Materials and method. The aim of the study is to evaluate the management of acute pain in newborn patients hospitalized in the neonatal intensive care unit of the “Sf. Maria” Emergency Clinical Hospital for Children, Iaşi. The study is prospective, conducted between 1.10.2020 and 1.12.2020, on a group of 15 newborn patients with surgical conditions. For each of these maneuvers, the intensity of pain was assessed using the baseline CRIES scale, at 1 minute, at 10 minutes, and one hour after starting the maneuver, considering as an indicator of insufficient analgesia a CRIES score higher than 4. Based on a predetermined protocol, analgesic drugs were administered preventively, as well as curatively. The quality of the treatment was finally evaluated according to the one-hour CRIES score and to the parental satisfaction score. Results. The one-hour CRIES score (Ch1) for low-intensity pain-generating maneuvers (PGM) was 2.30/patient. No patient had a score greater than or equal to 4, so as to require therapeutic intervention. The one-hour CRIES score (Ch1) for PGM of moderate intensity had a mean value of 2.26/patient. All patients had a score lower than 4 and did not require therapeutic intervention, demonstrating that the therapeutic protocol was effective. For the maneuvers producing high intensity pain, the CRIES score per hour had an average value of 2.4 per patient, all patients having score values below 4, proving that the drug therapeutic protocol was effective. The average satisfaction score of the parents was 6.73, with values over 5 to 12 of the relatives, out of a total of 15 respondents, representing 80% of the total, which we consider satisfactory. Conclusions. The CRIES scale is an effective tool for assessing newborn pain for all types of pain-generating maneuvers. Preventive therapeutic intervention is extremely important. The therapeutic protocol must be modified to combine at least two analgesics administered preventively, with sufficient time before the onset of pain-generating maneuvers. The curative treatment should be performed according to the CRIES score at 1 and at 10 minutes after the onset of PGM, using the polymodal technique, opiate drugs being an important resource.
Studiu prospectiv privind managementul durerii acute la nou-născutul cu afecţiuni chirurgicale prin corelaţia scalei de durere CRIES cu protocolul terapeutic etapizat
Prospective study regarding the management of acute pain in neonates with surgical diseases through the correlation of the CRIES pain scale with the staged therapeutic protocol
First published: 16 decembrie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Pedi.60.4.2020.4074
Abstract
Rezumat
Materiale şi metodă. Scopul studiului este evaluarea managementului durerii acute la pacienţii nou-născuţi spitalizaţi în unitatea de terapie intensivă a Spitalului Clinic de Urgenţe pentru Copii „Sf. Maria”, Iaşi. Studiul este prospectiv, realizat în perioada 1.10.2020-1.12.2020, pe un lot de 15 pacienţi nou-născuţi cu afecţiuni chirurgicale. Pentru fiecare din aceste manevre s-a evaluat intensitatea durerii prin intermediul scalei CRIES, bazal, la 1 minut, la 10 minute şi la o oră de la debutul manevrei, considerându-se indicator al analgeziei insuficiente un scor CRIES mai mare decât 4. Pe baza unui protocol prestabilit, s-au administrat medicamente antalgice, atât preventiv, cât şi curativ. Calitatea tratamentului s-a evaluat, în final, în funcţie de scorul CRIES, la o oră, alături de scorul de satisfacţie al părinţilor. Rezultate. Scorul CRIES la o oră (Ch1) pentru manevrele generatoare de durere (MGD) de intensitate mică a avut o valoare de 2,30/pacient. Niciun pacient nu a avut un scor mai mare sau egal cu 4, astfel încât să necesite intervenţie terapeutică. Scorul CRIES la o oră pentru MGD de intensitate medie a avut o valoare medie de 2,26/pacient. Toţi pacienţii au avut un scor mai mic decât 4 şi nu au necesitat intervenţie terapeutică, acest lucru demonstrând că protocolul terapeutic a fost eficient. Pentru manevrele producătoare de durere de intensitate mare, scorul CRIES la o oră a avut o valoare medie de 2,4 per pacient, toţi pacienţii având valori ale scorului sub 4, demonstrând că protocolul terapeutic medicamentos a fost eficient. Media scorului de satisfacţie al părinţilor a fost de 6,73, cu valori de peste 5 la 12 dintre aparţinători, din totalul de 15 chestionaţi, reprezentând 80%, ceea ce considerăm satisfăcător. Concluzii. Scala CRIES este un instrument eficient pentru evaluarea durerii la nou-născut, pentru toate tipurile de manevre generatoare de durere. Intervenţia terapeutică preventivă este extrem de importantă. Protocolul terapeutic trebuie modificat în sensul asocierii a cel puţin două analgezice administrate preventiv, cu un timp suficient de mare înainte de debutul manevrelor generatoare de durere. Tratamentul curativ trebuie realizat în conformitate cu scorul CRIES la 1 şi la 10 minute după debutul MGD, folosindu-se tehnica polimodală, medicamentele opiacee fiind o resursă importantă.
Introduction
The last 2-3 decades have brought major changes in the management of pain in the newborn. First of all, the conception of the perception of pain by the newborn has completely changed. If until 30 years ago it was considered that newborns do not perceive pain, or they perceive it at a much lower intensity than normal, the recent years have shown otherwise(1). Numerous studies published especially in the last 10 years have attested the fact that, on the contrary, newborns perceive pain, and that, moreover, due to the immaturity of the inhibitory descending central nervous system, they perceive it excessively, at a much higher intensity(2). There are also numerous studies which show that inadequate pain management in neonatal age leads to multiple changes in pain perception in childhood and adulthood(3). As such, pain management in the newborn has now become much more applied, based on a rigorous assessment of pain intensity. Subsequent treatment is staged, based on scores of various scales imagined to assess pain in the newborn. The drugs used are varied, polymodal therapy being the most commonly used. New types of antiinflammatory drugs are used, such as ketorolac, paracetamol, but also opiates such as morphine and fentanyl, remifentanyl and tramadol(4).
