Evaluarea durerii la efectuarea sonohisterosalpingografiei 3D
Pain evaluation during 3D hysterosalpingo-contrast sonography
Abstract
The evaluation of the tubal permeability for the infertile patient is the initial stage in the diagnostic conduct, practiced in the outpatient department, with minimally painful invasive intervention in the absence of the anesthetic support. Thanks to the technological advances of the equipment, as well as the finding of safe and more stable contrast media, the ultrasound procedure with contrast substance, histerosalpingo-contrast sonography (HyCoSy), led to remarkable results in terms of concordance with laparoscopic chromopertubation, exceeding hysterosalpingography in terms of sensitivity and specificity.Keywords
hysterosalpingocontrast sonographypaininfertilitytubal blockageRezumat
Evaluarea permeabilităţii tubare la pacienta infertilă este o etapă iniţială în conduita diagnostică şi care, practicată în ambulatoriu, presupune o intervenţie minim invazivă dureroasă în absenţa suportului anestezic. Graţie progreselor tehnologice ale aparaturii, cât şi găsirii unor medii de contrast sigure şi cât mai stabile, procedura ecografică cu substanţă de contrast, sonohisterosalpingografia (HyCoSy), a condus la obţinerea unor rezultate remarcabile în ceea ce priveşte gradul de concordanţă cu cromopertubaţia laparoscopică, depăşind histerosalpingografia în ceea ce priveşte sensibilitatea şi specificitatea.Cuvinte Cheie
sonohisterosalpingografiedurereinfertilitateobstrucţie tubarăIntroduction
Repeated pelvic inflammatory disease (PID) is considered the main cause of tubal obstruction, the probability of developing infertility being up to 43% after three acute episodes(1). Pelvic inflammatory disease can cause oedema, adhesions, obstruction and dilation of the fallopian tube with fluid. This can impede the normal function of receiving oocytes from the tubal fimbria, which leads to fertility problems. Therefore, in the diagnosis of female infertility, the assessment of tubal permeability is mandatory. To assess tubal permeability, several tests are available, including hysterosalpingography (HSG), laparoscopy with a staining test, fertiloscopy, selective salpingography, and hysterosalpingo-contrast sonography (HyCoSy)(2). HyCoSy is a noninvasive ultrasonographic procedure based on the introduction of a positive contrast fluid which increases the contrast of ultrasound in the uterine cavity and fallopian tubes that can be seen by transvaginal ultrasound. Despite the benefits, HyCoSy is definitely an operator-dependent process. Precise transverse probe movements are essential to identify the passage of fluid through the fallopian tubes during injection(3). In addition, 2D HyCoSy does not provide the image of the fallopian tubes entirely, the potential tubular spasm can be confused with tubal occlusions, and the fluid or airflow through the fallopian tubes can be misinterpreted due to bowel movements. 4D HyCoSy overcomes some of these limitations because it improves the visualization of the movement of the contrast medium in the fallopian tube(4).
Materials and method
From January 2019 to July 2019, a total of 15 infertile patients scheduled for minimally invasive surgery were selected. The inclusion criteria were as follows: proliferative phase of the menstrual cycle (days 5-10), no sexual contact or use of barrier methods during preprocedure, negative vaginal secretion cultures, negative urine culture, absence of vaginal bleeding. The exclusion criteria were: acute salpingitis or pelvic inflammatory disease, ultrasound-visible tubal pathology (hydrosalpinx), suspicious gynecological tumors, previous major surgery in the gynecological field. All ultrasound examinations were performed using GE Medical Systems ultrasound, Voluson E8 Expert ultrasound (equipped with dedicated 3D imaging software and CCI mode) and using a 5-9 MHz transvaginal probe. The detailed ultrasound examination was performed in longitudinal and transverse planes and any uterine, tubal and ovarian abnormalities were observed(5). The contrast medium was a diluted sulphur hexafluoride solution. The statistical analysis was performed to assess the threshold of pain experienced by patients at different times of the ultrasonographic procedure if the fallopian tubes were permeable, obstructed or only one was functional. This was done by determining the numerical value of pain at the time of insertion and fixation of the Foley probe (T1), at the time of injection of the contrast agent (T2) and 30 minutes after the end of the procedure (T3). The analysis was performed later, after confirming the concordance between the results of the ultrasound test with the laparoscopic procedure.
