Endometrial polyps (EPs) are a common benign gynecologic condition associated with abnormal uterine bleeding (AUB), infertility and recurrent pregnancy loss. Transvaginal ultrasound (TVU) provides an excellent diagnostic technique to identify the size and the anatomic location of endometrial polyps. Its accuracy increases when color Doppler, 3D investigation and saline-infused sonohysterography are used. However, hysteroscopy showed the highest diagnostic accuracy in infertile patients with suspected endometrial polyps and provides a safe and feasible opportunity for EPs removal. Objectives. This study aims to demonstrate the effectiveness of hysteroscopic polyps’ removal in infertile young female patients. Methodology. This study, conducted over a period of one year, included women who addressed our clinic for infertility. These patients were clinically examined and evaluated using transvaginal ultrasound (TVUS). Hysteroscopy was performed on all cases where TVUS raised the suspicion of endometrial polyps. Additionally, the incidence of pregnancies obtained within the first 12 months after the hysteroscopic removal of endometrial polyps was recorded. Results. Out of the cohort of 97 infertile patients, endometrial polyps were suspected in 33 patients. Before hysteroscopy, seven patients additionally underwent a sonohysterography (SHG) procedure. Abnormal uterine bleeding was the primary clinical manifestation (21 cases; 63.63%). EPs were histologically confirmed in 31 cases, and leiomyoma, in two cases. Of the 31 EPs cases, in 20 cases (64.51%) the localization was at the utero-tubal junction. Out of the 30 patients diagnosed with EPs and where the follow-up was possible, 18 individuals, constituting 60% of the group, successfully attained intrauterine pregnancies within the initial 12 months following their hysteroscopic procedure. Conclusions. Our study revealed a significant improvement in reproductive outcomes within the first year following EP resection. The prevalence of endometrial polyps has increased due to improved ultrasound techniques. SHG can potentially increase the ultrasound detection of endometrial polyps, especially in cases where the imagistic information is unclear. Nonetheless, hysteroscopy, known for its high diagnostic accuracy, remains the gold standard. Our research supports the importance of hysteroscopy for uterine cavity assessment and lesion management, and it highlights the increased chances of pregnancy after the lesion’s removal.
Managementul histeroscopic al subfertilităţii în cazurile cu suspiciune de polipi endometriali
Hysteroscopic management of subfertility in cases with suspected endometrial polyps
First published: 29 octombrie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.71.3.2023.9074
Abstract
Rezumat
Polipii endometriali reprezintă o afecţiune ginecologică benignă asociată cu sângerări uterine anormale, infertilitate şi pierderi repetate de sarcină. Ecografia transvaginală este o metodă excelentă pentru diagnosticul şi evaluarea dimensiunii şi localizării polipilor endometriali. Precizia sa creşte atunci când se utilizează tehnici precum Doppler color, evaluarea 3D sau sonohisterografia cu infuzie salină. Totuşi, histeroscopia demonstrează cea mai mare acurateţe în diagnosticul polipilor endometriali la pacientele cu infertilitate şi oferă o metodă sigură şi viabilă pentru rezecţia acestora. Obiective. Acest studiu îşi propune să demonstrez eficacitatea îndepărtării histeroscopice a polipilor endometriali la femeile tinere cu infertilitate. Metodologie. A fost realizat un studiu, pe parcursul unui an, ce a inclus femei care s-au prezentat la o clinică ginecologică pentru infertilitate. Aceste paciente au fost evaluate clinic şi ecografic. Toate pacientele la care ecografia transvaginală a ridicat suspiciunea de polipi endometriali au fost supuse unei examinări histeroscopice. În plus, s-a înregistrat incidenţa sarcinilor obţinute în primele 12 luni după îndepărtarea histeroscopică a polipilor endometriali. Rezultate. Din cohorta de 97 de paciente, la 33 au fost suspectaţi polipi endometriali. La şapte paciente a fost indicată histerosonografia (SHG) cu infuzie de ser fiziologic înainte de histeroscopie. Principala manifestare clinică a fost reprezentată de sângerări uterine anormale (21 de cazuri; 63,63%). Polipii endometriali au fost confirmaţi histologic în 31 de cazuri, iar în celelalte două cazuri au fost diagnosticate leiomioame submucoase. Din cele 31 de cazuri, în 20 (64,51%) localizarea polipilor a fost în proximitatea joncţiunii utero-tubare. Dintre cele 30 de paciente diagnosticate cu polipi endometriali şi la care a fost posibilă evaluarea în dinamică, 18 paciente, reprezentând 60% din totalul grupului, au obţinut sarcini intrauterine în primele 12 luni după rezecţia histeroscopică a polipilor. Concluzii. În studiul nostru, am observat o îmbunătăţire semnificativă a rezultatelor reproductive în primul an după rezecţia polipilor endometriali. Prevalenţa polipilor endometriali a crescut datorită îmbunătăţirii tehnologiilor ecografice. SHG creşte detecţia ecografică a polipilor, în special a formaţiunilor mici, izoecogenice, şi trebuie folosită în cazurile cu informaţii nesatisfăcătoare sau neclare. Cu toate acestea, histeroscopia rămâne standardul de aur pentru evaluarea cavităţii uterine. Datele noastre susţin importanţa histeroscopiei pentru evaluarea cavităţii uterine şi managementul leziunilor intracavitare, evidenţiind şansele sporite de obţinere a unei sarcini după îndepărtarea acestora.
