Rezultatele obstetricale şi neonatale ale sarcinilor complicate de infecţia cu SARS-CoV-2
Obstetrical and neonatal outcome of pregnancies complicated with SARS-CoV-2 infection
Abstract
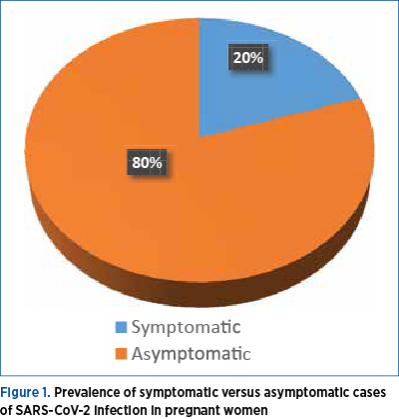
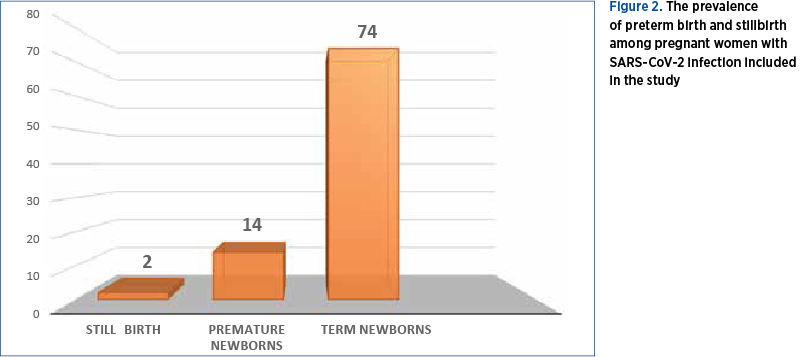
The COVID-19 pandemic has an impact without precedent. Pregnant women are part of the vulnerable population and the extent of SARS-CoV-2 infection consequences on pregnancy outcome and on neonatal prognosis are still studied. It has been speculated, based on what is known about other pathogenic viruses, that SARS-CoV-2 can interfere with placental defense mechanisms and increase the abortion and preterm birth rate. Often, pregnant women infected with SARS-CoV-2 develop mild pneumonia; however, severe pneumonia occurs very rarely and is statistically significantly related to neonatal death. Our study was conducted in a multidisciplinary hospital unit and included 90 pregnant women with SARS-CoV-2 infection, diagnosed through polymerase chain reaction. Data regarding the maternal symptomatology, the gestational age, the way of giving birth, complications that have occurred during birth, the weight at birth and neonatal outcome have been analyzed. No cases of infection with severe clinical impact has been included in the study, only 20% of patients presenting a mild symptomatology. We found an increased rate of preterm birth and intrauterine growth restriction and a high incidence of acute fetal distress followed by caesarean section. SARS-CoV-2 has a chain effects on both the mother and the fetus, as a whole and, subsequently, individually. Our results revealed the adverse obstetrical and neonatal outcome in the prenatal period complicated with SARS-CoV-2 infection, even in asymptomatic and mild-symptomatic cases.Keywords
SARS-CoV-2pregnancyoutcomeRezumat
Pandemia de COVID-19 are un impact fără precedent. Femeile gravide fac parte din populaţia vulnerabilă, iar amploarea consecinţelor infecţiei cu SARS-CoV-2 asupra prognosticului sarcinii şi asupra evoluţiei neonatale este încă studiată. S-a speculat, pe baza a ceea ce se ştie din patofiziologia virală, că SARS-CoV-2 poate interfera cu mecanismele de apărare placentară şi că poate creşte rata de avort şi de naştere prematură. Adesea, femeile însărcinate infectate cu SARS-CoV-2 dezvoltă pneumonie uşoară; pneumonia severă apare foarte rar şi are o legătură semnificativă statistic cu decesul neonatal. Studiul nostru a fost realizat într-o unitate spitalicească multidisciplinară şi a inclus 90 de femei gravide cu infecţie cu SARS-CoV-2, diagnosticate prin reacţia în lanţ a polimerazei. Au fost analizate datele privind simptomatologia maternă, vârsta gestaţională, modul de naştere, complicaţiile apărute în timpul naşterii, greutatea la naştere şi rezultatul neonatal. Nu au fost incluse în studiu cazuri de infecţie cu impact clinic sever, doar 20% dintre paciente prezentând o simptomatologie uşoară. Am constatat, în grupul de studiu, o rată crescută de naşteri premature şi de restricţie de creştere intrauterină, dar şi o incidenţă ridicată a suferinţei fetale acute urmate de cezariană. SARS-CoV-2 afectează în lanţ mama şi fătul, atât în ansamblu, cât şi individual, ulterior. Rezultatele noastre au arătat ca prognosticul obstetrical şi neonatal este influenţat de infecţia maternă în perioada prenatală, chiar şi în cazurile asimptomatice sau cu simptomatologie medie.Cuvinte Cheie
SARS-CoV-2sarcinăprognosticIntroduction
COVID-19 pandemic has an impact without precedent. Until now, more than 240 million of confirmed cases and about five million deaths related to SARS-CoV-2 infection have been registered. In Romania, until the end of September 2021, more than 1.2 million cases have been confirmed, with an associated overall mortality rate of 3%(1). However, these significant numbers have not offered clear answers regarding the differences of the infection’s mechanisms, the course the disease follows, the associated complications and the outcome.
