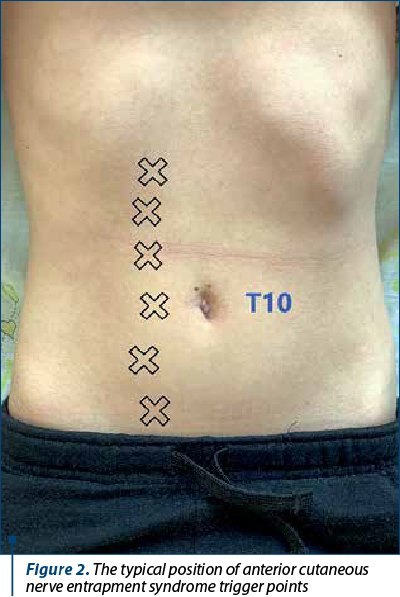
a. Pain identification – a clear identification of the aponeurotic openings is needed. Then, the patient is asked to point the painful area using one finger. Consecutively, the investigator will palpate the indicated area along the lateral margin of the rectus abdominis muscle. The optimal position to identify the pain at the lateral border of the rectus abdominis muscle is while standing, with the abdomen bulging upwards (Figure 2). The most typical site is T11 on the right side or T11 and T10 on the left side. The level of the umbilicus corresponds with intercostal nerve T10(1,9).
b. Carnett’s sign (positive in 100% of cases) – while in supine position, the patient is being asked to raise his or her head or feet from the surface, while the investigator pushes on the tender spot. If the superficial palpation of the reported painful area provokes substantial pain while rectus muscles are tightened, the test is considered positive. However, there are other instances when the Carnett’s test is positive, such as herniation, myositis or myofascial disruptions(8,9,18).
c. Altered skin sensitivity – identified on a larger area covering the small area of maximal pain, including hypoesthesia, hyperesthesia, hyperalgesia, even allodynia or a change of cool perception, while they are absent on the contralateral side. These modifications are demonstrated by using a swab (positive in 83% of cases) or an alcohol soaked gauze (positive in 92% of cases)(7).
d. Pinch test (positive in 83% of cases) – elicits hyperalgesia, while the investigator pinches a skinfold containing skin and subcutaneous tissue between thumb and index finger. The test is positive if the patient experiences an unusual severe pain compared to other abdominal areas(7,9).
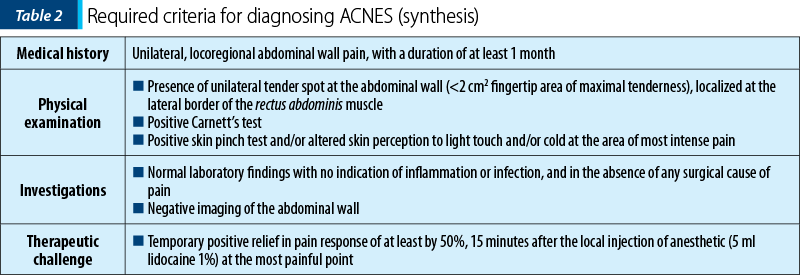
Criteria required for diagnosis
The first physician to examine the patient must establish the diagnosis of ACNES(4), in order to avoid unnecessary investigations and improper management. However, the overall median pain duration from onset to diagnosis varies between 4 months(26) and 10 months (1-60 months)(1). When bilateral ACNES is involved, an even longer diagnostic delay of 18 months (3-48 months) is reported(1). Currently, there are no gold standard criteria for the diagnosis of ACNES. Therefore, a combination of typical findings in patient’s history and a thorough physical examination are necessary. The commonly used diagnostic criteria are presented in Table 2(1,7,18).
