Vaginal bleeding in the first trimester is a common occurrence, but the majority of the pregnancies have a normal outcome. The careful assessment is yet important, given the possibility of complications. The patients with a threatened abortion should be monitored for progression to pregnancy failure. The most common type of spontaneous abortion is early pregnancy loss, defined as death of an embryo or fetus within the first 13 weeks of pregnancy. The clinical manifestations have low specificity, neither the duration of bleeding, nor the presence of lower abdominal cramping in the first trimester being reliable indicators of pregnancy outcome, thus the special attention has turned to ultrasonography for the evaluation of early pregnancy complications. The therapeutic approach (expectant management, medication or surgical interventions) should be tailored based on the gestational age, clinical and ultrasound findings. Severe hemorrhage requires urgent treatment, the surgical evacuation of the products of conception being often necessary. In this paper, we present the incidence and prevalence of early pregnancy loss and threat of abortion in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital, for a two-year period, discussing the impact of the advanced maternal age as a risk factor for spontaneous abortion.
Studiu retrospectiv privind avortul precoce, efectuat în cadrul Departamentului de obstetrică şi ginecologie al Spitalului Universitar de Urgenţă Bucureşti
A retrospective study regarding early pregnancy loss in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital
First published: 23 decembrie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.68.4.2020.4030
Abstract
Rezumat
Sângerarea vaginală în primul trimestru de sarcină este frecvent întâlnită, dar majoritatea sarcinilor au o evoluţie normală. Evaluarea atentă este totuşi importantă, având în vedere posibilitatea complicaţiilor. Cazurile diagnosticate ca ameninţări de avort pot avea ca rezultat oprirea în evoluţie a sarcinii. Cel mai comun tip de avort spontan este avortul precoce, definit ca decesul produsului de concepţie survenit în primele 13 săptămâni de sarcină. Manifestările clinice sunt nespecifice, sângerarea vaginală sau durerile abdominale apărute în primul trimestru nefiind indicatori fiabili ai evoluţiei sarcinii. În acest context, examinarea ultrasonografică joacă un rol esenţial în evaluarea complicaţiilor sarcinii incipiente. Abordarea terapeutică (expectativă, tratament medicamentos sau tratament chirurgical) trebuie adaptată în funcţie de vârsta gestaţională şi de constatările clinice şi ecografice. Hemoragia severă necesită tratament urgent, evacuarea chirurgicală a produselor de concepţie fiind adesea necesară. În această lucrare, prezentăm incidenţa şi prevalenţa pierderii precoce a sarcinii şi ameninţarea de avort în cadrul Departamentului de obstetrică şi ginecologie al Spitalului Universitar de Urgenţă din Bucureşti, pe o perioadă de doi ani, discutând impactul vârstei materne avansate ca factor de risc pentru avortul spontan.
Introduction
Abortion is the termination of pregnancy before 20 weeks of gestation(1). Spontaneous abortion or miscarriage is a naturally occurring event, unlike induced medical or surgical abortions(1). It is difficult to properly estimate the incidence of spontaneous abortion, as many miscarriages are mistaken as heavy, late menses before clinically recognized pregnancy, but the total incidence is as high as 31%(1).
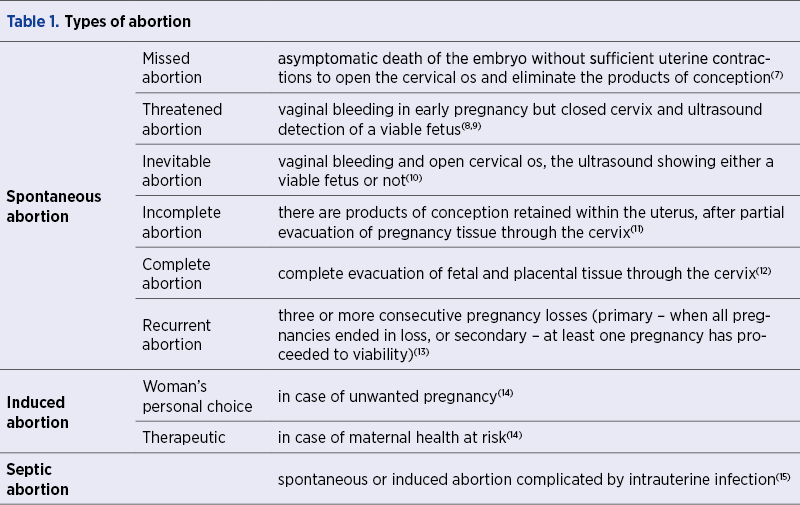
Most spontaneous abortions occur during the first trimester of pregnancy and, although there is no consensus over the terminology for nonviable pregnancies, usually the term “early pregnancy loss” (EPL) refers to such nonviable intrauterine pregnancy within 12+6/7 days of gestation, including the anembryonic pregnancies(1). There are several subtypes of spontaneous abortion based on clinical and ultrasound findings (Table 1), including missed, threatened, inevitable, incomplete and complete abortion.