Pregnant women are part of the vulnerable population group and the extent of SARS-CoV-2 infection consequences on pregnancy outcome and on neonatal prognosis are still studied. It has been speculated, based on what is known about other pathogenic viruses, that SARS-CoV-2 can interfere with placental defense mechanisms and increase the abortion and preterm birth rate(2).
Regarding the physiopathology of SARS-CoV-2 infection, from the immunological point of view, a decrease in the number of lymphocytes and monocytes with macrophages infiltration at the level of lung lesions are predominant. Also, respiratory failure is a typical clinical manifestation in severe cases, along with hypercoagulability, thrombosis and, later, multiple organ failure. There is a predisposition to severe forms of the disease as mother’s body undergoes a series of physiological changes in order to sustain and support the growth of the fetus; there is an increased number of decidual natural killer cells, predominant in the first trimester, having a role in regulating the trophoblast invasion and arterial remodeling(3). Macrophages are involved in a series of essential functions in the early pregnancy, such as immunomodulation, blood vessels remodeling and trophoblast invasion, along with the prevention of the rejection phenomena through the production of prostaglandin E2, interleukin 10 (IL-10) and indolamine 2,3-dioxygenase(4).
Cytokines, neurotrophins and chemokines are immune mediators with a crucial role in central nervous system development. If the balance of physiological mechanisms is disrupted, this will be translated in impaired neurodevelopment, cognitive and intellectual abilities and in a high risk of psychiatric disorders(5).
Given the above, it is clear that the changes which occur in women during pregnancy turn them into a segment of population with a high risk of SARS-CoV-2 infection. The cytokine storm interferes with the immunological pregnancy state and can have consequences for the mother and for her unborn child. Data until now have shown that the most common symptoms in COVID-19 pregnant women are fever, cough, lymphopenia, increased levels of C-reactive protein and neutrophil count and increased levels of alanine aminotransferase (ALT). Often, pregnant women infected with SARS-CoV-2 develop mild pneumonia; however, severe pneumonia occurs very rarely and is statistically significantly related to neonatal death(6). The placental histopathological examination has shown that SARS-CoV-2 infection in pregnancy is related to an acute placental inflammation, the presence of the infection at the fetal-placental level and with a reduced level of vertical transmission of antibodies(7).
The microbiota from the maternal-placental interface is affected by the viral infections in the sense that it decreases the level of beta-interferon secretion which plays a key role in fetal receptivity. Thus, the SARS-COV-2 infection, by initiating the described inflammatory response, increases the risk of preterm birth.
Materials and method
Our study has been conducted in a multidisciplinary hospital unit, the Bucharest University Emergency Hospital, during the COVID-19 pandemic (1.03.2020 – 30.09.2021), having the hospital’s ethical committee approval (22276/21.06.2021). In this retrospective study, 90 pregnant women with SARS-CoV-2 infection, who were diagnosed through polymerase chain reaction (PCR) test at admission, were included. The second inclusion criterion was the birth during admission. Data regarding the maternal symptomatology, the gestational age, the way to give birth, the complications that occurred during childbirth, the weight at birth and the neonatal outcome have been analyzed.
Results
During the studied period, in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital, 90 women with SARS-CoV-2 infection gave birth. Most of them were asymptomatic; 20% of symptomatic cases had a mild clinical symptomatology. There were no cases of infection with severe clinical impact to be included in the study (Figure 1).