Differential diagnosis
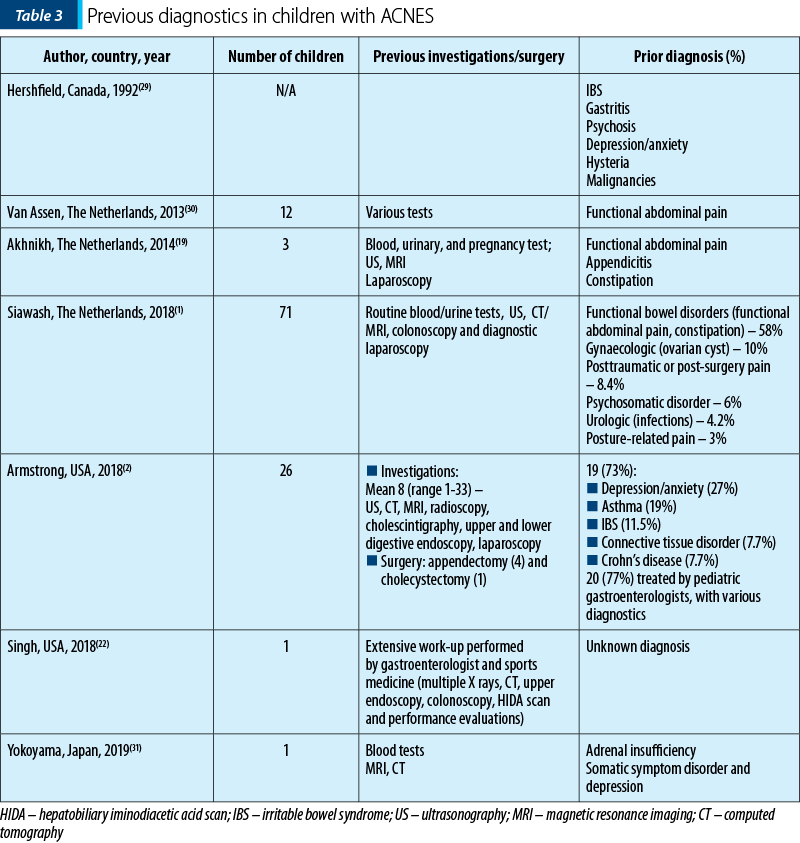
As mentioned before, visceral causes are considered by physicians in the first instance. Multiple investigations are used. If no visceral cause is found, then many other diagnostics (especially functional) are taken under consideration. Abdominal wall is reported in a minority of cases. Very often, patients diagnosed eventually with ACNES report repeated visits to the general practitioners and specialists from clinics/hospitals (gastroenterologists, surgeons, emergency care doctors, pediatricians, neurologists, psychiatrists, rheumatologists)(12,19,28). Table 3 presents previous diagnostics in children finally diagnosed with ACNES.
Indeed, ACNES is very often misdiagnosed as irritable bowel syndrome (IBS). Very recently, Siawash et al. designed a 17-item questionnaire to aid the differentiation between IBS and abdominal wall pain. The questionnaire proved to be a good diagnostic test and could be used to differentiate between abdominal wall pain and IBS(32). Other wall disorders that could mimic ACNES include: abdominal myofascial pain syndrome, hernias, abdominal wall tumors and endometriosis, hematoma, abdominal wall tear, scar tissue originating from appendectomy, caesarean section, laparoscopy, rib-related disorders such as rib-tip syndrome, slipping rib syndrome and other rib abnormalities, herpes zoster, radiculopathies such as traumatic and diabetic, ilioinguinal or iliohypogastric nerve entrapment, sportsman hernia or sports groin/pubalgia and vertebral column abnormalities including herniated disk, exaggerated lumbar lordosis, leg length difference(8,24).