Introduction
Endometrial polyps (EPs) are localized proliferations within the uterine mucosa, comprising endometrial stromal and glandular tissue surrounding a vascular pedicle. The estimated prevalence of uterine polyps is approximately 10% in the general female population(1).
The appearance of EPs can exhibit a high variability regarding their size, which may range from millimeters to centimeters, and their shape, which can be either sessile or pedunculated, as well as their number, which may be solitary or multiple. Furthermore, while their morphology can exhibit diversity, malignant transformation remains infrequent(2).
The clinical manifestations of uterine polyps may range from asymptomatic cases to instances identified during the assessments for abnormal uterine bleeding (AUB) or infertility concerns. AUB represents the most common symptom associated with endometrial polyps, being identified in 20% to 30% of cases involving women with vaginal bleeding(3,4).
The evaluation of the uterine cavity is a fundamental stage in the treatment of female infertility. Even though hysterosalpingography (HSG) and transvaginal sonography (TVUS) are most commonly used for the evaluation of the uterus, the gold standard is represented by hysteroscopy(5-7). The American Society for Reproductive Medicine (ASRM) asserts that hysteroscopy is the definitive method to detect and treat intrauterine disease(8).
Uterine factors account for only 2% to 3% of cases of female infertility, while intrauterine lesions are considerably more prevalent (40% to 50%)(6,7). Notably, larger polyps can occasionally undergo ischemic necrosis at their apex, stemming from intermittent torsion and ensuing thrombosis, potentially leading to the disruption of capillaries beneath them(9).
Endometrial polyps can distort the uterine cavity, resulting in reduced endometrial receptivity and heightened instances of failed pregnancy implantation(10). Such intrauterine lesions exert a detrimental effect on both spontaneous fertility and assisted reproductive pregnancy rates(5). Some studies suggest increased pregnancy rates following the hysteroscopic treatment of intrauterine lesions(4). Larusso et al.(11) proposed that hysteroscopy should be routinely incorporated into infertility assessments due to the high incidence of pathological findings in this context.
Endometrial polyps can hinder embryo implantation within the uterine cavity, not only by occupying space, but also by generating an adverse environment and inflammation(12). Additionally, EPs compromise endometrial receptivity by decreasing mRNA levels of HOXA 10 (Homeobox A10 protein) and HOXA 11 (Homeobox A11 protein), potentially impairing normal embryo implantation(13).
The primary aim of our study was to examine whether transcervical resection of endometrial polyps (TCRP) positively impacts the fertility outcomes and its potential influence on pregnancy rates (PR) among ovulatory infertile women.
