Actualităţi în investigarea prenatală a fătului folosind RMN-ul fetal
Advances in the prenatal investigation of the fetus using MRI
Abstract
Fetal MRI represents a modern tool that can help us better diagnose and evaluate at-risk pregnancies. It comes as an adjuvant to the widespread ultrasound examination, proving its importance in a large number of pathologies. As already known, magnetic resonance imaging (MRI) is an imaging technique that does not use ionizing radiation. This is the most important feature when talking about maternal and fetal imaging. Beside this, it also has a few other advantages: wide field of view, excellent tissue contrast, it is not limited by maternal body fat, osseous structures or fetal presentation. The ability to make multiplanar acquisitions has also proven to be a powerful tool that is not always available with ultrasound. Although there are no contraindications regarding the safety of the mother or fetus, it is recommended that the investigation should not be performed earlier than the second trimester. It is also important to mention that the examination does not provide useful information if it is made too early. In conclusion, as MRI technology is becoming more and more accessible, we expect that fetal imaging will become more widespread in complicated cases. The new advancements will surely prove to be a useful tool in managing at-risk pregnancies.Keywords
fetal MRIcentral nervous systemmalformationposterior fossa pathologyprenatal diagnosispregnancy evaluationRezumat
Rezonanţa magnetică nucleară (RMN) fetală reprezintă o unealtă modernă, care vine în ajutorul stabilirii diagnosticului în sarcinile la risc. Acesta reprezintă o examinare complementară ecografiei, demonstrându-şi astfel importanţa într-un număr mare de patologii. După cum se ştie, RMN-ul este o procedură imagistică neionizantă. Aceasta reprezintă cel mai important aspect atunci când vorbim despre imagistica materno-fetală. RMN-ul mai are şi alte avantaje, precum câmp de explorare mare, contrast tisular bun, cât şi faptul că nu este limitat de obezitatea maternă, de structuri osoase sau de prezentaţia fătului. Un alt avantaj de care ecografia nu beneficiază mereu este capacitatea de a realiza reconstrucţii 3D multiplanare. Chiar dacă nu au fost observate efecte adverse, se recomandă realizarea RMN-ului după trimestrul I. De asemenea, menţionăm şi că o examinare făcută prea precoce nu va aduce informaţii utile. În concluzie, ne aşteptăm ca RMN-ul fetal să devină o examinare din ce în ce mai răspândită odată cu creşterea accesibilităţii populaţiei la această tehnologie. Dezvoltarea continuă a acestei noi tehnici de imagistică va aduce, cu siguranţă, avantaje în gestionarea sarcinii la risc.Cuvinte Cheie
RMN fetalsistem nervos centralmalformaţiepatologie de fosă posterioarădiagnostic prenatalevaluarea sarciniiIntroduction
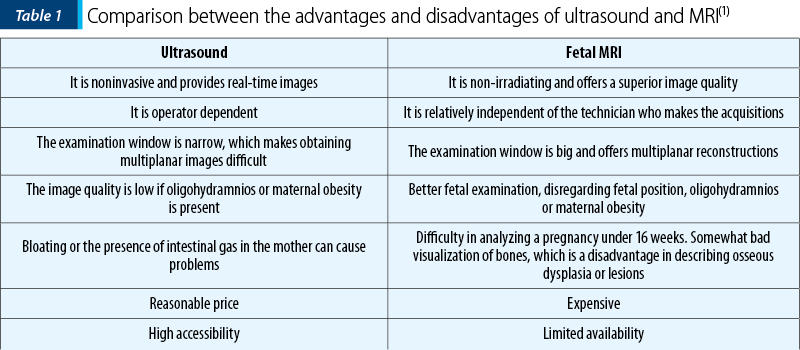
Fetal magnetic resonance imaging (MRI) is a fully developing investigation that provides a plethora of anatomical aspects regarding both the mother and the fetus. Although ultrasound is the most widespread form of pregnancy evaluation, sometimes it is necessary to complement it with something more, namely fetal MRI(1).
MRI is of great help in cases when ultrasound is incapable of fully describing a lesion or anomaly, and it is only used to complement the ultrasound procedure, not replace it. By using fetal MRI, some more obscure pathologies can be better analyzed than just using ultrasound, thus the management and prognosis of each case can be adjusted and optimized(2). The most common cases in which we use fetal MRI are the following: anomalies of the posterior fossa (choroid plexus cysts, agenesis of the corpus callosum), ventriculomegaly, Dandy-Walker syndrome, hiatal hernias, CCAM, pulmonary sequestration, and others(3). The progress brought by these new investigations, that can accurately describe the lesions observed at an ultrasound examination, has increased the quality of the treatment(4). Fetal MRI has seen a great evolution in the past years, making it an efficient and safe way to evaluate multiple parameters of the fetal growth, being especially useful in describing the nervous central system. Ultrasound, although considered the routine examination method, can’t always detect all the neural tube defects(5). MRI can provide a superior analysis of the fetal brain and neural tube compared to the classical ultrasound, being able to detect unobserved ultrasound anomalies(6). This is why the MRI follow-up tends to become an important step in the correct evaluation and monitoring of the pregnancy when the ultrasound examination raises the suspicion of a possible neurologic or neural tube anomaly.
