Introduction. Schizophrenia is a serious disorder that influences all aspects of the patients’ life. The most important goals in schizophrenia are remission, recovery, and improving psychosocial functioning and quality of life. Unfortunately, there are important barriers to achieving optimal long-term outcomes in this disease due to patient-related factors and treatment-related factors. Lack of insight is considered the main reason for partial/non-adherence and, therefore, for the long-term outcome.
Aim. The aim of this study was to identify the predictive factors involved in long-term schizophrenia, and especially the role of the awareness of illness.
Materials and method. Eighty patients (44 males and 36 females) recruited from the First and Second Psychiatric Clinic from Cluj-Napoca, diagnosed according to ICD-10 criteria with schizophrenia, participated in this study. A semi-structured interview collected the demographical data. Psychotic symptoms were evaluated using Positive and Negative Syndrome Scale (PANSS), severity of the disease using Clinical Global Impression (CGI) and insight using the Scale for the Assessment of Unawareness of Mental Disorder (SUMD), the Schedule for Assessment of Insight-Expanded version (SAI-E) and Beck Cognitive Insight Scale (BCIS).
Results. Our results showed that, among potential predictors of psychotic symptoms change measured in this research, those significantly correlated with changes are the level of insight measured with SUMD scale (r=-0.41; p<0.01), presence of family history (r=0.24; p<0.05), and belonging to urban areas (r=0.23; p<0.05). The level of insight, as one predictor, with PANSS initially controlled, explained 16% of variance of improving psychotic symptoms during hospitalization. Also, patients from urban areas seem to have a slight tendency towards higher magnitudes of the changes (low correlation, but statistically significant). Again, the square of the correlation obtained (coefficient of determination) indicates that urban membership explaines 5% of variance when symptoms improve. Also, it seems that the family history is positively associated with the magnitude of symptoms’ change, but the level of this relationship is also reduced.
Conclusions. The awareness of illness is one of the predictive factors for long-term schizophrenia, and the best predictive model of disease progression is composed of variables SUMD total and PANSS total on admission.
Predictors of schizophrenia clinical evolution
Predictori ai evoluţiei clinice a schizofreniei
First published: 30 iunie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.73.2.2023.8256
Abstract
Rezumat
Introducere. Schizofrenia este o afecţiune gravă, care influenţează toate aspectele vieţii pacientului. Cele mai importante obiective în schizofrenie sunt remisiunea, recuperarea, îmbunătăţirea funcţionalităţii psihosociale şi a calităţii vieţii. Din păcate, există bariere importante în obţinerea unei bune evoluţii pe termen lung, determinate de factori dependenţi de pacient şi de factori legaţi de tratament. Lipsa conştientizării bolii este considerată principalul motiv pentru aderenţa parţială/lipsa aderenţei şi deci pentru evoluţia pe termen lung.
Obiective. Scopul acestui studiu este de a identifica factorii predictivi implicaţi în evoluţia pe termen lung a schizofreniei şi în special rolul conştientizării bolii.
Materiale şi metodă. 80 de pacienţi (44 de bărbaţi şi 36 de femei) din Clinicile de Psihiatrie I şi II din Cluj-Napoca, diagnosticaţi conform ICD-10 cu schizofrenie, au participat la studiu. Datele demografice au fost colectate printr-un interviu semistructurat. Simptomele psihotice au fost evaluate folosind scala PANSS, severitatea bolii a fost evaluată cu ajutorul CGI, iar pentru evaluarea capacităţii de conştientizare a bolii au fost utilizate scalele SUMD, SAI-E şi BCIS.
Rezultate. Rezultatele noastre au arătat că, dintre potenţialii predictori ai schimbării simptomatologiei psihotice măsuraţi în această cercetare, corelate semnificativ cu aceste schimbări se dovedesc a fi doar nivelul de insight măsurat cu ajutorul scalei SUMD (r=-0,41; p<0,01), prezenţa antecedentelor heredocolaterale (r=0,24; p<0,05) şi apartenenţa la mediul urban (r=0,23; p<0,05). Nivelul de insight, ca singur predictor, cu PANSS iniţial controlat, explică 16% din varianţa îmbunătăţirii simptomatologiei psihotice pe parcursul internării. De asemenea, pacienţii din mediul urban par a avea o uşoară tendinţă spre magnitudini mai mari ale acestei schimbări (corelaţie redusă, dar semnificativă statistic). Şi în acest caz, pătratul corelaţiei obţinute (coeficientul de determinare) indică faptul că apartenenţa la mediul urban explică 5% din varianţa îmbunătăţirii simptomatologiei. De asemenea, se pare că prezenţa antecedentelor heredocolaterale se asociază pozitiv cu magnitudinea schimbării simptomatologiei, însă nivelul acestei relaţii este de asemenea redus.