Materials and method
This prospective study was conducted in the regional tertiary center of Craiova (Prenatal Unit of the County Emergency University Hospital of Craiova) and Medgin/GinEcho Clinic, Craiova. This study was performed on a one-year period, encompassing a cohort of 97 female participants, aged 20 to 35 years old. The inclusion criteria involved individuals presenting with infertility, with or without abnormal uterine bleeding. All patients underwent a comprehensive TVUS using Voluson E10 and an E8 (GE Medical Systems) ultrasound machine equipped with RIC5-9-D transducers. We also performed sonohisterography in seven cases where the nature of the intrauterine lesion was unclear. In cases where a focal endometrial lesion was confirmed through either color Doppler or saline-enhanced ultrasound assessments, hysteroscopy was deemed necessary. Diagnostic and therapeutic hysteroscopy procedures were conducted for all suspected cases, with meticulous documentation detailing the identified polyps’ localization, size, shape and surface characteristics. Notably, all hysteroscopic interventions were executed under general anesthesia, and the informed consent was obtained from each participant.
The investigation recorded and analyzed the occurrence of pregnancies within the initial 12-month period after the hysteroscopic excision of endometrial polyps.
Results
Out of the cohort comprising 97 patients undergoing ultrasound evaluation for infertility, endometrial polyps were suspected in 33 cases, prompting hysteroscopic evaluation in all patients. Before hysteroscopy, seven patients additionally underwent a sonohysterography procedure.
Among these 33 infertility cases, the primary clinical manifestation predominantly featured AUB (21 cases; 63.63%).
Endometrial polyps were subsequently confirmed in 31 cases through clinical-histological analysis, while in the remaining two cases, a submucous fibroid was identified. Of the 31 confirmed EPs cases, in 20 cases (64.51%) the localization was at the utero-tubal junction; in nine cases (29.03%) there were multiple polyps, and in two cases there were lateral uterine wall polyps (6.45%). In all cases, the size of the polyps was between 1.3 cm and 2.7 cm. It is worth noting that one patient was lost to follow-up. Of the 30 patients with confirmed EPs and where the follow-up was possible, 12 couples had associated conditions related to infertility. Still, the rest of 18 women (representing 60% of the cohort) achieved intrauterine pregnancies within the first 12 months following the hysteroscopic intervention. Notably, three patients experienced a recurrence of endometrial polyps during the first year after pregnancy.
Case report
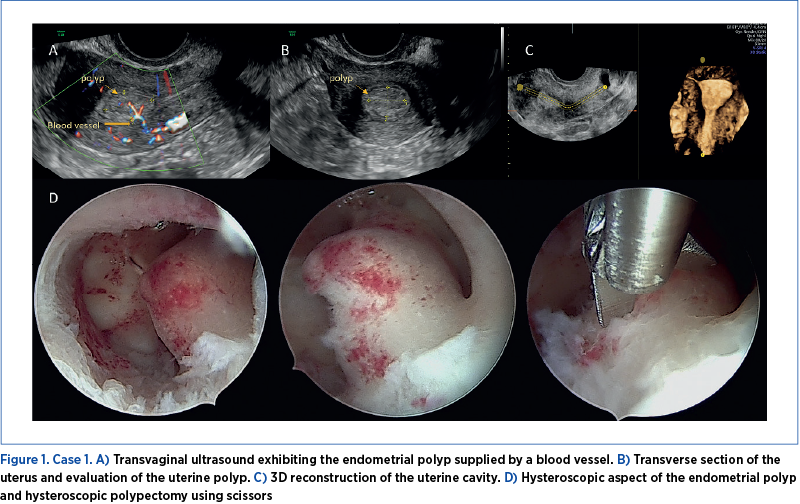
Case 1. A 32-year-old female presented with a medical history marked by sporadic episodes of intermenstrual vaginal bleeding that had persisted for over four months. Concurrently, the patient had been attempting to conceive for approximately seven months. A transvaginal ultrasound examination revealed an abnormally thickened endometrial lining measuring 2.1 cm, with indications suggesting the presence of an endometrial polyp (Figure 1). Both ovaries exhibited normal characteristics, with a corpus luteum image on the left side.
Subsequently, a flexible hysteroscopy was conducted under general anesthesia, confirming the presence of a 1.4-cm endometrial polyp originating from the left lateral uterine wall. The patient then underwent a hysteroscopic resection of the polyp. The duration of the entire procedure, encompassing anesthesia, patient setup and device preparation, was less than 20 minutes. The patient was discharged on the same day. A follow-up examination at three months revealed the absence of further abnormal menstrual or intermenstrual bleeding. The pathological assessment of the excised tissue confirmed the benign nature of the endometrial polyp. The pregnancy was obtained at six months following the hysteroscopic resection procedure.