The incidence of preterm birth in our study group was 15.5% (14 cases) and the rate of stillbirth was 2.2%, respectively two cases (Figure 2); the majority of pregnant women with SARS-CoV-2 infection have delivered at term.
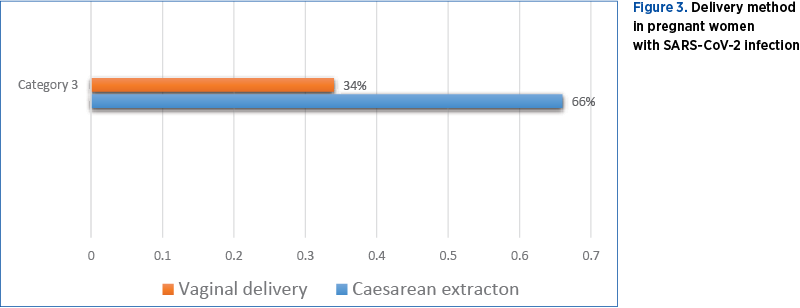
The preferred way of delivery was through caesarean section, with a percentage twice as high (Figure 3).
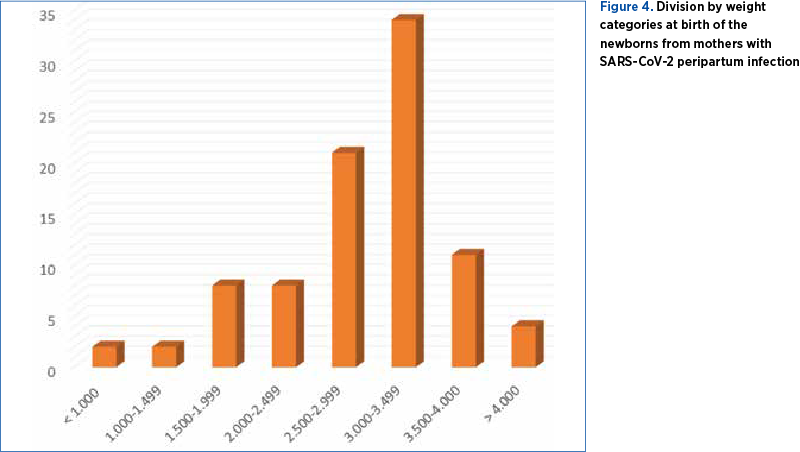
Regarding the birth weight, more than 22% of the newborns of mothers with peripartum SARS-CoV-2 infection have shown intrauterine growth restriction, having a birth weight below 2500 grams (Figure 4).
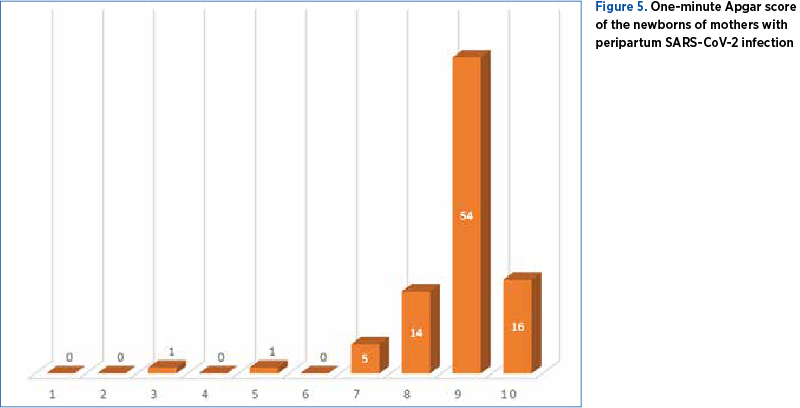
By analyzing the immediate neonatal outcome, only two cases from our studied group had a difficult postnatal adaptation (Apgar score below 7), but with subsequent favorable outcome (Figure 5).
Discussion and conclusions
The studies conducted until now show that, due to the physiological, anatomical and immunological pregnancy-related changes, pregnant women have an increased risk of developing a severe form of COVID-19(8). In our study, only 20% of women were symptomatic, with mild symptoms, but for every positive case the monitoring and treatment protocols have been respected.
One possible explanation for the lack of pneumonia cases in our study group could be the fact that, during the third trimester, the prenatal medical visits are frequent, the general status and the symptomatology are being monitored, and paraclinical evaluation takes place, when a specific management is initiated, if any suspicion of viral infection comes out.