The best known one-dimensional acute pain assessment tools are the visual analog scale (VAS), the numerical rating scale (NRS) and the verbal (four-point) scale (VRS). They work best for the patient’s subjective feeling of pain intensity, and the first two, VAS and NRS, are superior to VRS. The patients were familiar with the use of the numerical instrument before starting the procedure, and the results were recorded and then classified according to the recommendations of Breivik et al. in four categories: 0 = the absence of pain; 1-3 = reduced pain; 4-6 = medium pain; 7-10 = intense pain. The NRS scale is also useful for VAS in the subjective assessment of acute pain, and can be used for up to 24 hours(6). In the initial analysis, we took into account the establishment of the absolute numerical value, as well as the percentage of pain felt by patients at each moment of each procedural time, regardless of the test result, to identify for the studied group the general values of pain felt.
Results
The pain was felt by all patients at different times. At 30 minutes after injection, all patients considered the procedure painless or with mild pain (NRS 0-3) – Table 1.
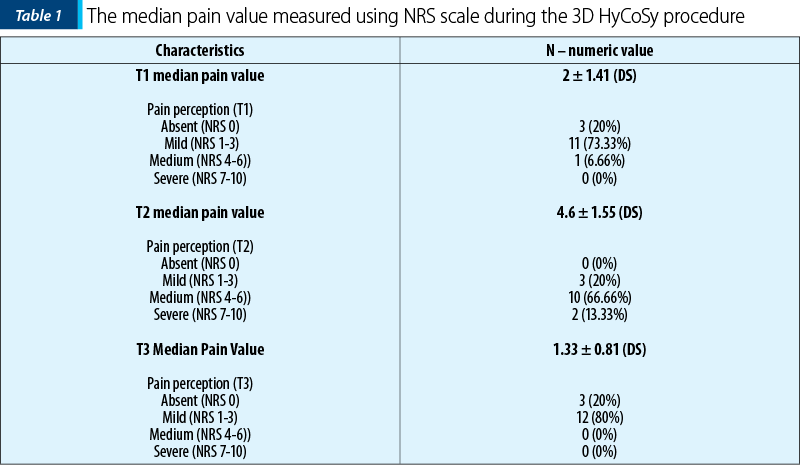
When present, pain was described as uterine, abdominal cramps or menstrual-like pain (dysmenorrhea).
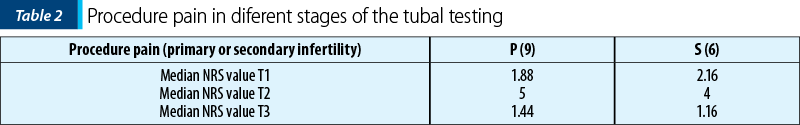
In the second part of the analysis, we divided patients according to secondary or primary infertility status. Thus, nine patients with primary infertility and six patients with secondary infertility were studied.
The conclusions of the obtained results are interesting. The pain felt at the time of T1 is significantly more intense in the group of patients with secondary infertility, which apparently seems peculiar, considering their history. The explanation may take into account the fact that often these patients had to use a Foley pediatric no. 8, compared to the value of 6, which was the size used especially in patients with primary infertility. The baloon was fixed with extra 0.5 ml more serum, in patients who had a history of second-trimester births or abortions to prevent backflow or elimination of the Foley catheter. Subsequently, the recorded values were similar in the two groups, both at the time of injection and at distance (Table 2).
In the last part of the study, we compared the scores obtained according to the patency tubal status, dividing the group into three subgroups: patients in whom both tubes had contrast passage, with a single permeable tube or bilateral tubal obstruction (Table 3 and Table 4).
