In the case of all types of cancers, it is universally valid that early detection significantly improves the survival rate. In the case of cervical cancer, this statement extends to more advanced forms where the proper treatment is associated with significant disease control. The prevention and control of cervical cancer depend significantly on national policies and implemented guidelines. Also, informing targeted population is a key point of a successful prevention program. There are two key points of a screening program for directing it to success. First, educating health carriers and the general population on the importance of detecting preinvasive lesions and early stages of cancer and, secondly, increasing the accessibility and affordability of a proper medical approach. Our proposal includes a database notification program which identifies and highlights the patients suitable for HPV vaccination and those for cervical cancer screening through cytology. The idea of this program can be adapted and used for any existing database and for any other screening programs.
Analiza rezultatelor programelor naţionale de screening pentru depistarea activă precoce a cancerului de col uterin şi propunere de strategie
Analysis of the results of national screening programs for early active diagnosis of cervical cancer and proposal of improvement strategy
First published: 28 septembrie 2021
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.33.3.2021.5314
Abstract
Rezumat
În cazul tuturor tipurilor de cancer, este universal valabil faptul că detectarea precoce îmbunătăţeşte semnificativ rata de supravieţuire. În cazul cancerului de col uterin, această afirmaţie se extinde la forme mai avansate pentru care tratamentul adecvat este asociat cu un prognostic semnificativ mai bun. Prevenţia şi managementul pacientelor cu cancer de col uterin depind în mod semnificativ de politicile naţionale şi de liniile directoare implementate. De asemenea, informarea populaţiei vizate este baza unui program de prevenţie de succes. Există două puncte-cheie ale unui program de screening pentru ca acesta să fie de succes. În primul rând, educarea responsabililor din sănătate şi a populaţiei generale cu privire la importanţa detectării leziunilor preinvazive şi a diagnosticării stadiilor incipiente de boală şi, în al doilea rând, creşterea accesibilităţii pentru investigaţiile medicale adecvate. Propunerea noastră cuprinde un program de notificare ce include o bază de date care identifică şi evidenţiază pacienţii potriviţi pentru vaccinarea HPV şi, respectiv, pentru screeningul cancerului de col uterin prin citologie. Ideea acestui program poate fi adaptată şi utilizată pentru orice bază de date existentă şi pentru orice alt program de screening.
Introduction
Cervical cancer is one of the few types of cancer for which primary prevention, vaccination and secondary prevention, respectively, screening and treatment of precancerous lesions, are known and possible(1). In the case of all types of cancers, it is universally valid that early detection significantly improves the survival rate. In the case of cervical cancer, this statement extends to more advanced forms where proper treatment is associated with significant disease control. Diagnosed in early stages, cervical cancer associates a five-year survival rate of 92%; in contrary, the diagnosis in the final stages is associated with a five-year survival rate of only 17%(2). With the clear establishment of the etiological agent, namely the infection with high-risk HPV genotypes, the development of the vaccine and the implementation of large-scale screening programs, the expected result was the elimination of cervical cancer from public health problems over generations.
According to World Health Organization (WHO), in 2018 cervical cancer was the fourth most common cancer in women; at that point, an estimated number of 570,000 new cases per year were declared and, in the same year, 311,000 women died due to cervical cancer(3). In the aforementioned context, these are huge numbers. For 2020, The American Cancer Society offers the following estimated numbers: a total of 13,800 new diagnosed cases of invasive cervical cancer and 4290 deaths(4).
The preponderantly involved ages are 35-44 years old, only 20% of cases occurring in women over the age of 65. The development of cancer before 20 years old is exceptional(5).
The great majority – about 80% – of HPV infections are autolimited. The recommended European strategy for an efficient screening implies the cytology testing for 25-35-year-old women and, in the context of a positive result, the HPV testing is recommended. For the 35-64-years-old age group, the primary testing focuses on evidencing the signs of persistent HPV infection(6).
The prevention and control of cervical cancer depend significantly on national policies and implemented guidelines. Also, informing the targeted population is a key point of a successful prevention program. The screening tools, cytology and/or HPV testing should be generally affordable. The primary prevention, respectively vaccination, should be promoted correctly by highlighting the benefits and focused on teenagers (9-14 years old).