Treatment and prognosis
Currently, there are two treatment strategies to manage ACNES: nonsurgical and surgical(24). The most accepted protocol in children includes the following(7): local injection of anesthetic (5 ml lidocaine 1%) at the most painful point with or without ultrasound guidance, positive relief in pain response of at least by 50% after 15 minutes. If the pain reoccurs after two weeks, then local anesthetic (4 ml lidocaine 1%) combined with 40 mg of metylprednisolon (1 ml) must be administered. If the pain still reoccurs, then surgery (anterior neurectomy) is recommended. Even though the effects of corticosteroids are considered, recent studies did not report an increase in the proportion of the patients with successful response to injection(33). The immediate effect was reported after the first injection with anesthetic in 97% of the patients, of which 15% had a sustained effect. Also, 22.3% required repeated injections with anesthetic even combined with corticosteroids, of which 38% had a sustained effect (mean 17 months, extremes 4-39 months)(18). The recent systematic review by Markus et al. reported a treatment success after anterior neurectomy ranging from 86% to 100%, during a follow-up duration of 4 weeks to 36 months. They also mentioned one study where 78% of the patients gained pain relief after anterior neurectomy with occasional pain during physical exertion(34). Besides surgical anterior neurectomy, other techniques could be used, with various efficacy: chemical neurolysis, radiofrequency ablation and neuromodulation sometimes in combination with systemic medication (like non-steroidal antiinflammatory drugs, weak opioids and drugs generally used for neuropathic pain, such as antiepileptics [gabapentin and pregabalin] and antidepressants [amytriptiline])(24). Roderick et al. reported good results after the administration of amytriptiline and lidocaine patches combined with paracetamol(35). However, ACNES was not relieved by NSAIDS, muscle relaxants, tramadol and gabapentin in two patients(24). Nizamuddin et al. did not report any effect of systemic drugs administered before interventional therapy. Therefore, systemic medication is generally not useful(36). A very recent systematic review of all studies published in children up to February 25, 2020(34) proposed a step-up treatment strategy. This strategy was also advanced in other studies(7,18). This involves administering injections with a local anaesthetic agent such as lidocaine or bupivacaine into the trigger point. The injection can be performed using a freehand technique or ultrasound guided, with or without corticosteroids. If the pain is reduced by 50% in approximately 15 minutes, then ACNES is treated, as well as positively confirmed(34). The same authors suggested that ultrasound guided injection is the method of choice, allowing injection of the anaesthetic closer to the nerve. In case of multiple injections, usually more than 7, successful only for a short period of time, the next step to be considered is anterior neurectomy. Data regarding the recurrence rate are still limited. However, Markus et al. reported two studies, one retrospective and one prospective, with the recurrence rate after anterior neurectomy(34). The retrospective study showed recurrence of ACNES in 11% of the patients, with a median time until recurrence of 3 months(2). The prospective one mentioned new onset (in a different location) of ACNES in 8% of the patients(6). Both the injections and surgery are good viable treatment options with good treatment success(34). As directions for future perspectives, a very recent paper showed that ultrasound examination revealed a perforator artery with its characteristic low peak systolic velocity at the site of the pain. These ultrasonographic findings may facilitate a more accurate and objective diagnosis of ACNES(37); however, they have to be proven in prospective well-designed research.
Conclusions
ACNES is a typical clinical diagnosis. The positive diagnosis is based on key findings from the patient’s history and physical examination. Therefore, ACNES should be considered in children above 8 years of age, with CAP located usually in the right lower abdomen, especially in females. A combination of positive Carnett’s test and pinch test is compatible with a diagnosis of ACNES. In terms of treatment, a step-up strategy is suggested to be the best approach. This strategy starts with an injection with a local anesthetic with or without ultrasound guidance and with or without adding corticosteroids. This is followed by surgery (anterior neurectomy) if pain is persistent. The dissemination of information about ACNES among the medical community could lead to a faster diagnosis and to the avoidance of multiple unnecessary diagnostic procedures.
Bibliografie
-
Siawash M, Roumen R, Ten WTA, van Heurn E, Scheltinga M. Diagnostic characteristics of anterior cutaneous nerve entrapment syndrome in childhood. Eur J Pediatr. 2018; 177(6):835-839.
-
Armstrong LB, Dinakar P, Mooney DP. Neurectomy for anterior cutaneous nerve entrapment syndrome in children. J Pediatr Surg. 2018; 53(8):1547-1549.
-
Mol FMU, Lataster A, Scheltinga M, Roumen R. Anatomy of abdominal anterior cutaneous intercostal nerves with respect to the pathophysiology of anterior cutaneous nerve entrapment syndrome (ACNES): A case study. Transl Res Anat. 2017; 8-9:6-10.
-
Applegate W. Abdominal cutaneous nerve entrapment syndrome (ACNES): A commonly overlooked cause of abdominal pain. Perm J. 2002; 6(3):20-27.