Materials and method
The aim of the study is to evaluate the management of acute pain in newborn patients hospitalized in the neonatal intensive care unit of the “Sf. Maria” Emergency Clinical Hospital for Children, Iaşi, newborns who have undergone surgery or not, and who needed pain treatment.
The study is prospective, conducted between 1.10.2020 and 1.12.2020 on a number of 15 newborn patients with gestational ages between 32 and 40 weeks. These patients were hospitalized in the neonatal intensive care unit of the “Sf. Maria” Emergency Clinical Hospital for Children for surgical conditions, most of them being operated and mechanically ventilated postoperatively. These patients underwent hospitalization pain-generating maneuvers that were classified into three types:
-
Low-intensity pain-generating maneuvers – changing diapers and primary toilet, dressing the surgical wound, changing the position in the incubator, installing a nasogastric tube, installing a urinary tube.
-
Medium-intensity pain-generating maneuvers – peripheral venous puncture for branula installation, arterial puncture for arterial catheter installation, tracheal aspiration on the intubation tube, peripheral blood gas collection, peripheral venous puncture analysis, oral aspiration pharyngeal and nasopharyngeal.
-
Maneuvers generating high-intensity pain – surgical operation, installation of central venous catheter, orotracheal intubation, tracheal aspiration on laryngoscope, puncture for thoracic drainage, puncture for abdominal drainage.
In all patients, the intensity of the pain caused by the three types of maneuvers was assessed by means of a scale, widely used in neonatological practice. This is the CRIES-1995 scale (Crying, Requires oxygen saturation, Increased vital signs, Expression, Sleeplessness). This scale takes into account five parameters, three of them behavioral, namely crying, facial expression and lack of sleep, as well as two vital parameters, these being the need for oxygen in conditions of peripheral saturation less than 95% and the cardiovascular parameter represented the increased heart rate and/or blood pressure. For each of these five parameters there is an evaluation from 0 to 2, thus the maximum score is 10, and the minimum is 0.
The CRIES score was evaluated in all patients admitted to the intensive care unit, every 4 hours during hospitalization, and before performing pain-provoking maneuvers, naming this score as the baseline CRIES score. The CRIES score was also evaluated for the maneuvers producing low-intensity pain, at 1 minute, at 10 minutes and one hour after the maneuver. The same was done for the maneuvers producing medium- and high-intensity pain, the CRIES score being evaluated at 1 minute, at 10 minutes and one hour after the maneuver.
Also, in all patients, the therapeutic response to analgesic drugs administered according to the CRIES score was evaluated.
The following protocol was used to treat pain in the newborns in the study: for low-intensity pain-producing maneuvers, no preventive analgesics were administered prior to the start of the maneuver. However, if at 1 minute or at 10 minutes the CRIES score was greater than or equal to 4, metamizole (Algocalmin®) 20 mg/kg b.w. or paracetamol 10 mg/kg b.w. were administered. In patients who experienced moderate-intensity pain maneuvers, metamizole or paracetamol were administered preventively 30 minutes before the start of the maneuver. If the score at 1 minute or 10 minutes after the maneuver was greater than or equal to 4, an additional dose of metamizole or paracetamol was administered. If the score was greater than or equal to 6, a dose of tramadol 1 mg/kg b.w. was administered. In patients who underwent painful interventions provoking high-intensity pain, a dose of tramadol 1 mg/kg b.w. was administered preventively with 30 minutes before starting the maneuver. If at 1 minute or 10 minutes after the maneuver the analgesic score was between 4 and 6, a dose of metamizole or paracetamol was added. At a analgesic score greater than 6, the dose of tramadol was repeated. Exceptions were mechanically ventilated patients in whom, if the CRIES score was greater than or equal to 6 at 1 minute or 10 minutes after the maneuver, a dose of fentanyl of 1 mcg/kg b.w. was administered. If at the CRIES score, calculated one hour after the painful maneuver, the value was between 4 and 6, a dose of metamizole or paracetamol was administered, and if the value was higher than 6, a dose of tramadol was administered in unventilated patients or one dose of fentanyl in those mechanically ventilated.
For patients in whom the baseline CRIES score assessed at 4 hours, in the absence of a pain-provoking maneuver, was between 4 and 6, a dose of metamizole or paracetamol was administered. If the CRIES score was 6 or higher, a dose of tramadol was administered in unventilated patients, or fentanyl in ventilated patients.
In this study, the distribution by sex, the number of days of hospitalization, whether patients were operated or not, whether they were mechanically ventilated or not, and the number of hours of mechanical ventilation were analyzed. The number of low-intensity, medium- and high-intensity pain-provoking maneuvers for each patient was also analyzed throughout the hospital stay. Correlations were made between these types of maneuvers and CRIES scores that were performed before the start of the maneuvers, at 1 and at 10 minutes for the maneuvers provoking low-intensity pain, before the maneuvers, at 1 minute, at 10 minutes and at one hour, for medium-intensity and high-intensity pain-provoking maneuvers. The therapeutic analgesic measures that were instituted for CRIES scores greater than or equal to 4 for all three types of pain-provoking maneuvers were also analyzed. Correlations were made between the therapeutic maneuvers instituted to combat pain and the one-hour CRIES scores. The satisfaction of patients in the study correlated with CRIES scrutiny was also estimated and analyzed.