Regarding the etiology of early pregnancy loss, the exact mechanisms involved cannot always be specified. In about half of the cases, chromosomal abnormalities are a direct cause(2).
Other etiologies refer to maternal infections, uterine anomalies, coagulation and immunological disorders, chronic diseases, unhealthy lifestyle (alcohol or heavy caffeine use, cigarette smoking), and extreme weight. Advanced maternal age and prior pregnancy loss are important risk factor(3).
The most common signs of EPL are vaginal bleeding and pelvic cramping in patients with positive pregnancy test or abnormal menstrual cycle. Given the nonspecific clinical manifestations, transvaginal or transabdominal ultrasound and quantitative human chorionic gonadotropin (hCG) levels are important diagnostic tools(3). The physical examination has limitations as the uterine size and patient’s estimated gestational age can be misleading. A visibly dilated cervix and conception products at the os are suggestive signs, but the cervix can appear dilated in parous women even in the case of a viable pregnancy. On the contrary, a closed cervix and no active bleeding does not rule out EPL(4). The combination of ultrasound scan and serial hCG measurements is considered the optimal evaluation strategy(5). Transvaginal ultrasound criteria for the diagnosis or just suspicious of pregnancy loss are well established and widespread used(6).
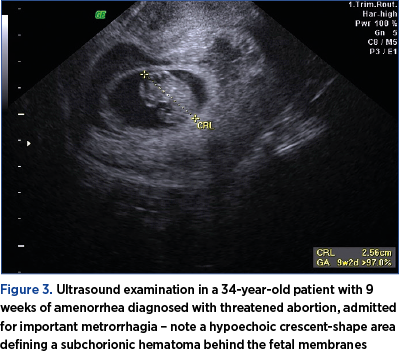
Threatened abortion is defined, according to World Health Organization, as pregnancy-related bloody vaginal discharge or frank bleeding during the first 20 weeks of pregnancy without cervical dilatation. About 10% of the cases are caused by subchorionic hemorrhage and subchorionic hematoma, which increase the risk of pregnancy loss (if the hematoma accounts for 25% or more of the volume of the gestational sac, it is located retroplacental versus marginal(16), if is identified earlier(17)).
In this paper, we present the incidence and prevalence of early pregnancy loss and threat of abortion in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital, for a two-year period.
Materials and method
We retrospectively evaluated the cases admitted in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital between the 1st of January 2018 and the 31st of October 2020 with diagnosis of abortion (according to International Statistical Classification of Diseases and Related Health Problems 10th revision; search by ICD-10 codes O02.1; O03, O04 and O05 with subdivisions 0-9), in order to analyze the rate of early pregnancy loss. The ectopic and molar pregnancies were not included. Another incidence analyzed rate refers to the threat of abortion (ICD-10 code O20.0).
The diagnosis for the patients included in the study was based on clinical examination and on transvaginal/abdominal ultrasound. Serial quantitative hCG measurements were included into the approach to care for the patients presenting with a pregnancy of unknown location.
The informed consent was obtained from each patient and the statistical analysis was performed using Microsoft Excel and SPSS 9.5.
Results
Between the 1st of January 2018 and the 31st of October 2020, 1849 patients were admitted in the Department of Obstetrics and Gynecology of the Bucharest University Emergency Hospital for abortion or threat of abortion. The average age of the patients was 30.5 years old, the average weight was 68.2 kg, the average height was 163 cm, and the average Body Mass Index was 24.3.