-
Sahoo RK, Nair A. Ultrasound guided transversus abdominis plane block for anterior cutaneous nerve entrapment syndrome. Korean J Pain. 2015; 28(4):284–286.
-
Kifer T, Mišak Z, Jadrešin O, Hojsak I. Anterior cutaneous nerve entrapment syndrome in children: A prospective observational study. Clin J Pain. 2018; 34(7):670-673.
-
Siawash M, De Jager-Kievit JWA, Ten WTA, Roumen RM, Scheltinga MR. Prevalence of anterior cutaneous nerve entrapment syndrome in a pediatric population with chronic abdominal pain. J Pediatr Gastroenterol Nutr. 2016; 62(3):399-402.
-
Scheltinga MR, Roumen RM. Anterior cutaneous nerve entrapment syndrome (ACNES). Hernia. 2018; 22(3):507-516.
-
van Assen T, Brouns JAGM, Scheltinga MR, Roumen RM. Incidence of abdominal pain due to the anterior cutaneous nerve entrapment syndrome in an emergency department. Scand J Trauma Resusc Emerg Med. 2015; 23(1).
-
Bishop WP. The wall of pain: Not all abdominal pain is visceral. J Pediatr Gastroenterol Nutr. 2016; 62(3):359-360.
-
DiGiusto M, Suleman M-I. Anterior cutaneous nerve entrapment syndrome in a pediatric patient previously diagnosed with functional abdominal pain: a case report. A&A Pract. 2018;11(5):134-136.
-
Thome J, Egeler C. Abdominal cutaneous nerve entrapment syndrome (ACNES) in a patient with a pain syndrome previously assumed to be of psychiatric origin. World J Biol Psychiatry. 2006; 7(2):116-118.
-
Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2016; 150(6): 1456-1468.e2.
-
Kanakarajan S, High K, Nagaraja R. Chronic abdominal wall pain and ultrasound-guided abdominal cutaneous nerve infiltration: a case series. Pain Med. 2011; 12(3):382-386.
-
Lindsetmo RO, Stulberg J. Chronic abdominal wall pain – a diagnostic challenge for the surgeon. Am J Surg. 2009; 198(1):129-134.
-
Skinner AV, Lauder GR. Rectus sheath block: successful use in the chronic pain management of pediatric abdominal wall pain. Paediatr Anaesth. 2007; 17:1203.
-
Bairdain S, Dinakar P, Mooney DP. Anterior cutaneous nerve entrapment syndrome in children. J Pediatr Surg. 2015; 50(7):1177-1179.
-
Siawash M, Maatman R, Tjon A, Ten W, van Heurn E, Roumen R, Scheltinga M. Anterior neurectomy in children with a recalcitrant anterior cutaneous nerve entrapment syndrome is safe and successful. J Pediatr Surg. 2017; 52(3):478-480.
-
Akhnikh S, De Korte N, De Winter P. Anterior cutaneous nerve entrapment syndrome (ACNES): The forgotten diagnosis. Eur J Pediatr. 2014; 173(4):445-449.
-
Peleg R. Abdominal wall pain caused by cutaneous nerve entrapment in an adolescent girl taking oral contraceptive pills. J Adolesc Health. 1999; 24:45.
-
Omura D, Obika M, Iwamuro M, et al. Anterior cutaneous nerve entrapment syndrome possibly triggered by oral contraceptives. Intern Med. 2019; 58(10):1507-1509.
-
Singh G, Nasany R, Zidan A. Chronic abdominal pain due to anterior cutaneous nerve entrapment syndrome, a diagnosis almost missed. J Pain. 2018; 19(3):S35.
-
Ivens D, Wojciechowski M, Vaneerdeweg W, Vercauteren M, Ramet J. Abdominal cutaneous nerve entrapment syndrome after blunt abdominal trauma in an 11-year-old girl. J Pediatr Surg. 2008; 43(5).
-
Chrona E, Kostopanagiotou G, Damigos D, Batistaki C. Anterior cutaneous nerve entrapment syndrome: Management challenges. J Pain Res. 2017; 10:145-156.