Results
The study included a number of 15 newborn patients with gestational ages between 32 and 40 weeks. Of these, three had a gestational age of less than 36 weeks and 12 had a gestational age of 36 weeks or more. All patients studied were hospitalized between 1.10.2017 and 30.11.2017 in the neonatal surgical intensive care unit of the “Sf. Maria” Emergency Clinical Hospital for Children. Out of the total number of patients, 10 were males and 5 were females. The total number of hospitalization days for the entire group of 15 patients studied was 227 days, with an average of 15.13 days/patient. The diseases for which they were hospitalized in the neonatal intensive care unit were of a surgical but diverse type, each newborn being hospitalized for at least one organ dysfunction. Out of the total number of newborns, five were unoperated and 10 were operated, the surgical interventions being of variable magnitude. Eight newborns were mechanically ventilated, and seven did not require mechanical ventilation. The number of hours of mechanical ventilation varied from 2 to 340 hours, the total number of hours being 773, with an average of 99.62 hours per patient.
The evolution of the patients was favorable in 14 cases, registering only one death in a newborn with diaphragmatic hernia, severe pulmonary hypertension and severe secondary respiratory failure.
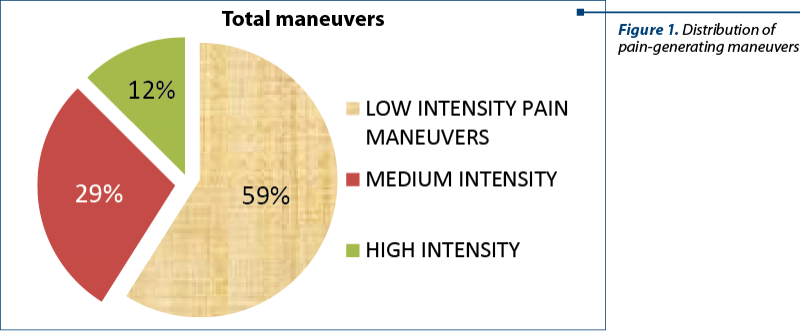
All patients hospitalized during the study period, in intensive care, were subjected to pain-producing maneuvers. The total number of pain-producing maneuvers for all patients was 1518, with an average of 101.2 maneuvers per patient throughout hospitalization and 6.92 maneuvers per patient per day of hospitalization. There were a total of 895 maneuvers producing low-intensity pain, with an average of 59 maneuvers per patient, respectively 3.85 maneuvers producing low-intensity pain per patient per day. There were a total of 433 maneuvers producing pain of medium intensity throughout the hospitalization and in all patients, with an average of 36.2 per patient and 2.39 maneuvers per patient per day. Maneuvers producing high-intensity pain were a total of 190 cumulated in all patients and throughout the hospitalization, with an average of 12.66 per patient, respectively 0.82 per patient and per day.
The assessment of pain intensity in all patients was performed with the CRIES scale, at the hospitalization of patients in intensive care, before each pain-producing maneuver, at one minute, at 10 minutes and one hour after these maneuvers. The CRIES and routine score was also performed at 4 hours throughout the hospitalization of patients in neonatal intensive care.
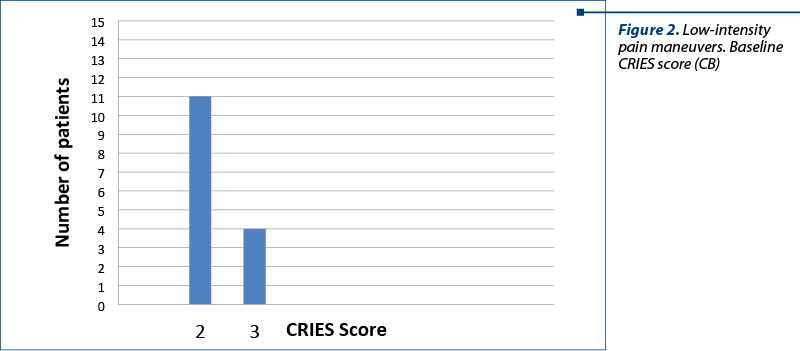
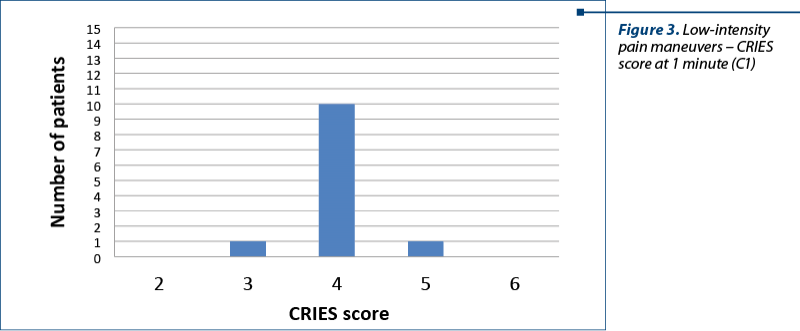
For low-intensity pain-producing maneuvers, the baseline CRIES score (CB) had an average value of 2.53 per patient, with no patient with a score greater than or equal to 4. At one minute (C1), the mean value was of 4.2 per patient, with 14 patients (93.31%) with a CRIES score higher than 4 and requiring therapeutic intervention.