The role of this article is to review the recent data regarding the exploration and management of the pregnancy, so that a collaboration between the obstetrician and the radiologist can be made in the complicated cases that can’t be sufficiently described by the classical ultrasound exploration(7).
Advantages
The main advantage of this investigation is that it does not use ionizing radiation, as it is the case in the conventional X-ray or CT, therefore it doesn’t cause any harm to the developing fetus. It also has a large field of examination and a very high tissue contrast, meaning that the anatomical structures can be better differentiated. The large field of view also allows for 3D multiplanar reconstructions of the region of interest. This allows us to adapt the images based on the fetal position, in this case the presentation of the fetus doesn’t influence the examination(8).
As opposed to conventional ultrasound, the examination is not limited by the maternal obesity, oligohydramnios or by bony parts. The brain can be seen without the interference of the ossification process of the cranium(9). Other fetal structures and systems can also be visualized (lungs, liver, kidneys and intestines)(10). The fact that you can acquire multiplanar images allows the clinician to properly asses the extension and complexity of some lesions in proportion to the whole fetal body, thus increasing the examination accuracy(7). MRI also has an important role in case of in utero interventions, such as spina bifida, or masses that compress the airways(11). It also describes with great accuracy the placenta and other placentar malformations. This can be then correlated with the morphological features of the fetus to assess his health(12). In case of multiple pregnancy, it also brings a new light, providing important information in complicated cases(13).
Recently, MRI has also been used in some post-mortem cases when the necropsy can’t be made(14,15). Of course, the advancements are still being researched, such as MRI spectroscopy.
Short history
The first fetal MRI was performed in 1983. In the 1990s, fetal MRI was revolutionized by the apparition of the fast “single shot” sequences. This offers quality images that can be obtained in less then one second, practically eliminating motion artefacts. Also, the equipment has become more and more accessible, being distributed by both Siemens and General Electrics.
When to use fetal MRI
Ultrasound is at the moment the most widespread method of pregnancy evaluation. There are some instances in which ultrasound is not enough, as such we have to rely on MRI(16). The recommendation towards MRI is made by the gynecologist who is faced with a complicated diagnosis at any gestational age.
The opportune moment to perform
the examination
The age of the pregnancy can affect the quality of the images. Therefore, in the first trimester the examination is difficult due to the small size of the fetus, the increased cases of movement artefacts characteristic for this period and, lastly, because some pathologies aren’t sufficiently developed yet.
After the 17th week, the examination becomes much easier and accurate. The third trimester is the best one for performing an MRI because the organs and systems are completely developed. Also, the fetus is larger now, making the characterization of small lesions easier. In this trimester, there is also a reduced number of motion artefacts(17). The main disadvantage in the third trimester is that the pregnancy is already well developed and some therapeutic procedures can already be obsolete (cervical mases that compress the airways).