In order to stimulate the population to participate, for maintaining a positive functional program, real and positive results should be declared, at regular time intervals, in order to increase the public confidence in the effectiveness of prevention and the screening programs.
The aim of this article is to analyze the results of national screening programs implemented for early detection of preneoplastic lesions and cervical cancer, as in 2020, according to World Health Organization, in Romania cervical cancer had an estimated number of new cases of 3380, representing 7.5% of all diagnosed types of cancer in females of all ages (Figure 1).
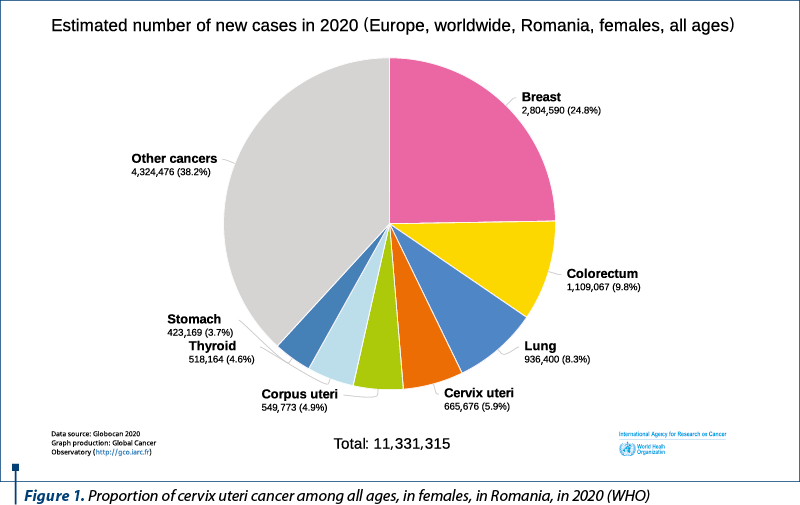
According to the last reported data, Romania ranks first among European countries in terms of incidence (34.9 new cases/100,000 women) and mortality (14.2 deaths/100,000) of cervical cancer, this rate being four times higher than the European mean incidence(7).
Results
The National Screening Program for Cervical Cancer in Romania begun in 2012 and was aimed for a period of five years. The targeted population were the women aged 25-64 years old, including a total of 5.4 million women, Romanian citizens, with or without health insurance, who respected the following criteria:
1. The absence of a confirmed diagnosis of cervical cancer.
2. Asymptomatic.
3. The lack of pathologies in personal medical history suggestive for cervical cancer.
4. Cases with congenital or postsurgical absence of cervix uteri were excluded.
At the national level, the unit responsible for conducting the program was the National Institute of Public Health, along with other nine regional units. The evaluation of the program was performed by the cancer experts from the World Health Organization and the International Agency for Research on Cancer in 2017. The conclusions of the evaluation were that during the program only 10% (611,630 tests) of the targeted population was assessed, and the program did not include a proper follow-up of the patients with positive results, implicitly with the lack of a well-defined process for diagnosis and treatment. From the managerial point of view, the program was characterized by inappropriate monitoring and evaluation(8).
Having these conclusions, the experts made some key recommendations regarding the reintroduction of HPV vaccination in the immunization program and the inclusion of the adequate management of patients with abnormal cytology as a part of the screening program.
There are two key points of a screening program for leading to success: first, educating health carriers and the general population on the importance of detecting preinvasive lesions and early stages of cancer and, secondly, increasing accessibility and affordability of a proper medical approach(9).
Having these data, we propose a strategy for facilitating the selection of patients aged and clinically suitable for primary and secondary screening, respectively vaccination and cytology. Our proposal includes a database notification program which identifies and highlights the patients suitable for HPV vaccination and those for cervical cancer screening through cytology. The idea began from one important deficit of the national screening programs for the early active diagnosis of cervical cancer, which was the lack of information. It is a well-known fact that in Romania the medical staff is insufficient to cover the requirements of a perfectly functional system. Thus, our strategy is based on a simple tool that alerts the physician every time he must access the patients he takes care of. The message is simple: “The following patients must be contacted and informed”, and the software cell corresponding to the investigation recommended is highlighted in a specific color. In order for the program to be functional, it is mandatory to register the personal identification number, based on which the sex of the patient is automatically noted and the age of the patient is calculated. Also, having the contact telephone number of each patient is a must (Figure 2).