Concluzii. Capacitatea de conştientizare a bolii este unul dintre factorii predictivi pentru evoluţia pe termen lung a schizofreniei şi cel mai optim model predictiv este cel compus din variabilele PANSS total şi SUMD total la internare.
Cuvinte-cheie: conştientizarea bolii, insight, psihopatologie, evoluţia pe termen lung a schizofreniei
1. Introduction
Schizophrenia is one of the most severe mental disorders, but its essential nature remains to be clarified. The global age-standardized point prevalence of schizophrenia in 2016 was estimated to be 0.28%(1). Unfortunately, there are important barriers to achieving optimal outcomes in this disease due to patient-related factors (males, single status, uneducated, unemployed, frequently or ever-used drugs or alcohol)(2), as well as treatment-related factors associated with favorable outcomes (antipsychotic medication adherence)(3). Insight refers to a multidimensional construct with distinct but interrelated subdomains: awareness of illness, consequences of illness, need for treatment and illness attribution(4). Interestingly, schizophrenia patients with severely impaired insight report a more positive perception regarding quality of life and illness severity, as opposed to physician evaluation or those with unimpaired insight(5). Psychopharmacological and psychological treatments can significantly reduce symptoms of schizophrenia but, overall, the disease is associated with a high number of hospital admissions and long-term use of psychiatric services(6,7). Our research aimed to identify the psychometric predictive factors involved in the clinical outcome of schizophrenia.
Method
We conducted a prospective cross‑sectional study including 80 patients admitted to the Psychiatry Clinic of the County Emergency Clinical Hospital Cluj-Napoca, diagnosed according to the 10th edition of the International Classification of Diseases (ICD-10) with schizophrenia, aged between 19 and 73 years old, with an educational level of minimum eight years of study (grades), and voluntary research inform consent singed. The exclusion criteria consisted in the presence of mental retardation, organic cerebral syndromes, alcohol and psychoactive substances abuse, epileptic seizures, and pregnancy or lactation. The patients were evaluated twice during their hospitalization, first after the admission and, secondly, before releasing from hospital.
A semi-structured interview collected the socio-demographical data. The psychotic symptoms were evaluated using the Positive and Negative Syndrome Scale (PANSS)(8), and the severity of the disease was assessed using the Clinical Global Impression (CGI). Insight was measured using the Scale for the Assessment of Unawareness of Mental Disorder (SUMD)(9-11), the Schedule for Assessment of Insight-Expanded Version (SAI-E)(12), and the Beck Cognitive Insight Scale (BCIS)(13). For the descriptive analysis, we used indicators of central tendency (arithmetic mean) and the dispersion (standard deviation, minimum and maximum values). Where the sample was analyzed simultaneously in terms of two categorical variables (e.g., gender × adherence to treatment), charts were constructed based on contingency tables and the association of variables was tested using the nonparametric chi-square correlation coefficient for categorical variables. The materiality of these values was tested at a significance level less than 0.05. To test the effectiveness of intervention on psychotic symptoms and the level of insight, from admission to discharge, we choose the dependent samples t test – i.e., repeated measurements. For statistically significant differences, we also calculated the size of intervention effect based on Cohen’s d coefficient.
Results
Our group consisted of 55% male patients and 45% female patients, the mean age was 35.76 ± 10.95 years old (range: 19-73 years old), the average age of illness onset was 27.24 ± 8.81 (range: 16-57 years old) and the average number of hospitalizations was 5.13 ± 5.64 (range: 0-35 hospitalizations). Our psychometric evaluation revealed the following results.
The progression of psychotic symptoms and insight from admission to discharge
CGI and PANSS progression
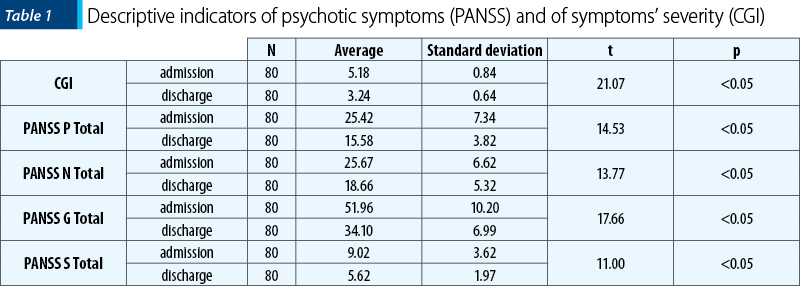
Table 1 presents the descriptive indicators of psychotic symptoms measured by PANSS and for the severity of symptoms measured by the CGI scale.