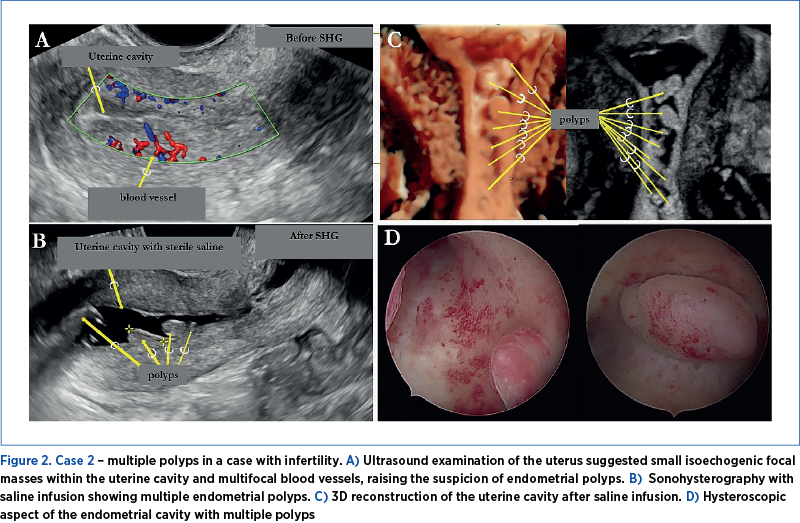
Case 2. A 27-year-old patient presented for a routine gynecological evaluation. She has been attempting to conceive for approximately six months, and she was complaining about menorrhagia. We identified a normal-sized uterus with a homogeneous myometrium during the ultrasound assessment. However, we observed small elongated focal masses within the uterine cavity. Diagnosing endometrial polyps can be challenging through standard ultrasound examination. The combination of transvaginal ultrasound with saline infusion is much more accurate in identifying endometrial polyps. This was our approach during the investigation of this case, which allowed us to observe multiple polyps inside the uterine cavity (Figure 2).
Under general anesthesia, hysteroscopy was performed, which identified the presence of multiple endometrial polyps ranging in size from 0.5 to 1.5 cm (Figure 2). The entire procedure lasted approximately 30 minutes and involved the excision of the polypoid formations. These findings were subsequently confirmed through histopathological examination. The patient’s recovery was uneventful, and she was discharged on the same day. A reevaluation of the patient at ten months confirmed the presence of an intrauterine pregnancy.
Discussion
Extracting endometrial polyps blindly using polyp forceps without a hysteroscope was previously found with a 41% success rate in completely removing the polyp. This method also carries the risk of missing malignant cells at the polyp base(14). Fortunately, all pathological findings in our study confirmed the benign nature of the polyps.
Endometrial polyps represent benign proliferative lesions, often asymptomatic but with the potential to impede a patient’s fertility. Through the use of a hysteroscope, it is obtained a detailed view of the number, structure and vascularization of endometrial polyps(15,16). Additionally, through hysteroscopy, polyps can be removed while allowing for precise control over the resection depth. This approach minimizes the potential harm to the endometrium and facilitates a rapid and uneventful postoperative recovery. Hysteroscopic polypectomy is a cost-effective(17) procedure with a low occurrence of complications and polyps recurrence, making it a technically feasible option for gynecologists, which does not demand extensive training. However, despite its low complication rate, there are still potential complications associated with hysteroscopic polypectomy that should be taken into account. These complications may encompass infection, bleeding, pelvic inflammatory disease, rare instances of uterine tearing, damage to the cervix, as well as issues related to the use of fluids for uterine expansions. In our study, no complications were documented, polypectomies were complete, and the patients were discharged on the same day. The documented incidence of endometrial polyps among infertile women is approximately 32%(18). Our study observed an EP incidence of 31.9%, aligning closely with previously reported studies. AUB emerges as the prevailing clinical presentation linked to the study. The most frequently reported localization of endometrial polyps in the existing literature and in our study is at the utero-tubal junction. Specifically, 64.5% of our cases and 57.4% in the literature exhibited this characteristic pattern.