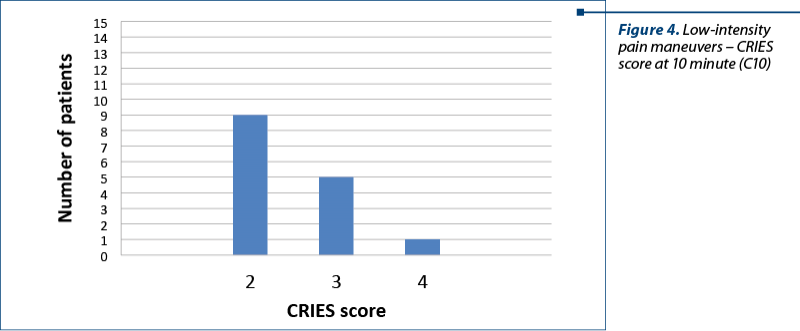
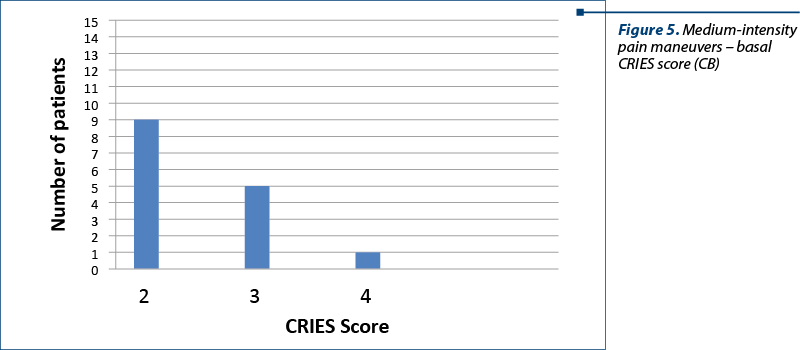
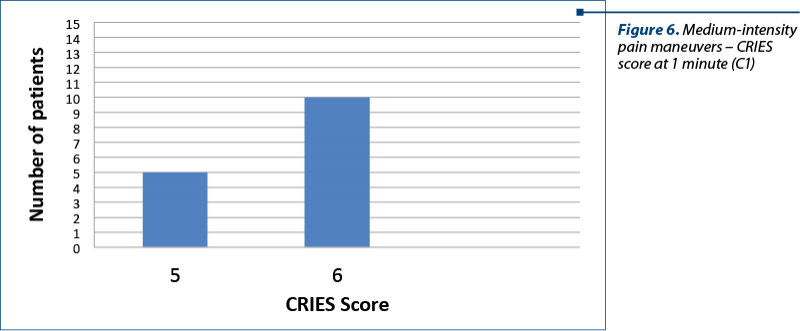
At 10 minutes (C10), with an average value of 2.46 per patient, there was a single patient (6.66%) with a CRIES score greater than or equal to 4. For maneuvers producing pain of medium intensity, the mean baseline CRIES score was 2.26 per patient, with only one patient (6.66%) with a value greater than or equal to 4. The average CRIES score at 1 minute was 5.66 per patient, all 15 patients having a value greater than or equal to 4.
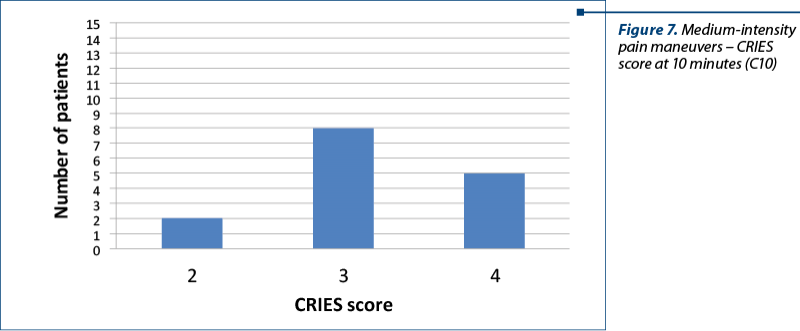
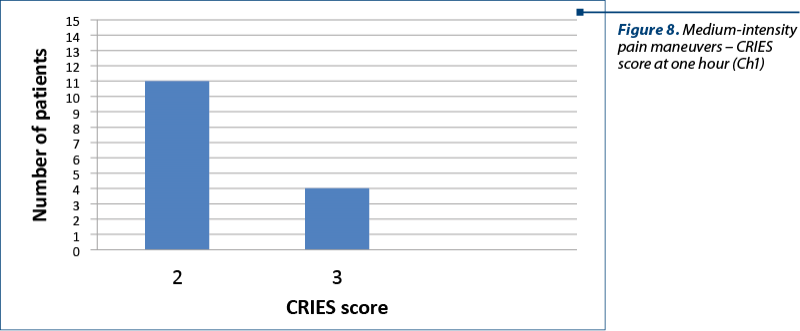
The mean CRIES score at 10 minutes was 3.2 per patient, with five patients (33.33%) having a score greater than or equal to 4. The mean CRIES score at one hour after performing these maneuvers (C1H) had an average value of 2.26 per patient, all patients having a score lower than 4.