The results show a significant reduction in the severity of psychotic symptoms at discharge compared with its level on admission, with a large effect size, according to the Cohen’s d indicator (d=2.59). Also, there were significant reductions in psychotic symptoms measured by PANSS, for both positive and negative symptoms’ subscales, both with large effect sizes (positive d=1.68; negative d=1.16; total d=2.04).
SUMD progression
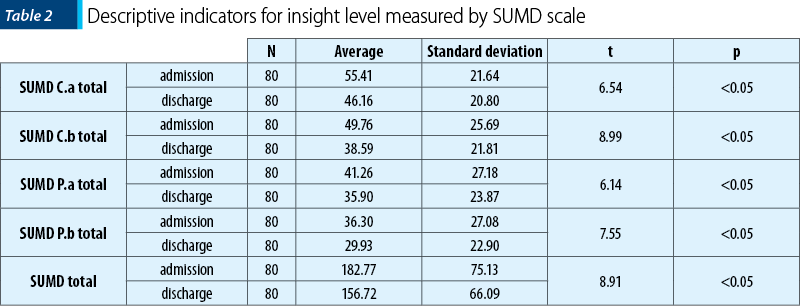
We note that for this scale high scores mean low levels of insight. Table 2 presents descriptive indicators of scores’ progression for insight, and wrong attribution of current and past symptoms.
As it can be seen in Table 2, following insight average column at admission and discharge, for every SUMD subscale and, as well, for total score, there is a downward trend indicating a decrease of non-insight (high SUMD scores show a high level of non-insight). T test with repeated measurements performed for each of these variables showed that these decreases are statistically significant for both insight and wrong attribution of current symptoms (SUMD C.a total for insight, and SUMD C.b for the attribution of current symptoms), and also for insight and wrong attribution of past symptoms (SUMD P.a for insight, and SUMD P.b for the attribution). By using Cohen’s d indicator, we calculated the size of these effects and we found average values for current symptomatology (d current insight = 0.43; d current attribution = 0.46) and reduced values for past symptoms (d past insight = 0.20; d past attribution = 0.25).
SAI-E progression
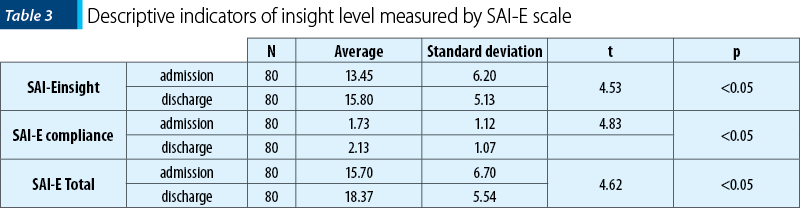
We note that for this scale high scores mean high levels of insight. Table 3 presents descriptive indicators of scores’ progression for insight and treatment compliance scales and for total score.
Dependent samples t-test performed in each of these cases confirms the statistically significance of these trends for subscales of insight, treatment compliance, and for total insight score. As the sizes of these effects highlighted by the Cohen’s d indicator, they are medium to low (d insight = 0.41; d compliance = 0.36; d SAI-E total = 0.43).
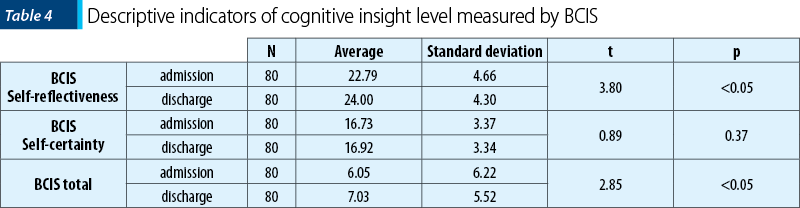
BCIS progression
The third scale of insight analysis is BCIS cognitive insight scale. Table 4 presents the descriptive indicators of progression from admission to discharge.
Following the progression of cognitive insight average levels for every subscale and for total scores, we find that these values record an upward trend from admission to discharge. Dependent sample t-test revealed that this ascendent trend is statistically significant only for self-reflectiveness scale and for cognitive insight total score. For self-certainty scale, this trend is not statistically significant, and Cohen’s d indicator showed low and very low values for the effect at BCIS scales (d self-reflectiveness = 0.26; d self-certainty = 0.05; d total BCIS = 0.16).
Predictors of symptoms progression measured
by PANSS
Further on, we are interested to highlight the significant predictors for psychotic symptoms’ progression from admission to discharge. The analysis was set up based on some steps.