Numerous studies have reported increased pregnancy rates after the removal of endometrial polyps in infertile women(15). Varasteh et al.(19) observed a pregnancy rate of 78.3% after endometrial polypectomy in subfertile women, Spiewankiewicz et al.(20) documented a pregnancy rate of 76% in the first 12 months post-endometrial polypectomy in infertile women, and Shokeir et al.(21) reported a 50% pregnancy rate following endometrial polypectomy(16,17). While the precise relationship between endometrial polyps and subfertility remains a subject of ongoing debate, our investigation revealed that, among the 30 confirmed cases where the follow-up was possible, 60% achieved pregnancy within the subsequent 12 months following the intervention.
A Cochrane review has emphasized the need for additional well-designed randomized controlled trials (RCTs) to assess the efficacy of hysteroscopic polypectomy in improving reproductive outcomes among subfertile women(22). This aligns with the findings of our study. Furthermore, a systematic review, primarily based on low-quality observational studies, suggested a favorable outcome associated with polypectomy in infertile women(23). However, it is important to note that the evidence supporting endometrial polyp removal is limited, and further research is warranted to comprehensively evaluate this common procedure’s outcomes.
Conclusions
Endometrial polyps are frequently underreported but can provide valuable insights into the biological processes occurring within the uterus. They represent a cause of uterine bleeding, infertility, and may potentially serve as a precursor to malignancy. Consequently, they remain a common condition for individuals seeking medical attention.
In our investigation, we identified a significant enhancement in reproductive outcomes during the initial year following the resection of EPs. The incidence of endometrial polyps has shown an upward trend in recent decades, primarily due to advancements in ultrasound techniques. However, it is noteworthy that hysteroscopy remains the gold standard for diagnosis, boasting high sensitivity and specificity, especially compared to ultrasound’s relatively low specificity. Sonohisterography with saline infusion can potentially increase the ultrasound detection of EPs, especially in cases where the imagistic information is not clear. The clear image of the endometrial contour helps identify small, isoechogenic polypoid formations.
Our study validates the assertions made by previous researchers, reinforcing the continued prominence of hysteroscopy as the preferred and safe method for assessing the uterine cavity and for managing lesions at this anatomical site. Furthermore, our findings emphasize the substantial increase in the likelihood of achieving pregnancy due to removing intrauterine lesions.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
- Clark TJ, Middleton LJ, Cooper NA, et al. A randomised controlled trial of Outpatient versus inpatient Polyp Treatment (OPT) for abnormal uterine bleeding. Health Technol Assess. 2015;19(61):1-194.
- Lieng M, Istre O, Sandvik L, Qvigstad E. Prevalence, 1-year regression rate, and clinical significance of asymptomatic endometrial polyps: cross-sectional study. J Minim Invasive Gynecol. 2009;16(4):465-471.
- Clevenger-Hoeft M, Syrop CH, Stovall DW, Van Voorhis BJ. Sonohysterography in premenopausal women with and without abnormal bleeding. Obstet Gynecol. 1999;94(4):516-520.
- Elfayomy AK, Habib FA, Elkablawy MA. Role of hysteroscopy in the detection of endometrial pathologies in women presenting with postmenopausal bleeding and thickened endometrium [published correction appears in Arch Gynecol Obstet. 2015 Mar;291(3):709. Alkabalawy, Mohamed A [corrected to Elkablawy, Mohamed A]]. Arch Gynecol Obstet. 2012;285(3):839-843.
- Bakour SH, Jones SE, O’Donovan P. Ambulatory hysteroscopy: evidence-based guide to diagnosis and therapy. Best Pract Res Clin Obstet Gynaecol. 2006;20(6):953-975.
- Bosteels J, van Wessel S, Weyers S, et al. Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. Cochrane Database Syst Rev. 2018;12(12):CD009461.
- Taylor E, Gomel V. The uterus and fertility. Fertil Steril. 2008;89(1):1-16.
- Practice Committee of the American Society for Reproductive Medicine. Diagnostic evaluation of the infertile female: a committee opinion. Fertil Steril. 2015;103(6):e44-e50.