The idea of this program can be adapted and used for any existing database and for other screening programs.
Discussion
The European recommendations for cervical cancer screening are represented by Pap smear performed at 21 years old or after the beginning of sexual activity, adapting the period of retesting according to the medical history and previous results. It is considered that a successful cervical cancer screening program can reduce the incidence, the morbidity and the mortality of this pathology with approximately 90%. Precancerous lesions (Table 1, Bethesda system) that precede the progression to cervical cancer are found in approximatively 3.5% of cases. These lesions are treatable with minimally invasive surgical procedures and the regular specialized follow-up of these cases is essential.
According to the Romanian Society of Obstetrics and Gynecology, the latest recommendations regarding the screening for precancerous cervical lesions include, as the first step, the cytology, as it reduces significantly the incidence of cervical cancer and the mortality related to it, and it implies much lower costs compared to HPV cotesting(10).
Furthermore, in order to increase the attention on this topic, we present the summary of three referential cases from our clinical experience.
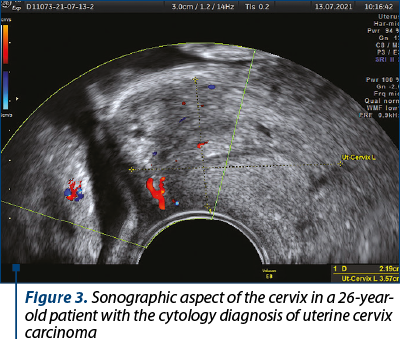
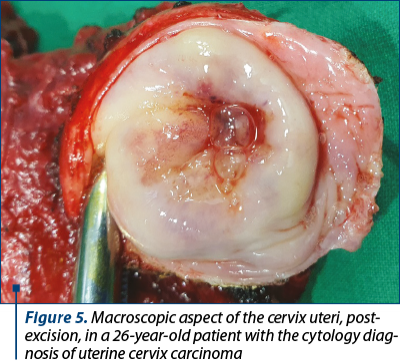
Case 1. A 26-year-old female diagnosed with stage IA2 nonkeratinized microinvasive squamous cell carcinoma of the uterine cervix (Figures 3, 4, 5 and 6).

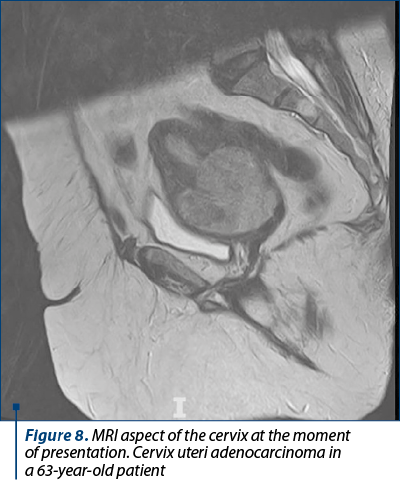
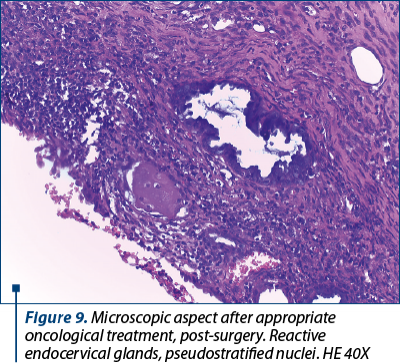
Case 2. A 63-year-old patient diagnosed with stage IIB cervix uteri adenocarcinoma managed through oncological treatment and surgically, with favorable outcome (Figures 7, 8 and 9).