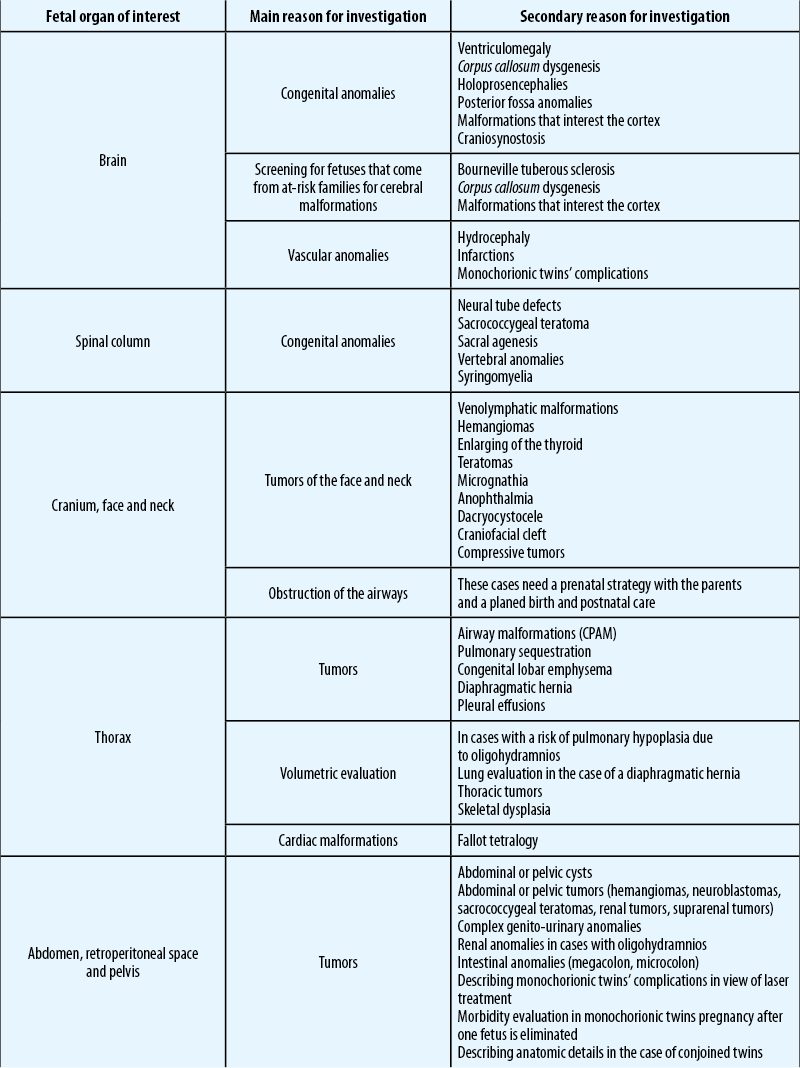
Fetal MRI indications
The MRI procedure is suggested when the ultrasound exploration is difficult to execute from various reasons, or when difficult to describe lesions are identified(18). The International Society of Ultrasound in Obstetrics and Gynecology (ISOUG) has elaborated a good practice guide for when to use fetal MRI(19), which is also in accordance with the guide developed by the American College of Obstetricians and Gynecologists (ACOG)(17).
Fetal MRI indications:
-
Difficulty in realizing a good and correct ultrasound examination
-
Events that occur during the progression of the pregnancy (oligohydramnios, anamnios, polyhydramnios)
-
Confirming or excluding the ultrasound findings
-
Anormal placenta
-
Multiple pregnancy
-
Previous maternal history
-
Previous family history.
Some other indications for the procedure concern the maternal pathologies and are represented by placenta implant anomalies, placenta accreta, percreta or increta, cervix length, oligohydramnios and obesity, the number of umbilical veins, amniotic bridle, umbilical implantation on the placenta and the ratio between the placenta and the cervical canal(16). The width of the exploration field is so big, that it can also describe at the same examination some pathologies pertaining to the mother that are not accessible to the ultrasound, such as uterine fibromas, ovarian cysts and renal related aspects(8). In some cases, fetal MRI may be done as preparation for invasive in utero interventions, such as cervical tumors, spina bifida, meningiomas, teratomas, hiatal hernias and complicated twin pregnancies(6). MRI can also be requested for timely postnatal interventions such as myelomeningocele, or other complex lesions that need immediate intervention(16).
Technique
The technique has seen a massive evolution in the past years. Two decades ago, such an investigation implied maternal and fetal sedation so that the motion artifacts would be reduced. In some cases, the mother would have to hold apnea. At prestent we use a 1.5 Tesla MRI and a plethora of different techniques, so that the procedure can be finished faster and with a good resolution.
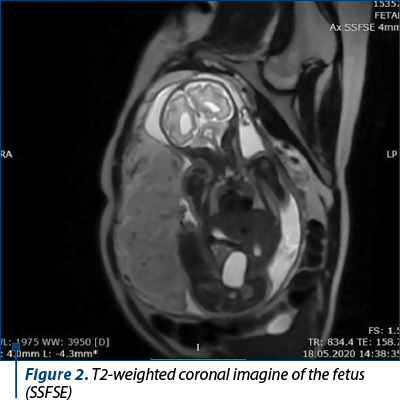
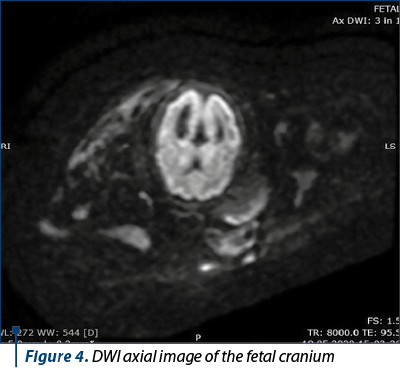
New techniques have been developed so that we can obtain better quality images for anatomical description (SSFSE – single shot fast spin echo), for the lung and vessels (SSFP – steady state free precession), as well as fast acquisition protocols HASTE (half Fourier acquisition single-shot turbo spin-echo), which greatly limit the amount of motion artefacts. These are the most common examination protocols used. Knowing this technical detail is important, so that you can adapt the examination protocol to each patient and pathology (T1-weighted images for describing hemorrhage, calcifications, the liver and thyroid; while T2-weighted images are usually used to describe facio-crancial and cervical anomalies)(20).