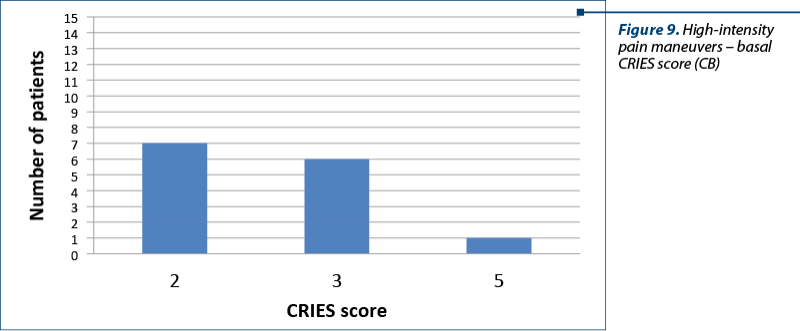
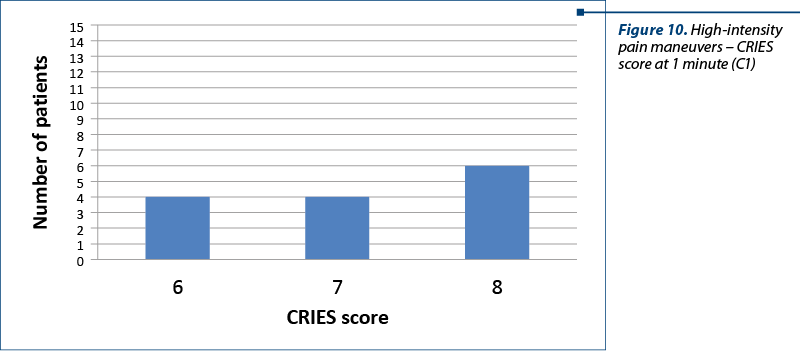
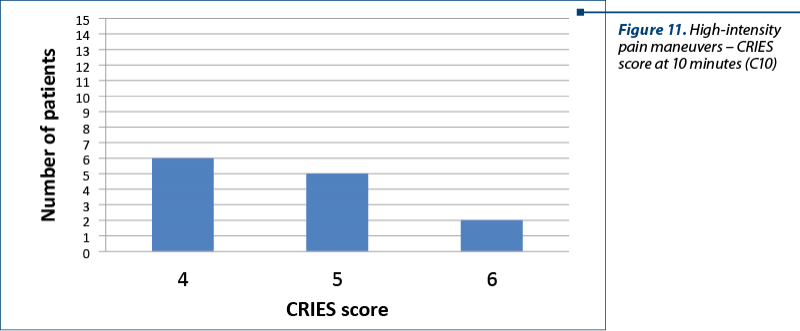
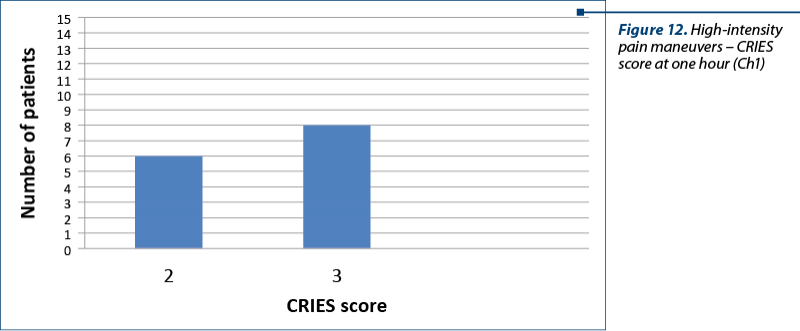
For the maneuvers producing high-intensity pain, the baseline CRIES score (CB) had an average value of 2 per patient, only one patient (6.66%) having a value greater than or equal to 4. The CRIES score per minute had a mean value of 6.66 per patient, with 14 patients (93.33%) with a value greater than or equal to 4. CRIES score at 10 minutes (C10) had a mean value of 4.5 per patient, with 13 patients (86.66%) with a score greater than or equal to 4. The CRIES score per hour (C1H) had an average value of 2.4 per patient, all patients having score values below 4.
The CRIES score achieved systematically at 4 hours, not corroborated with the pain-producing maneuvers, had an average value of 3.66, with only five (33.33%) patients with score values greater than or equal to 4 and requiring therapeutic intervention.
Depending on the CRIES score, as described in the material and method chapter, analgesic drugs such as metamizole (Algocalmin®), paracetamol, tramadol or fentanyl were administered. These analgesic administrations were performed both before the medium- and high-intensity pain-producing maneuvers and when the CRIES score was between 4 and 6 or greater than 6.
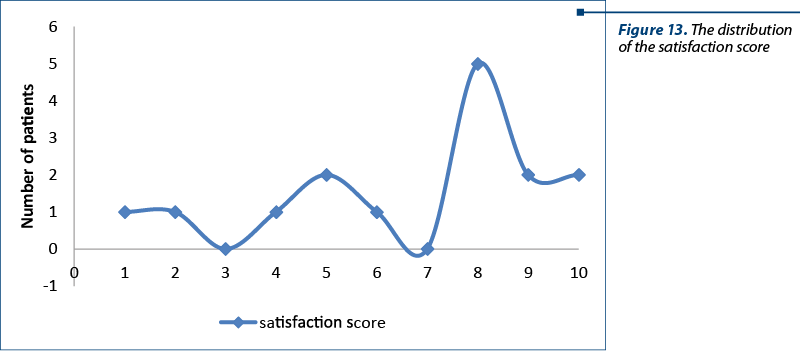
Pain therapy in newborns admitted to the neonatal surgical intensive care unit was qualitatively assessed by the degree of satisfaction of the members of the neonatal patients studied. Patients’ satisfaction was assessed after their interrogation, being rated from 1 to 10.