Step one – We defined the variable “∆ PANSS” as the difference between PANSS scores at admission and discharge, and tested the correlation of this variable according to baseline PANSS score. If there was a strong correlation, that means that the initial level of symptoms explained a significant proportion of variance of disease progression.
Step two – We tested the correlation of all the various potential predictors of change in magnitude of change (Δ PANSS), controlling the initial level of symptoms (PANSS score at baseline) using partial correlation.
Step three – We introduced the significant partial correlates of change as predictors in multiple linear regression equation to compare their predictive values for the magnitude of change in PANSS (progression of the disease from admission to discharge) and to determine the optimal predictive model.
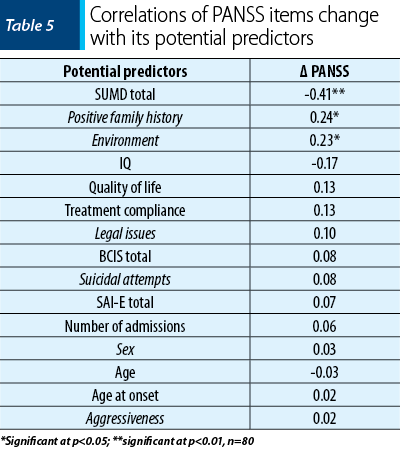
In this sequence of the research, we tested the correlation between baseline PANSS and magnitude of change of this variable. The statistical analysis showed a high correlation (r=0.74), significant for a threshold p<0.01 which means that the initial level of PANSS explained 54% (square of correlation coefficient) of the variance for this variable magnitude of change from admission to discharge. Therefore, in step two, all potential predictors of change correlations with Δ PANSS were tested at the initial level statistical control PANSS (partial correlation). In the next step we analyzed the partial correlation (at baseline – first controlled PANSS) of PANSS symptoms progress with each of its potential predictors. Table 5 shows the results of our analysis.
What can be seen from Table 5 is that the potential predictors of psychotic symptoms change, with significance related to change, appear to be only those measured by the level of insight SUMD scale, presence of family history, and belonging to urban areas. So, as the initial level of insight is higher, there will be an even more substantial improvement of symptoms. Raising the predictive value coefficient to square, we obtain the coefficient of determination corresponding to this predictor. Therefore, the level of insight, as one predictor, with PANSS initially controlled, explained 16% of variance of improving psychotic symptoms during hospitalization. Also, patients from urban areas seem to have a slight tendency towards higher magnitudes of change, as the coefficient of determination indicates that urban membership explained 5% of the variance when symptoms improve. Also, it seems that the family history is positively associated with magnitude of change of symptoms, but the level of this relationship is also reduced.
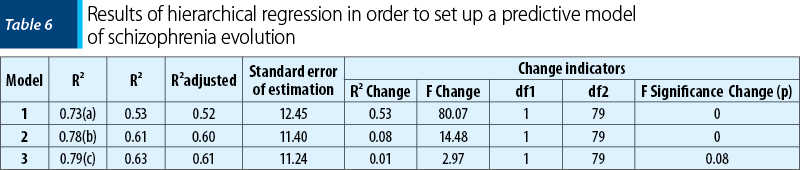
In this sequence, we are interested to identify the optimal predictive model of disease progression, based on available significant correlates of this dynamic. In order to reach this, we used hierarchical regression analysis in which the predictive model introduces all predictors, one by one, in order of correlation with progression of the disease, aiming to identify the model with the fewest predictors but most explanatory value. Table 6 presents the results of hierarchical regression.
From Table 6, we can see that, from initial level of composed model of variables, PANSS and total SUMD explained 60% of variance when disease progression (adjusted R²=0.60), in a statistically significant extent (p<0.01). Adding to this model the “area of residence” variable explained the increase by a further 1% for proportion of variance (R² Change=0.01), but this addition is not statistically significant (F change=2.97; p>0.05). Thus, the best predictive model of disease progression is composed of variables SUMD total and PANSS total on admission.
Discussion
Our study shows that the clinical outcome in schizophrenia is complex and involves many patient-related factors. Our results revealed that the severity of symptoms measured by PANSS explained 54% of the variance for this variable magnitude of change from admission to discharge. Also, both PANSS total and SUMD explained 60% of variance of the disease clinical evolution. From our date knowledge, there is no research in which the PANSS and SUMD scale was used to predict the variance of improving psychotic symptoms during hospitalization. There was a significant improvement in insight measured by SUMD and BCI scales. These results are similar to those found in other research(14). The change in scores on the PANSS scale over the three-week or four-week period predicted the improvement in insight, results supported by several studies(15). Our study showed that only the level of insight measured with the SUMD scale, the positive family history, and the environment (urban area) correlated statistically significantly with the change in psychotic symptomatology. A higher level of insight at admission was associated with a more substantial improvement in symptoms. Our results were in agreement with some previous studies (Mintz et al., 2004(16); Gharabawi et al., 2006(17); Weiler et al., 2000(18); Chen, 1998(19,20)). The limitations of the current study are represented by the research design, in which the prediction of psychotic symptoms and insight was made under the specific hospitalization conditions and psychopharmacological treatment for each patient, each of these being factors that modulate the outcome.