The two main methods used to analyze a region are T1- and T2-weighted images, both of which can tell you different things about the region of interest. The weighted images are dependent on some specific relaxation times (spin-spin, spin-matrix), as is also the case for the proton density images(21). We generally use T1-weighted images to describe the anatomical structures, the T2-weighted images being more helpful in describing the pathology. Among the more common types of imaging, we can also use DWI (diffusion weighted images), magnetic resonance spectroscopy and DTI (diffusion tensor imaging).


Recently, new techniques, such as functional MRI (a well-known and already in use protocol for adults), have been adopted in the fetal exploration field, which are of great help in defining lesions that don’t determine morphological changes in the brain. The patient is instructed not to eat for approximately 4 hours beforehand, so that the peristaltic movement of the bowel is at a minimum (thus reducing motion artefacts), and furthermore this reduces the postprandial activity of the fetus(1). Before the procedure, the family is informed about the technique and the possible implications of the findings. The patient is asked to urinate before the examination. He is then laid on his back on the examination table, with his feet pointing inward towards the MRI machine, as to reduce the sensation of claustrophobia(17). The special medication is not needed.
Limits of the method
The most common problem is represented by the motion artefacts. In the majority of cases, the fetus is the one responsible, although in some cases the mother may also move. In some cases, they are so important that the examination must be redone, thus increasing the scan time(16).
Safety
MRI is a noninvasive procedure that doesn’t use ionizing radiation which causes secondary aftereffects on the short or long term(22). As of now, there is no proof that the procedure causes long-term side effects on the fetus. Even so, this is not unanimously accepted. There are arguments supporting both sides.
Some of the possible effects were: audio perception alteration, teratogenic induction, excess tissue heating. All of these problems were considered to come from the examination technique (because of the high noise and the heating of the patient)(23). International institutions, such as US-FDA, ICNIRP and MDA, don’t restrict the investigation, but they advise precaution and correct monitoring of the SAR value (Specific Absorption Rate) of the exposed tissue. The lack of a consensus regarding the safety subject is due to the small lots of patients included in the clinical trials, as well as the difficulty in the long-term following of the patients. The contrast agent gadolinium is not usually used, being only given in the most complicated cases where the gains of the examination far exceed the risks. Even though the experimental data show no side effects, the lack of studies made with human subjects discourages its use. The main problem is related to the elimination of the gadolinium particles. In adults, as well as in the developing fetus, it’s eliminated trough the kidneys. The problem that appears in the case of the fetus is that the gadolinium particles are excreted in the amniotic fluid from where the fetus continues to recycle the particles by swallowing the amniotic fluid. As such, the particles are in contact with the fetus for an extended period of time(4).
Ethic problems
MRI is a noninvasive procedure that doesn’t use ionizing radiation which causes secondary aftereffects on the short or long term. The American Society of Radiology declared that a pregnant woman can benefit from this procedure at any gestational age, as long as the benefits are greater than the risk and when all other investigations that have been made are inconclusive. Even so, it is recommended that the procedure takes place after the 17th-18th week of pregnancy. This is mostly because at this time the fetus has grown a bit in size, making the examination easier, and also because the first trimester is characterized by many fetal movements. An informed statement from the mother is enough to go on with the procedure(24).
Conclusions
Fetal MRI comes as a complementary investigation in cases when the ultrasound diagnosis can’t be made with certainty. The information provided by MRI is highly precise and detailed and thus the therapeutic conduit, the birth planning and even the postpartum care of the fetus and mother can be made early, as to offer the best medical support. The fact that it is an expensive and laborious procedure means that the availability is not that high. Because of this, and due to the fact that the operating physicians’ skills greatly influence the result, it is reserved only for well-equipped medical centers.
An interdisciplinary team is ideal for the maximum benefit of the patients, with different medical specialists, such as radiologist, obstetrician, neonatologist, pediatric neurologist, geneticist, neuroradiologist and others.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Rathee S, Joshi P, Kelker A, Seth N. Fetal MRI: a pictorial essay. Indian J Radiol Imag. 2016;26(1):52-62.