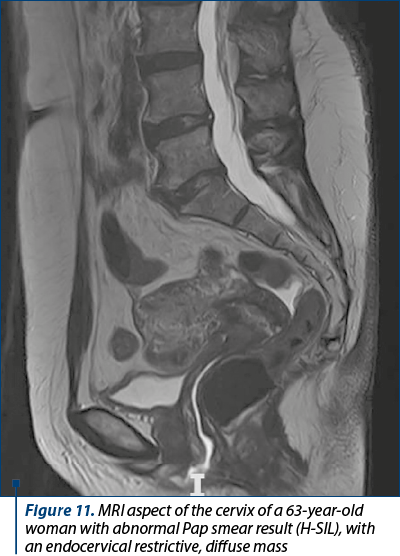
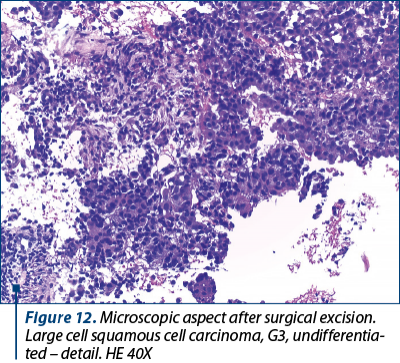
Case 3. A 63-year-old woman with HPV 18 infection, diagnosed with poorly differentiated squamous cell carcinoma of the cervix (Figures 10, 11 and 12).

Conclusions
Only 33% of the targeted population knew about the existence of the Romanian national screening program for the early detection of cervical cancer. Even though the testing was offered for free, only 6.3% of these women had benefited from it.
We consider this, along with Romania’s leading position among European countries in terms of incidence and mortality of cervical cancer, an alarm signal.
Our hope is that the proposed strategy will be a first step in selecting and informing patients regarding the possibility of HPV vaccination and screening for precancerous cervical lesions.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Said Mohammed A, Kabiru A, Mukhtar M, Liman IM, Rabiah AM, Rukayya BM. Perception of cervical cancer and its cytological screening among medical students. Sahel Med J. 2020;23(1):41-6.
- Yang DX, Soulos PR, Davis B, Gross CP, Yu JB. Impact of widespread cervical cancers screening. Am J Clin Oncol. 2018;41(3):289-94.
- https://www.who.int/reproductivehealth/call-to-action-elimination- cervical-cancer/en/
- Fontham E, Andrew PH, Wolf TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. 2020 July 30. Available at: https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21628
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7‐ 30.
- Castanon A, Landy R, Sasieni PD. Is cervical screening preventing adenocarcinoma and adenosquamous carcinoma of the cervix? Int J Cancer. 2016;139(5):1040‐5.
- European Cancer Observatory. 2020. Available at: http://eco.iarc.fr/EUCAN/CancerOne.aspx?Cancer=25&Gender=2
- Group of experts assess prevention and treatment of cervical cancer in Romania. Available at: https://www.euro.who.int/en/health-topics/Life-stages/sexual-and-reproductive-health/news/news/2017/11/group-of-experts-assess-prevention-and-treatment-of-cervical-cancer-in-romania
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012 v1.0. IARC Cancer Base No. 11. Available at: https://publications.iarc.fr/Databases/Iarc-Cancerbases/GLOBOCAN-2012-Estimated-Cancer-Incidence-Mortality-And-Prevalence-Worldwide-In-2012-V1.0-2012
- SROG. Cancerul de col uterin. 2019. Available at: https://sogr.ro/wp-content/uploads/2019/06/27.-Cancerul-de-col-uterin.pdf
Articole din ediţiile anterioare
Actualităţi asupra ghidurilor internaţionale privind screeningul cancerului cervical
Cancerul de col uterin afectează în principal femeile din ţările în curs de dezvoltare, incidenţa şi ratele mortalităţii sale fiind strâns legate d...
Pulsoximetria pentru screeningul nou-născuţilor cu boli congenitale cardiace
Bolile congenitale cardiace sunt cele mai frecvente malformaţii neonatale, iar cele critice, care necesită intervenţie chirurgicală sau cateter...
Carcinom ovarian seros cu grad înalt de malignitate la o femeie tânără - prezentare de caz și revizuirea literaturii de specialitate
Carcinomul ovarian seros cu grad înalt de malignitate este un tip de cancer rar întâlnit la femeile tinere, fiind mai frecvent la femeile în postme...
Screeningul primar în cancerul de col uterin - citologia cervico-vaginală vs detecţia tulpinilor HPV-HR
Cancerul cervical ocupă al treilea loc din totalul cancerelor la femei în întreaga lume, cu peste 500.000 de cazuri noi diagnosticate pe an, facto...