- Fritz MA, Speroff L. Clinical Gynecologic Endocrinology and Infertility, Eighth Edition, Lippincott Williams & Wilkins, 2010.
- Salim S, Won H, Nesbitt-Hawes E, Campbell N, Abbott J. Diagnosis and management of endometrial polyps: a critical review of the literature. J Minim Invasive Gynecol. 2011;18(5):569-581.
- Lorusso F, Ceci O, Bettocchi S, et al. Office hysteroscopy in an in vitro fertilization program. Gynecol Endocrinol. 2008;24(8):465-469.
- Richlin SS, Ramachandran S, Shanti A, Murphy AA, Parthasarathy S. Glycodelin levels in uterine flushings and in plasma of patients with leiomyomas and polyps: implications for implantation. Hum Reprod. 2002;17(10):2742-2747.
- Rackow BW, Jorgensen E, Taylor HS. Endometrial polyps affect uterine receptivity. Fertil Steril. 2011;95(8):2690-2692.
- Preutthipan S, Herabutya Y. Hysteroscopic polypectomy in 240 premenopausal and postmenopausal women. Fertil Steril. 2005;83(3):705-9.
- van Dijk MM, van Hanegem N, de Lange ME, Timmermans A. Treatment of women with an endometrial polyp and heavy menstrual bleeding: a levonorgestrel-releasing intrauterine device or hysteroscopic polypectomy. J Minim Invasive Gynecol. 2015;22(7):1153-1162.
- Rubino RJ, Lukes AS. Twelve-month outcomes for patients undergoing hysteroseopic morcellation of uterine polyps and myomas in an office or ambulatory surgical center. J Minim lnvasive Gynecol. 2015;22(2):285-290.
- Kanthi J, Remadevi C, Sumathy S, et al. Clinical study of endometrial polyp and role of diagnostic hysteroscopy and blind avulsion of polyp. J Clin Diagn Res. 2016;10(6):QC01-14.
- Fatemi HM, Kasius JC, Timmermans A, et al. Prevalence of unsuspected uterine cavity abnormalities diagnosed by office hysteroscopy prior to in vitro fertilization. Hum Reprod. 2010;25(8):1959–1965.
- Varasteh NN, Neuwirth RS, Levin B, Keltz MD. Pregnancy rates after hysteroscopic polypectomy and myomectomy in infertile women. Obstet Gynecol. 1999;94(2):168-171.
- Spiewankiewicz B, Stelmachów J, Sawicki W, Cendrowski K, Wypych P, Swiderska K. The effectiveness of hysteroscopic polypectomy in cases of female infertility. Clin Exp Obstet Gynecol. 2003;30(1):23-25.
- Shokeir TA, Shalan HM, El-Shafei MM. Significance of endometrial polyps detected hysteroscopically in eumenorrheic infertile women. J Obstet Gynaecol Res. 2004;30(2):84-89.
- Jayaprakasan K, Polanski L, Sahu B, Thornton JG, Raine-Fenning N. Surgical intervention versus expectant management for endometrial polyps in subfertile women. Cochrane Database Syst Rev. 2014;2014(8):CD009592.
- Lieng M, Istre O, Qvigstad E. Treatment of endometrial polyps: a systematic review. Acta Obstet Gynecol Scand. 2010;89(8):992-1002.
Articole din ediţiile anterioare
Rolul chirurgiei în cazul pacientelor infertile cu adenomioză
Adenomioza este o maladie benignă ce aparţine unui grup de afecţiuni estrogen-dependente, asociate cu unele consecinţe clinice semnificative: disme...
Uterul septat: mini-review util clinicienilor
Septate uterus is more closely associated with infertility, recurrent abortion and obstetrical malpresentations. This pathology raises controversie...
Tratamentul laparoscopic al bolilor pelvine inflamatorii şi implicaţiile infertilităţii
Infecţiile genitale, atât la bărbaţi, cât şi la femei, pot provoca leziuni funcţionale permanente ale aparatului reproductiv, care pot duce la apa...
Tipare de infertilitate. Un studiu de asistenţă medicală primară
Introducere. Infertilitatea reprezintă o problemă medicală şi economică majoră în întreaga lume. Există puţine date referitoare la tiparele cauzelo...