-
Da Silva NA Jr, Vassallo J, Sarian LO, Cognard C, Sevely A. Magnetic resonance imaging of the fetal brain at 3 Tesla. Medicine (Baltimore). 2018;97(40):e12602.
-
The Society for Pediatric Radiology. Fetal MRI. General information. Available at: https://www.pedrad.org/Specialties/Fetal-Imaging/Fetal-MRI-General-Information.
-
Coakley FV, Glenn OA, Qayyum A, Barkovich AJ, Goldstein R, Filly RA. Fetal MRI: developing technique for the developing patients. Am J Roentgenol. 2004;182(1):243-52.
-
Tee LM, Kan EY, Cheung JC, Leung WL. Magnetic resonance imaging of the fetal brain. Hong Kong Med J. 2016;22(3):270-8.
-
Saleem S N. Fetal MRI: An approach to practice: A review. J Adv Res. 2014;5(5):507-23.
-
Tercanli S, Prüfer F. Fetal Neurosonography: ultrasound and Magnetic Resonance Imaging competition. Ultraschall Med. 2016;37(6):555-7.
-
Kosus A, Kosus N, Usluogullan B, Duran M, Turhan NO, Teksam M. Fetal magnetic resonance imaging in obstetric practice. J Turkish-German Gynecol Assoc. 2011;12(1):39-46.
-
Robinson D, Bulas DI, Ashley J. Fetal Magnetic Resonance Imaging - basic technique. In: Bulas DI, Bahado-Singh R, Kline-Fath BM. Fundamental and advanced fetal imaging. Ultrasound and MRI. Philadelphia, Wolters Kluwer Health, 2015.
-
Prayer D. Fetal MRI. Berlin, Springer-Verlag, 2011.
-
Maselli KM, Badillo A. Advances in fetal surgery. Ann Transl Med. 2016;4(20):394.
-
Vegar-Zubovic S, Behmen A, Bektesevic H, Prevljak S, Sefic-Pasic I, Dzananovic A, Bukvic M. Magnetic Resonance Imaging in the diagnosis of fetal pathology. Acta Inform Med. 2019;27(1):50-3.
-
Hubinont C, et al. Anomalies of the placenta and umbilical cord in twin gestations. Am J Obstet Gynecol. 2015;213(4, suppl):91-101.
-
Shelmerdine SC, Hutchinson JC, Arthurs OJ, Sebire NJ. Latest developments in post-mortem foetal imaging. Prenatal Diagnosis. 2020;40(1):28-37.
-
Kang X, Carlin A, Cannie MM, Cos Sanchez T, Jani JC. Fetal postmortem imaging: an overview of current techniques and future perspectives. Am J Obstet Gynecol. 2020;223(4):493-515.
-
Kline-Fath BM, Bulas DI, Bahado-Singh R. Fundamental and advanced fetal imaging. Ultrasound and MRI. Philadelphia, Wolkers Kluwer Health. 2015:4-12.
-
Copel J, et al. Guidelines for diagnostic imaging during pregnancy and lactation. ACOG. Clinical Guidance. 2017:723.
-
Prayer D, Brugger PC, Asenbaum U. Indications for Fetal MRI. [book auth.] Daniela Prayer. Fetal MRI. Springer. 2011:1-16.
-
ISUOG Practice Guidelines: performance of fetal magnetic resonance imaging. Ultrasound Obstet Gynecol. 2017;49:671-80.
-
Şanta A. Imagistică prin rezonanţă magnetică. In: Dudea SM. Radiologie - Imagistică Medicală. Îndrumător de studiu pentru pregătirea în specialitate. Ed Medicală, Bucharest. 2015;1:21-34.
-
Beatu AM, Zaharia C, Popa BV. Noţiuni de radiofizică şi radioprotecţie. In: Iana G, Popa BV, Lupaşcu IG. Radiologie şi imagistică Medicală. Curs pentru studenţi şi medici rezidenţi. Bucharest. Ed. Univ. “Carol Davila”. 2018:13-39.
-
Stecco A, Saponaro A, Carriero A. Patient safety issues in magnetic resonance imaging. Radiol Med. 2007;112(4):491-508.
-
Lubner RJ, Kondamuri NS, Knoll RM, Ward BK, Littlefield PD, Rodgers D, Abdullah KG, Remenschneider AK, Kozin ED. Review of audiovestibular symptoms following exposure to acoustic and electromagnetic energy outside conventional human hearing. Front Neurol. 2020;11:234.
-
Martin C, Darnell A, Escofet C, Duran C, Perez V. Fetal MR in the evaluation of pulmonary and digestive system pathology. Insights Imaging. 2012;3(3):277-93.