The quality of patients’ analgesia was considered satisfactory, given that the satisfaction score of the relatives was higher than 5. The average satisfaction score of the parents was 6.73, with values over 5 to 12 of the relatives, out of a total of 15 respondents, representing 80% of the total.
Discussion
The assessment and therapy of acute pain in a neonatal surgical intensive care unit are difficult and a real problem for the medical staff. In our study, we used a group of 15 newborns hospitalized during two months in the neonatal intensive care unit of the Pediatric Surgery Clinic of the “Sf. Maria” Emergency Clinical Hospital for Children, Iaşi. The gestational age of the newborns in the group was between 32 and 40 weeks, which allowed us to use the CRIES scale for pain intensity assessment. This scale is widely used in neonatal practice since 1995 and is only used in newborns over 32 weeks of gestational age(5).
The gender distribution in the studied group did not have any implications in the working methodology and the results of the study.
The total number of hospitalization days in all patients in the group, cumulatively, was 227 days, with an average of 15.3 days per patient, correlating with data from the literature(6,7,8). The patients were hospitalized for various surgical conditions that were not evaluated in detail, considering only the pain-generating maneuvers performed on newborns in the treatment process for these conditions, and less the conditions themselves.
Out of the total of 15 newborns, 10 were operated on, five being unoperated, this being important for the newborns who underwent surgery who were subjected to more pain-generating maneuvers, of medium and high intensity, than the unoperated ones. A total of 8 newborns, representing 53.33%, were mechanically ventilated, this being important for the study, as ventilated newborns were subjected to more pain-generating maneuvers than unventilated ones, such as mobilization and taping, endotracheal aspiration, or change of intubation probe.
Out of a total of 15 newborns in the group, only one death was recorded in a patient with diaphragmatic hernia and severe pulmonary hypertension, along with severe acute respiratory failure treated with ventilator. This death cannot be correlated with the quality of pain management, the death being most likely caused by the condition itself, generating severe organ dysfunctions.
The pain-generating maneuvers in the patients in our group were 1518, with an average of 101.2/patient/hospitalization, respectively 6.92/patient/day. These data do not fully correlate with those in the literature, where the average per patient per day is around 10. This discrepancy may be due to the lack of staff in neonatal intensive care where the study was conducted, and the poor quantification of these pain-generating maneuvers(9,10,11).
The maneuvers generating low-intensity pain had an average of 3.85/patient/day, those of average intensity – 2.39/patient/day, while those of high-intensity pain were 0.82/patient/day. Of all the pain-generating maneuvers in terms of daily average/patient, it is best to correlate with the data in the literature of high-intensity pain-generating maneuvers. The value of 0.82/patient/day recorded in our study is close to 1/patient/day communicated in the literature data(12). For low- and medium-intensity pain-generating maneuvers, mean/patient/day values were lower in our study than in data published in the literature. As mentioned before, the cause was the lack of rigor in quantifying them due to the lack of specialized staff in the care of newborns.
As mentioned in the study methodology, for all three types of pain-generating maneuvers (PGM), the CRIES score was evaluated before the start of the CRIES-base (CB) score maneuver, one minute after the start of the maneuver (C1), at 10 minutes (C10), and at one hour (Ch1).
For low-intensity pain-provoking maneuvers, the baseline CRIES score (CB) had a mean value of 2.53/patient. No patient had a score greater than or equal to 4.
The CRIES score achieved at 1 minute for low-intensity PGM had a value of 4.2/patient. Fourteen patients (93.31%) had C1 greater than or equal to 4, requiring therapeutic intervention according to the study protocol.
The fact that such a large number of patients had a C1 greater than or equal to 4 per minute is most likely due to the absence of prophylactic therapeutic maneuvers to prevent pain, which were performed before the onset of low-intensity pain-generating maneuvers.
The 10-minute CRIES score (C10) for low-intensity pain-generating maneuvers was 2.46/patient. Only one patient (6.66%) had a C10 greater than or equal to 4, requiring therapeutic intervention(13,14,15). This suggests that the therapeutic maneuvers performed for patients who had C1 greater than or equal to 4 were effective and that the chosen protocol is effective for this type of therapeutic intervention.
The one-hour CRIES score (Ch1) for low-intensity pain-generating maneuvers was 2.30/patient. No patient had a score greater than or equal to 4, in such a way as to require therapeutic intervention.
For the provocative maneuvers of medium intensity pain, the baseline CRIES score (CB) had an average value of 2.26/patient. Only one patient (6.66%) had a CB greater than or equal to 4, requiring therapeutic intervention(16,17,18).
For the maneuvers generating medium intensity pain, the CRIES score at 1 minute (C1) had an average value of 5.66/patient. However, all patients had a C1 greater than or equal to 4, requiring therapeutic intervention(19). This suggests that the preventive therapeutic maneuvers performed according to the study protocol before the onset of medium-intensity pain-generating maneuvers were ineffective. There are two possibilities: either the drugs chosen under the protocol had insufficient potency to prevent a CRIES pain score greater than or equal to 4, or the time between the administration of these drugs and the onset of PGM was too short for the drugs to take action. This will need to be addressed by changing the protocol for the administration of analgesics to prevent moderate-intensity PGM(20,21,22,23).
The 10-minute CRIES score (C10) for moderate-intensity PGM had a mean value of 3.2/patient. A total of five patients (33.33%) had a C10 greater than or equal to 4.
This suggests that analgesic drugs administered according to the protocol in patients who had a C1 greater than or equal to 4 were only partially effective. It is therefore necessary to adjust the therapeutic protocol for this situation as well(24,25,26,27).