Secondly, it is worth mentioning the higher incidence of preterm birth compared to the general population (approximately 10%). Data published on this topic agree on the fact that the severe infection associates a higher risk of preterm birth, which is insignificant in asymptomatic and mild forms of COVID-19(9). However, the results are controversial, as they vary from one study to another, with a small number of participants and being impossible to exclude other risk factors.
In our case, when comparing with data corresponded to pre-pandemic years, respectively 2016-2019, there is clearly an increase in the incidence of preterm birth, for that period the calculated incidence being 10%(10).
Another interesting fact we have noticed is the high incidence of intrauterine growth restriction. The mechanism of fetal growth restriction is regarded as multifactorial, resulting from a combination of maternal, placental and fetal factors, the uteroplacental insufficiency being the dominant cause. Several maternal nonpathological factors can be reflected in an increased risk of fetal growth restriction, such as height, pregnancy weight, parity and ethnicity(11). SARS-CoV-2 infection is an acute event with a proven negative placental effect, leading to severe hypoxemia.
The functional receptor for SARS-CoV-2 is angiotensin converting enzyme 2 (ACE2), that is mainly expressed in cardiovascular, respiratory and digestive systems. Any changes in maternal homeostasis will affect the fetal growth.
Since the beginning of the pandemic, the anatomopathological analysis of placentas has confirmed that the inflammatory reaction is extended not only to the placental site, but also to the fetus, causing fetal distress, preterm birth, abortion or other unfavorable outcomes. Our results show that, even in asymptomatic pregnant SARS-CoV-2-positive women, there is an increased risk of fetal distress, as in 66% of cases an emergency caesarean section has been performed due to acute fetal distress objectified through a low biophysical score (Figure 3).
In conclusion, SARS-CoV-2 has a chain effect on both the mother and the fetus as a whole and individually. Our results showed the adverse obstetrical and neonatal outcome in prenatal period complicated with SARS-CoV-2 infection, even in asymptomatic and mild-symptomatic cases. A prompt and safe action from the first moment of suspicion or confirmation of the infection is essential for improving the prognosis.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
https://datelazi.ro/
-
Mubarak A, Alturaiki W, Hemida MG. Middle east respiratory syndrome coronavirus (MERS-CoV): infection, immunological response, and vaccine development. J Immunol Res. 2019;6491738.
-
Smith SD, Dunk CE, Aplin JD, Harris LK, Jones RL. Evidence for immune cell involvement in decidual spiral arteriole remodeling in early human pregnancy. Am J Pathol. 2009;174(5):1959.
-
Renaud SJ, Graham CH. The role of macrophages in utero-placental interactions during normal and pathological pregnancy. Immunol Invest. 2008;37(5):535.
-
Schepanski S, Buss C, Hanganu-Opatz IL, Arck PC. Prenatal immune and endocrine modulators of offspring’s brain development and cognitive functions later in life. Front Immunol. 2018; 9:2186.
-
Yan J, Guo J, Fan C, Juan J, Yu X, Li J, et al. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. 2020;223(1):111.e1–4.
-
Sherer ML, Lei J, Creisher P, Jang M, Reddy R, Voegtline K, et al. Dysregulated immunity in SARS-CoV-2 infected pregnant women. medRxiv. 2020 Nov 16;2020.11.13.20231373. doi: 10.1101/2020.11.13.20231373.
-
Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, et al. Maternal death due to COVID-19. Am J Obstet Gynecol. 2020;223(1):109.e1–109.e16.
-
Cosma S, Carosso AR, Cusato J, Borella F, Carosso M, Gervasoni F, et al. Preterm birth is not associated with asymptomatic/mild SARS-CoV-2 infection per se: Pre-pregnancy state is what matters. PLoS One. 2021;16(8):e0254875.
-
Ţurcan N, Bohîlţea RE, Ioniţă‑Radu F, Furtunescu F, Navolan D, Berceanu C, Nemescu D, Cîrstoiu MM. Unfavorable influence of prematurity on the neonatal prognostic of small for gestational age fetuses. Exp Ther Med. 2020;20:2415-2422.
-
Gardosi J. New definition of small for gestational age based on fetal growth potential. Horm Res. 2006; 65 Suppl 3:15-8.