Among these patients, 1155 women were hospitalized for threat of abortion or inevitable abortion, out of which 47.01% were pregnancies under 14 weeks of gestation (exemplified in Figure 3 and Figure 6). Our records identified 2.6% of all cases in this category eventually ending in early pregnancy loss despite treatment.

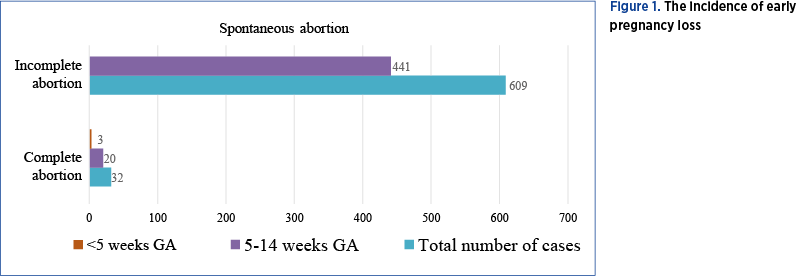
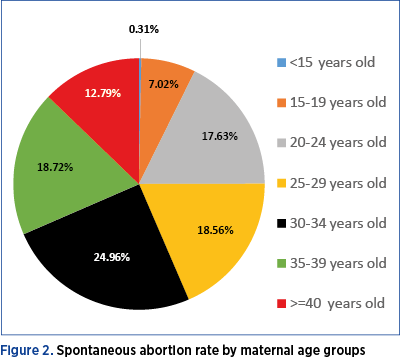
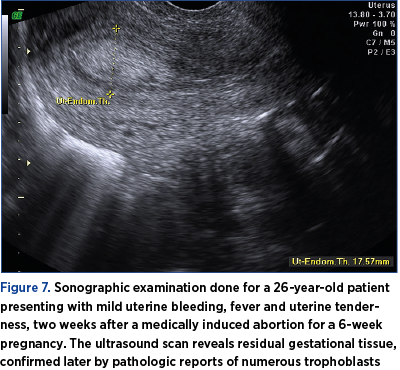
We also identified 641 cases of spontaneous abortion, 71.91% of them occurring in the first trimester (Figure 1). The most common type of spontaneous abortion in our clinic is incomplete abortions (95%) – exemplified in Figure 7. Usually, the complete evacuation of gestational tissue does not require further surgical or medical intervention, unless complications occur. Thus, we had only 32 patients with complete abortion, hospitalized for urgent treatment of complications, such as hemodynamic instability due to heavy bleeding, or severe anemia. The mean maternal age among women with spontaneous abortion was 30 years old, range: 13-48, with 31.51% of miscarriages happening in women over 35 years old (Figure 2). Sixteen patients experienced two spontaneous abortions during the selected period.
In the study interval, 53 medical, therapeutic abortions were performed in our clinic and only 40% of them addressed pregnancies less than 14 weeks.
There were two cases of septic abortion, both after surgically induced abortion in a different medical center, and no cases of EPL complicated by embolism in the selected period.
Discussion
The evaluation of early pregnancy loss might be problematic since ICD-10 available codes for this category are not easily aligned with the clinically relevant EPL types in use. For instance, threat of abortion and inevitable abortion are reunited under the same code. Furthermore, the code for the first trimester includes pregnancy duration up to 13 weeks and 6 days.
First-trimester bleeding in a pregnant woman has an extensive differential diagnosis. Apart from spontaneous abortion, it can be caused by ectopic pregnancy, hydatidiform mole, subchorionic hemorrhage (Figure 3), cervical pathology, infection of the vagina or cervix, vaginal trauma or idiopathic bleeding in a viable pregnancy(18).
It is estimated that approximately 20% of pregnant women will have some bleeding before 20 weeks of gestation, and roughly one half of these pregnancies will end in spontaneous abortion(19). Despite the great number of threat of abortions in our study, we found that 2.6% of them returned to our clinic for EPL (exemplified in Figure 4).