The one-hour CRIES score (Ch1) for PGM of moderate intensity had a mean value of 2.26/patient. All patients had a score lower than 4 and did not require therapeutic intervention. This shows that the therapeutic protocol in the study to combat pain in patients who had a C10 greater than or equal to 4 was effective.
High-intensity pain-generating maneuvers had a mean baseline CRIES score of 2/patient. Only one patient (6.66%) had a value greater than or equal to 4, requiring therapeutic intervention(28).
The high-intensity pain-generating maneuvers had a CRIES score at one minute (C1) with a mean value of 6.66/patient. However, a number of 14 patients (93.33%) had C1 greater than or equal to 4, requiring therapeutic intervention. This shows that the prevention treatment in the protocol for high-intensity PGM was inefficient. It is necessary to modify the protocol either in the sense of increasing the analgesic prevention drugs, or in the sense of increasing the time interval between the time of administration of the analgesic drugs and the moment of the onset of high intensity PGM.
High-intensity PGM had a CRIES score at 10 minutes (C10), with a mean value of 4.5. A number of 13 patients (86.66%) had a C10 score greater than or equal to 4, requiring therapeutic intervention. These results show that the analgesic drugs used in the protocol for patients who had a C1 greater than or equal to 4 were partially effective, and that the protocol needs to be modified(28,29,30).
High-intensity PGMs had an hourly CRIES score (Ch1) with a mean value of 2.4/patient. All patients had Ch1 values lower than 4 and did not require therapeutic intervention(31,32,33). This shows that the therapeutic intervention performed in patients with high-intensity PGM who had a CRIES score at 10 minutes (C10) greater than or equal to 4 was effective(34,35,36,37).
In our study, the quality of pain management was also assessed by a satisfaction score of the patients belonging to the study group. The quality of analgesia was considered satisfactory if that the satisfaction score of the relatives was higher than 5. This score was achieved by questioning the parents of the newborns in the group. They gave a grade from 1 to 10 for the quality of analgesia. The average satisfaction score was 7.33. Out of the total number of patients studied, 12 patients (80%) gave a grade above 5 for the quality of analgesia.
Conclusions
The CRIES scale is an effective tool for assessing the presence of pain and its intensity in the newborn with gestational age between 32 and 40 weeks, for all types of PGM.
The preventive therapy is extremely important in pain management to achieve a CRIES score less than 4 at 1 and at 10 minutes, for all types of PGM.
The therapeutic protocol should be modified in the sense of combining at least two analgesics administered preventively, long enough before the onset of PGM.
The curative treatment should be performed according to the CRIES score at 1 and at 10 minutes after the onset of PGM, using the polymodal technique, opiate drugs being an important resource.
Bibliografie
-
Weiner J, Sharma J, Lantos J, Kilbride H. How infants die in the neonatal intensive care unit: trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2011;165(7):630–634.
-
Balaguer A, Martin-Ancel A, Ortigoza-Escobar D, Escribano J, Argemi J. The model of palliative care in the perinatal setting: a review of the literature. BMC Pediatr. 2012;12:25. http://dx.doi.org/10.1186/1471-2431-12-25.
-
Meert KL, Thurston MA, Sarnaik AP. End-of-life decision making and satisfaction with care: parental perspectives. Pediatr Crit Care Med. 2000;1(2):179–185.
-
Philips DM. JCAHO pain management standards are unveiled. Joint Commission on Accreditation of Healthcare Organizations. J Am Med Assoc. 2000;285(4):428–429.
-
Carter B, Jones P. Evidence-based comfort care for neonates towards the end of life. Semin Fetal Neonat Med. 2013;18 (2):88–92.
-
Craig KD, Korol CT, Pillai RR. Challenges of judging pain in vulnerable infants. Clin Perinatol. 2002;29(3):445–457.
-
Cignacco E, Hamers J, van Lingen RA, et al. Neonatal procedural pain exposure and pain management in ventilated preterm infants during the first 14 days of life. Swiss Med Wkly. 2009;139(15-16):226–232.
-
Carbajal R, Rousset A, Dana C, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. J Am Med Assoc. 2008;300(1):60–70.
-
Simons SHP, van Dijk M, Anand KJS, Roofthooft D, van Lingen RA, Tibboel D. Do we still hurt newborn babies? Arch Pediatr Adolesc Med. 2003;157(11):1058–1064.
-
Mancuso T, Burns J. Ethical concerns in the management of pain in the neonate. Pediatr Anesth. 2009;19(10):953–957.
-
Ferrell B. Ethical perspectives on pain and suffering. Pain Manag Nurs. 2005;6(3):83–90.
-
Hall RW. Anesthesia and analgesia in the NICU. Clin Perinatol. 2012;39(1):239–254.
-
Fahnenstach H, Steffan J, Kau N, Bartmann P. Fentanyl-induced chest wall rigidity and laryngospasm in preterm and term infants. Crit Care Med. 2000;28(3):836–839.
-
Vaughn PR, Townsend SF, Thilo EH, McKenzie S, Moreland S, Denver KK. Comparison of continuous infusion of fentanyl to bolus dosing in neonates after surgery. J Pediatr Surg. 1996;31(12): 1616–1623.
-
Harlos MS, Stenekes S, Lambert D, Hohl C, Chochinov HM. Intranasal fentanyl in the palliative care of newborns and infants. J Pain Sympt Manag. 2013;46(2):265–274.