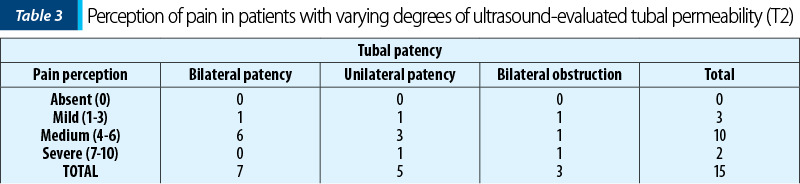
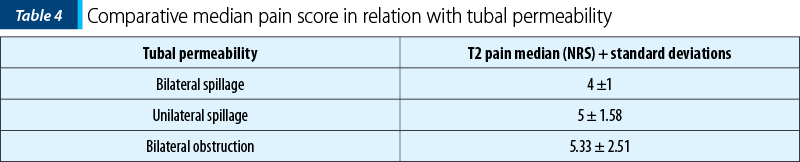
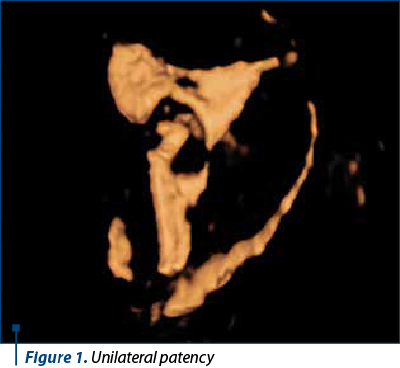
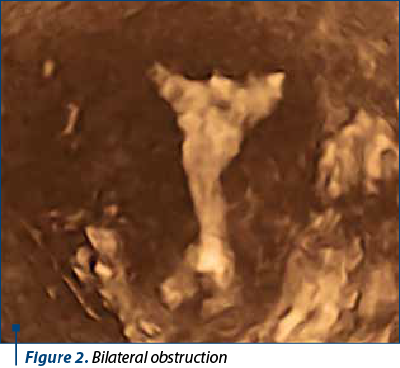
From the demographic and clinical variables assessed, only the impairment of tubal permeability was significantly correlated with the pain felt during injection (T2) measured by the NRS scale. Regarding tubal obstruction, the mean pain scores were 4±1 for bilateral passage, 5±1.58 for unilateral obstruction (Figure 1) and 5.33±2.5 for bilateral obstruction (Figure 2).
It was noted that the most intense pain occurred during the injection of the contrast solution, being mentioned by patients, in general, as of numeric value. This may be due in particular to the need to use an increased volume of solution in the 3D/4D procedure. Fortunately, at T3, 30 minutes after the end of the procedure, the pain was either absent or of low intensity, which confirms the opportunity to perform it in an outpatient setting, without the need for postprocedural medication.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Eschenbach D. Acute pelvic inflammatory disease. Glob Libr Women’s Med. 2008. Available at: https://www.glowm.com/section_view/heading/acute-pelvic-inflammatory-disease/item/29
- Sora-Mărgineanu C, Toader O, Suciu N. Fertiloscopy evaluation of oviduct disease and patency. Proceedings of the 4th Congress of the Romanian Society for Minimally Invasive Surgery in Ginecology and Annual Days of the National Institute for Mother and Child Health “Alessandrescu Rusescu”, Nov 1-3, Bucharest, Filodritto Editore - Proceedings. 2019:567-70.
- Panchal S, Nagori C. Imaging techniques for assessment of tubal status. J Hum Reprod Sci. 2014;7(1):2–12.
- Chen S, Du X, Chen Q, Chen S. Combined real-time three-dimensional hysterosalpingo-contrast sonography with B mode hysterosalpingo-contrast sonography in the evaluation of fallopian tube patency in patients undergoing infertility investigations. Biomed Res Int. 2019; 2019:9408141.
- Exacoustos C, Pizzo A, Lazzeri L, Pietropolli A, Piccione E, Zupi E. Three-dimensional hysterosalpingo contrast sonography with gel foam: Methodology and feasibility to obtain 3-dimensional volumes of tubal shape. J Minim Invasive Gynecol. 2017;24(5):827-32.
- Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Breivik Hals EK, Kvarstein G, Stubhaug A. Assessment of pain. Brit J Anaest. 2008;101(1):17–24.