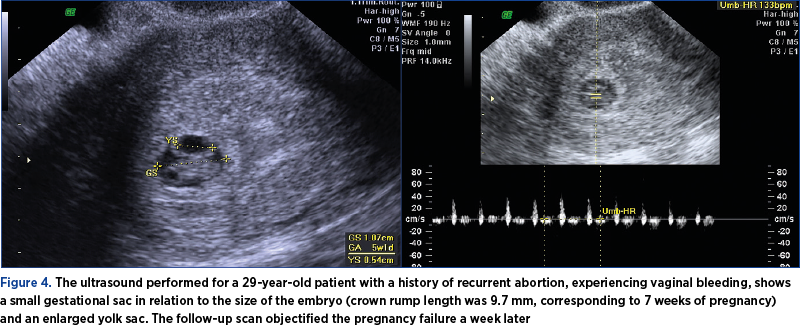
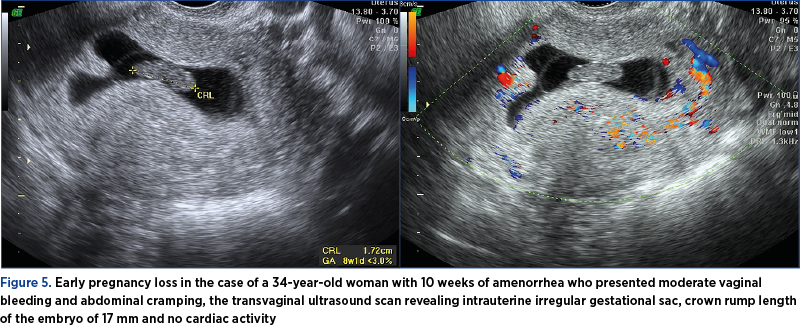
Pregnancy loss is most common in the first trimester and our study revealed about 72 percent of the spontaneous abortions occurring before 14 weeks of gestation (exemplified in Figure 5). The risk of miscarriage varies with maternal age, and there is a strong association between increased maternal age and fetal chromosomal abnormalities(2). In our study, most patients admitted for spontaneous abortion were aged between 30 and 34 years old. In a national prospective cohort study in the Norwegian population, in which 421,000 pregnancies were included, the risk of miscarriage (after excluding induced abortions) was the lowest in women aged between 25 and 29 years old (10%), and rose rapidly after the age of 30, reaching 53% in women aged 45 years old and over(20).
The clinical evaluation can show cervical dilatation and intracervical conception products, being diagnostic for inevitable abortion (exemplified in Figure 6), but ultrasonography is more reliable for distinguishing between complete and incomplete abortion, with 100% sensitivity and 80% specificity for finding products of conception(21).
Although most cases of EPL have mild clinical manifestations, the complications such as severe hemorrhage or infection require a prompt treatment(18). The main reason for hospitalization of patients addressing to our emergency room was moderate or heavy vaginal bleeding, with only two cases of septic abortion.
In case of hemorrhage, severe anemia, cardiovascular disease, bleeding disorders, hemodynamic instability or signs of infection, the surgical evacuation through sharp or suction curettage is the preferred treatment option of early pregnancy loss(22). While the success rates for surgical evacuation reach 99%(23), the risk of complications among the treatment options (expectant, medical or surgical) remains low and is equivocal in women without comorbid conditions or contraindications to one form or another. The patients admitted to our clinic usually required surgical treatment due to severe symptomatology, and had good outcome after treatment.
Conclusions
Vaginal bleeding is a common first-trimester complication and in our clinic we had more than 1000 cases of threat of abortion during the two-year study period. Among the cases of spontaneous abortion requiring hospitalization, incomplete abortions were the most frequent. Ultrasonography plays a crucial role in the evaluation of early pregnancy loss for a highly certain diagnosis.
Bibliografie
-
1. Wilcox AJ, Weinberg CR, O’Connor JF, Baird DD, Schlatterer JP, Canfield RE, et al. Incidence of Early Loss of Pregnancy. N Engl J Med. 1988 Jul 28;319(4):189-94.
-
2. Levy B, Sigurjonsson S, Pettersen B, Maisenbacher MK, Hall MP, Demko Z, et al. Genomic imbalance in products of conception: Single-nucleotide polymorphism chromosomal microarray analysis. Obstet Gynecol. 2014 Aug;124(2 Pt 1):202-9.
-
3. ACOG Practice bulletin no. 200: Early pregnancy loss. Obstetrics and Gynecology. 2018 Nov;132(5):e197-e207.
-
4. Wieringa-De Waard M, Bonsel GJ, Ankum WM, Vos J, Bindels PJE. Threatened miscarriage in general practice: Diagnostic value of history taking and physical examination. Br J Gen Pract. 2002 Oct;52(483):825–829.