-
Bouwmeester NJ. Age and therapy-related effects on morphine requirements and plasma concentrations of morphine and its metabolites in postoperative infants. Br J Anaesth. 2003;90(5):642–652.
-
Dijk M, Bouwmeester NJ, Duiven voorden HJ, et al. Efficacy of continuous versus intermittent morphine administration after major surgery in 0-3 year old infants; a double-blind randomized controlled trail. Pain. 2002;98(3):305–313.
-
Lynn AM, Nespeca MK, Bratton SL, Shen DD. Intravenous morphine in postoperative infants: intermittent bolus dosing versus targeted continuous infusions. Pain. 2000;88(1):89–95.
-
Borenstein-Levin L, Synnes A, Grunau RE, Miller SP, Yoon EW, Shah PS. Canadian Neonatal Network Investigators. Narcotics and sedative use in preterm neonates.
-
J Pediatr. 2017;180 (1):92–98.
-
McClain BC, Probst LA, Pinter E, Hartmannsgruber M. Intravenous clonidine use in a neonate experiencing opioid-induced myoclonus. Anesthesiology. 2001;95(2):549–550.
-
Finn D, Collins A, Murphy BP, Dempsey EM. Mode of neonatal death in an Irish maternity centre. Eur J Pediatr. 2014;173(11):1505–1509.
-
Zimmerman KO, Hornik CP, Ku L, Watt K, Laughon MM, Bidegain M. Sedatives and analgesics given to infants in neonatal intensive care units at the end of life. J Pediatr. 2015;167(2):299–304.
-
Sankaran K, Hedin E, Hodgson-Viden H. Neonatal end of life care in a tertiary care centre in Canada: a brief report. Chinese J Contemp Pediatr. 2016;18(5):379–385.
-
Gilmour D, Davies MW, Herbert AR. Adequacy of palliative care in a single tertiary neonatal unit. J Paediatr Child Health. 2017 Feb;53(2):136-144.
-
Partridge JC, Wall SN. Analgesia for dying infants whose life support is withdrawn or withheld. Pediatrics. 1997;99(1):76–79.
-
Provoost V, Cools F, Bilsen J, et al. The use of drugs with a life-shortening effect in end-of-life care in neonates and infants. Intensive Care Med. 2006;32(1):133–139.
-
Hauer JM. Treating dyspnea with morphine sulfate in nonverbal children with neurological impairment. Pediatr Pulmonol. 2015;50(4):e9–e12.
-
Garcia-Salado A, de Paso-Mora MG, Monleon-Luque M, Martino-Alba R. Palliative care in children with spinal muscular atrophy type 1: what do they need? Palliat Support Care. 2015;13(2):313–317.
-
Cohen SP, Dawson TC. Nebulized morphine as a treatment for dyspnea in a child with cystic fibrosis. Pediatrics. 2002;110(3): e38–e40.
-
Irikura M, Minamni E, Ishitsuka Y, Kawase A, Kondo Y, Irie T. Abnormal movements of Japanese infants following treatment with midazolam in a neonatal intensive care unit: incidence and risk factors. ISRN Pharmacol. 2012;2012:950603 http://dx.doi.org/10.5402/2012/950603.
-
Ng E, Taddio A, Ohlsson A. Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev. 2012(6):CD002052 http://dx.doi.org/10.1002/14651858.CD002052.pub2
-
Baleine J, Milesi C, Mesnage R, et al. Intubation in the delivery room: experience with nasal midazolam. Early Hum Develop. 2014;90(1):39–43.
-
Tobias JD. Pentobarbital for sedation during mechanical ventilation in the pediatric ICU patient. J Intensive Care Med. 2000;15(2):115–120.
-
Van der Marel CD, Peters JWB, Bouwmeester NJ, Jacqz-Aigrain E, Van den Arker JN, Tibboel D. Rectal acetaminophen does not reduce morphine consumption after major surgery in young infants. Br J Anaesth. 2007;98(3):372–379.
-
Hong JY, Han SW, Kim WO, Kil HK. Fentanyl sparing effects of combined ketorolac and acetaminophen for outpatient inguinal hernia repair in children.
-
J Urol. 2010;113(3):1551–1555.
-
Ceelie I, de Wildt SN, van Dijk M, et al. Effect of intravenous paracetamol on postoperative morphine requirements in neonates and infants undergoing major noncardiac surgery: a randomized controlled trial. J Am Med Assoc. 2013;309(2):149–154.
-
Saroyan JM, Tresgallo ME, Farkouh C, et al. The use of oral ketamine for analgesia with dressing change in an infant with epidermolysis bullosa: report of a case. Pediatr Dermatol. 2009;26 (6):764–765.
Articole din ediţiile anterioare
Maternal preeclampsia effects on newborn – review
Preeclampsia este o afecţiune frecventă în prezent, până la 5-10% dintre sarcini fiind asociate cu această boală. Pe lângă efectele devastatoare ...
The impact of postnatal depression on the health and development of the newborn
Depresia prenatală şi postnatală reprezintă un factor de risc pentru buna dezvoltare a sugarului şi nou-născutului, cu repercusiuni care se întind ...
Icterele neonatale
Icterul apare la nou-născut la o valoare de peste 5 mg/dl bilirubină totală, faţă de adult, la care icterul este vizibil la valori ale bilirubinei ...
Consequences of anemia in pregnancy upon the newborn – a cross-sectional study
Anemia la gravide este încă o problemă importantă de sănătate publică. Consecinţele asupra nou-născutului, imediate sau tardive, pot varia de la ...