Conclusions
Our findings offer an additional knowledge of using psychometric evaluation to predict clinical outcome in schizophrenia evolution.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
- Charlson FJ, Ferrari AJ, Santomauro DF, et al. Global Epidemiology and Burden of Schizophrenia: Findings from the Global Burden of Disease Study 2016. Schizophr Bull. 2018;44(6):1195-1203.
- Smithnaraseth A, Seeherunwong A, Panitrat R, Tipayamongkholgul M. Hospital and patient factors influencing the health status among patients with schizophrenia, thirty days after hospital discharge: multi-level analysis. BMC Psychiatry. 2020;20(1):592.
- Alem A, Kebede D, Fekadu A, et al. Clinical course and outcome of schizophrenia in a predominantly treatment-naive cohort in rural Ethiopia. Schizophr Bull. 2009;35(3):646-654.
- Davis BJ, Lysaker PH, Salyers MP, Minor KS. The insight paradox in schizophrenia: A meta-analysis of the relationship between clinical insight and quality of life. Schizophrenia Research. 2020;223:9-17.
- Lysaker PH, Weiden PJ, Sun X, O’Sullivan AK, McEvoy JP. Impaired insight in schizophrenia: impact on patient-reported and physician-reported outcome measures in a randomized controlled trial. BMC Psychiatry. 2022;22(1):574.
- Radu M, Ciucă A, Crişan CA, et al. The Relationship between Insight and Psychopathology in First-Episode Schizophrenia. Perspect Psychiatr Care. 2022;58(4):2372-2382.
- Sigrúnarson V, Gråwe RW, Lydersen S, Morken G. Predictors of long term use of psychiatric services of patients with recent-onset schizophrenia: 12 years follow-up. BMC Psychiatry. 2017;17(1):18.
- Kay SR, Fizbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-76.
- Amador XF, Strauss DH. The scale to assess unawareness of mental disorders. Columbia University and New York Psychiatric Institute, 1990.
- Amador XF, Flaum M, Andreasen NC, et al. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry. 1994;51(10):826-836.
- Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM. Assessment of insight in psychosis. Am J Psychiatry. 1993;150(6):873-879.
- Kemp R, David A. Insight and adherence to treatment in psychotic disorders. Br J Hosp Medicine. 1995;54(5):222-227
- Beck AT, Baruch E, Balter JM, Steer RA, Warman DM. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. 2004;68(2-3):319-329.
- Capdevielle D, Norton J, Aouizerate B, et al. Comparison of three scales (BIS, SUMD and BCIS) for measuring insight dimensions and their evolution after one-year of follow-up: Findings from the FACE-SZ Cohort. Psychiatry Res. 2021;303:114044.
- Wiffen BD, Rabinowitz J, Lex A, David AS. Correlates, change and ‘state or trait’ properties of insight in schizophrenia. Schizophr Res. 2010;122(1-3):94-103.
- Mintz AR, Addington J, Addington D. Insight in early psychosis: a 1-year follow-up. Schizophr Res. 2004;67(2-3):213-7.
- Gharabawi GM, Lasser RA, Bossie CA, Zhu Y, Amador X. Insight and its relationship to clinical outcomes in patients with schizophrenia or schizoaffective disorder receiving long-acting risperidone. Int Clin Psychopharmacol. 2006;21(4):233-240.
- Weiler MA, Fleisher MH, McArthur-Campbell D. Insight and symptom change in schizophrenia and other disorders. Schizophr Res. 2000;45(1-2):29-36.
- Chen EY-H. Insight and symptoms of psychosis: a prospective inpatient study. Schzizophr Res. 1998;29:34.
- Mintz AR, Dobson KS, Romney DM. Insight in schizophrenia: a meta-analysis. Schizophr Res. 2003;61(1):75-88.
Articole din ediţiile anterioare
Sindromul depersonalizării și depersonalizarea disociativă
Sindromul de depersonalizare/ derealizare ocupă un loc aparte în psihopatologie. Deşi ocupă un loc central în perturbarea identitară a persoanei, a...