-
5. Butts SF, Guo W, Cary MS, Chung K, Takacs P, Sammel MD, et al. Predicting the decline in human chorionic gonadotropin in a resolving pregnancy of unknown location. Obstet Gynecol. 2013 Aug;122(201):337-43.
-
6. Doubilet PM, Benson CB, Bourne T, Blaivas M. Diagnostic criteria for nonviable pregnancy early in the first trimester. Ultrasound Q. 2014;30(1):3–9.
-
7. Wu HL, Marwah S, Wang P, Wang QM, Chen XW. Misoprostol for medical treatment of missed abortion: A systematic review and network meta-analysis. Sci Rep. 2017; 7: 1664.
-
8. Kanmaz AG, Inan AH, Beyan E, Budak A. The effects of threatened abortions on pregnancy outcomes. Ginekol Pol. 2019; 90(4):195-200.
-
9. Zhou J, Huang Z, Pan X, Leung WT, Li C, Chen L, et al. New thoughts in exploring the pathogenesis, diagnosis, and treatment of threatened abortion. BioScience Trends. 2019 13(3):284-285.
-
10. Birch JD, Gulati D, Mandalia S. Cervical shock: A complication of incomplete abortion. BMJ Case Rep. 2017; 2017: bcr2017220452.
-
11. Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L. Medical treatments for incomplete miscarriage. Cochrane Database of Systematic Reviews. 2017 Jan;2017(1):CD007223.
-
12. Hendriks E, Macnaughton H, Mackenzie MC. First trimester bleeding: Evaluation and management. Am Fam Physician. 2019; Feb 1;99(3):166-174.
-
13. Ford HB, Schust DJ. Recurrent pregnancy loss: etiology, diagnosis, and therapy. Rev Obstet Gynecol. 2009 Spring; 2(2):76–83.
-
14. Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD. Management of Unintended and Abnormal Pregnancy: Comprehensive Abortion Care. 2009 May. doi: 10.1002/9781444313031.
-
15. Eschenbach DA. Treating spontaneous and induced septic abortions. Obstet Gynecol. 2015 May;125(5):1042-8.
-
16. Tuuli MG, Norman SM, Odibo AO, MacOnes GA, Cahill AG. Perinatal outcomes in women with subchorionic hematoma: A systematic review and meta-analysis. Obstetrics and Gynecology. 2011 May;117(5):1205-12.
-
17. Heller HT, Asch EA, Durfee SM, Goldenson RP, Peters HE, Ginsburg ES, et al. Subchorionic hematoma: Correlation of grading techniques with first-trimester pregnancy outcome. J Ultrasound Med. 2018 Jul;37(7):1725-1732.
-
18. Griebel CP, Halvorsen J, Golemon TB, Day AA. Management of spontaneous abortion. American Family Physician. 2005 Oct 1;72(7):1243-50.
-
19. Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: Prospective study from general practice. Br Med J. 1997 Jul 5;315(7099):32-4.
-
20. Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: Prospective register based study. BMJ. 2019 Mar 20;364:l869.
-
21. Wong SF, Lam MH, Ho LC. Transvaginal sonography in the detection of retained products of conception after first-trimester spontaneous abortion.
-
J Clin Ultrasound. 2002 Sep;30(7):428-32.
-
22. The American College of Obstetricians and Gynecologists Practice Bulletin no. 150. Early pregnancy loss. Obstet Gynecol. 2015 May;125(5):1258-67.
-
23. Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM. A Comparison of Medical Management with Misoprostol and Surgical Management for Early Pregnancy Failure. N Engl J Med. 2005 Aug 25;353(8):761-9.
Articole din ediţiile anterioare
Sarcina implantată pe cicatricea operaţiei cezariene: propunere a unui ghid de practică medicală pentru diagnostic şi tratament
Având în vedere numărul mare de intervenţii chirurgicale de tipul operaţiei cezariene în România şi faptul că am întâlnit în practica noastră mai m...
Sarcina cicatricială după operaţia cezariană – o continuă dilemă terapeutică. Serie de cazuri şi review al literaturii
Sarcina cicatricială după operaţie cezariană (CSP) este o tulburare iatrogenă care pune viaţa în pericol, cu o incidenţă tot mai mare, din cauza cr...