-
Markus J, van Montfoort M, de Jong JR, de Beer SA, Aronica EMA, Gorter RR. Histopathologic examination of resected nerves from children with anterior cutaneous nerve entrapment syndrome: Clues for pathogenesis? J Pediatr Surg. 2020 [in press].
-
Scheltinga MR, Boelens OB, A Ten WET, Roumena RM. Surgery for refractory anterior cutaneous nerve entrapment syndrome (ACNES) in children. J Pediatr Surg. 2011; 46: 699–703.
-
Choi YK, Chou S. Rectus syndrome. Another cause of upper abdominal pain. Reg Anesth. 1995; 20:347–51.
-
McLaughlin C, Gandhi A, Hamner CE. Anterior cutaneous neurectomy for chronic abdominal wall pain: A case report and review of the literature. J Pediatr Surg Case Reports. 2017; 22:44-46.
-
Hershfield NB. The abdominal wall. A frequently overlooked source of abdominal pain. J Clin Gastroenterol. 1992; 14(3):199-202.
-
van Assen T, de Jager-Kievit JWAJ, Scheltinga MR, Roumen RMH. Chronic abdominal wall pain misdiagnosed as functional abdominal pain. J Am Board Fam Med. 2013; 26(6):738-744.
-
Yokohama N, Shiraki R, Watanabe T, Shiinoki M, Nin M, et al. Difficult differentiation of a somatic symptom disorder from anterior cutaneous nerve entrapment syndrome (ACNES): a case report. BMC Psychiatry. 2019; 19:394.
-
Siawash M, van Assen T, Tjon A, et al. Abdominal wall pain or irritable bowel syndrome: validation of a pediatric questionnaire. J Pediatr Gastroenterol Nutr. 2019; 69(3):e65-e69.
-
Mol FMU, Jansen CH, Boelens OB, et al. Adding steroids to lidocaine in a therapeutic injection regimen for patients with abdominal pain due to anterior cutaneous nerve entrapment syndrome (ACNES): a single blinded randomized clinical trial. Scand J Pain. 2018; 18(3):505-512.
-
Markus J, Sibbing IC, Ket JCF, de Jong JR, de Beer SA, Gorter RR. Treatment strategies for anterior cutaneous nerve entrapment syndrome in children: A systematic review. J Pediatr Surg. 2020 [in press].
-
Roderick B, Norman B. Anterior cutaneous nerve entrapment syndrome: an unusual cause of abdominal pain during pregnancy. Int J Obstet Anesth. 2016; 25:96–97.
-
Nizamuddin SL, Koury KM, Lau ME, Watt LD, Gulur P. Use of targeted transversus abdominis plane blocks in pediatric patients with anterior cutaneous nerve entrapment syndrome. Pain Physician. 2014; 17(5):E623–E627.
-
Hata J, Imamra H. Sonographic diagnosis of abdominal cutaneous nerve entrapment syndrome: a report of two cases. Japanese Journal of Gastroenterology and Hepatology. 2020; V3(4):1-4.
Articole din ediţiile anterioare
Urticaria autoimună
Afecţiunile alergice pot fi considerate boli sistemice, având în vedere polimorfismul simptomelor şi afectarea mai multor organe şi sisteme concomi...
Sleep-related breathing disorders in the pediatric patient with Prader-Willi syndrome
Sindromul Prader-Willi (PWS) este o boală genetică rară, întâlnită cu o incidenţă de 1:15000 de nou-născuţi, identificată la toate rasele şi car...
Caracteristica genotipurilor şi fenotipurilor infecţiei rotavirale în cadrul supravegherii de tip santinelă din Republica Moldova
Potrivit Organizaţiei Mondiale a Sănătăţii, peste 700 de milioane de episoade de diaree la copiii cu vârsta sub 5 ani şi aproximativ 40% din ...
Provocările tratamentului stomatologic la copiii cu tulburări de spectru autist
În literatura de specialitate, unii autori folosesc termenul de „epidemie de autism”, care poate fi explicată de creşterea „conştientizării” priv...