Adenocarcinomas are the most common histological types of lung cancer. Among them, primary pulmonary mucinous adenocarcinoma (former bronchioloalveolar carcinoma) is rarely encountered, with atypical presentation, which lends itself to diagnostic confusion. We present the case of a 78-year-old, non-smoker female patient who presented for chronic cough for over a year, accompanied by mucous expectoration and dyspnea in decubitus. Radiologically she presented condensation processes in bilateral extension. Computed tomography showed condensation processes and bilateral nodules with aeric bronchogram and a possible left lower lobe tumor process. The bronchoscopy with bronchoalveolar lavage was non-diagnostic, the confirmation of mucinous adenocarcinoma being made by surgical pulmonary biopsy. The investigations excluded an extrapulmonary starting point. The diagnostic process imposed the exclusion of other aetiologies: an interstitial lung disease or an infectious cause. Atypical presentation is likely to result in diagnostic confusion and delay in diagnosis.
Adenocarcinom mucinos pulmonar primitiv la o femeie nefumătoare
Primary pulmonary mucinous adenocarcinoma in a non-smoker woman
First published: 20 decembrie 2017
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.41.4.2017.1350
Abstract
Rezumat
Adenocarcinoamele sunt cele mai frecvente tipuri histologice de cancer pulmonar. Dintre ele, adenocarcinomul mucinos pulmonar primitiv (fostul carcinom bronhiolo-alveolar) este rar întâlnit, cu prezentare atipică, ce pretează la confuzii de diagnostic. Prezentăm cazul unei paciente de 78 de ani, nefumătoare, care s-a prezentat pentru tuse cronică de peste un an, însoţită de expectoraţie mucoasă şi dispnee de decubit. Radiologic, prezenta procese de condensare în extensie bilaterală. Examenul tomografic computerizat a evidenţiat procese de condensare şi noduli bilaterali cu bronhogramă aerică şi un posibil proces tumoral de lob inferior stâng. Bronhoscopia cu lavaj bronhoalveolar a fost nondiagnostică, confirmarea adenocarcinomului mucinos fiind făcută prin biopsie pulmonară chirurgicală. Investigaţiile au exclus un punct de plecare extrapulmonar. Procesul diagnostic a impus excluderea altor etiologii: o boală interstiţială pulmonară sau o cauză infecţioasă. Prezentarea atipică pretează la confuzii de diagnostic şi la întârzierea diagnosticului.
Introduction
Lung cancer is one of the main causes of morbidity and mortality due to neoplastic disease worldwide, and in most cases it is associated with smoking. Adenocarcinoma is the most common type of histology, responsible for half of the cases.
Recently, The International Society for the Study of Lung Cancer (IASCL), The American Thoracic Society and The European Respiratory Society published together a histological classification of adenocarcinomas, particularly useful for the prognostic value of the histological type of cancer(1).
Mucinous adenocarcinoma, previously called bronchioalveolar carcinoma, is the rarest type of lung adenocarcinoma, with a frequency of 2-6% of non-small pulmonary carcinomas(2).
The occurrence of such a lung cancer in a non-smoker female person may raise differential diagnosis problems and lead to a delay in diagnosis.
Case presentation
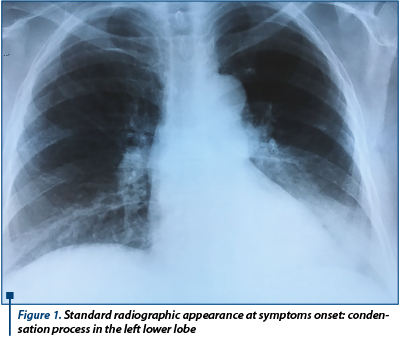
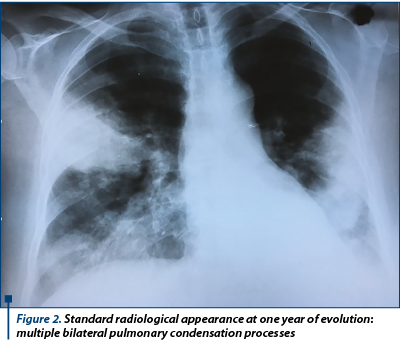
A 78-year-old female patient was admitted by transfer from a provincial pneumophtisiology hospital for diagnosis. The female patient, who was not a smoker and had a history of hypertension in treatment, without any exposure, had chronic cough for more than a year, which had associated dyspnea at exertion and dyspnea in decubitus for the past 6 months. She received inhaled bronchodilators without symptom relief. In October 2016, a pulmonary radiological examination revealed a left basal pulmonary consolidation, considered a left lower lobe pneumonia, for which she received oral antibiotic treatment (Figure 1). The radiological image remained unchanged after one month. In October 2017, she was hospitalized due to intensified cough, which became productive with abundant mucous expectoration; the radiological image showed this time the persistence of the left basal consolidation and the addition of multiple bilateral condensation processes (Figure 2). In hospital, she received antibiotics (beta-lactams and fluoroquinolones) and inhaled bronchodilators, without improvement of the symptoms.
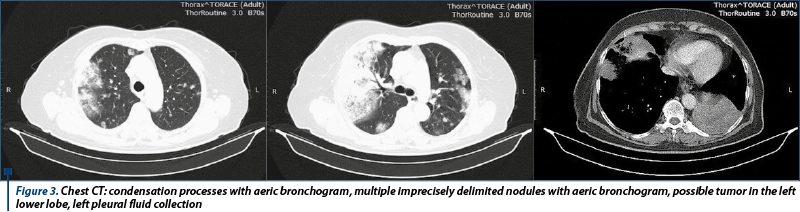
A chest computed tomographic scan (Figure 3) has been performed, showing numerous bilateral opacities, some nodules of different dimensions, ill defined, with aeric bronchogram or tendency to excavate, bilateral non-systemic consolidations with aeric bronchogram, as well as a possible tumor practically occupying the entire left lower lobe accompanied by a small left pleural effusion.
Upon admission to our clinic, the patient had a relatively good overall status with SaO2 measured percutaneously at rest in atmospheric air of 94%. Pulmonary auscultation revealed multiple bilateral subcrepitant crackles and ronchuses.
There was no peripheral adenopathy, the rest of the physical examination was normal.
Serologic tests showed a mild anemia (hemoglobin 11.2 g/dL), mild leukocytosis (WBC 11.200/mmc), and inflammatory syndrome with ESR of 64 mm at 1 hour. The rest of the performed tests were normal.
A fibrobronchoscopic examination was performed which did not reveal macroscopic changes in the bronchial mucosa.
A broncho-alveolar lavage (BAL) in the left lower lobe bronchus was attempted, without recovery of the lavage fluid, therefore BAL was performed in the territory of the left upper lobe bronchus, with a good recovery of a slightly opalescent liquid. Differential cytology of the lavage fluid showed very mild lymphocytosis (18.6%), with no evidence of tumor cells or germs, negative staining for acid fast bacilli.
At this point, based on the symptoms and the imaging aspect, several diagnostic assumptions were considered: diffuse interstitial pneumonia, possibly a granulomatosis with polyangeitis, due to the presence of excavated nodules, but the serology for the cANCA and pANCA antibodies was negative; a lung infection, but the long evolution with afebrility, the lack of response to antibiotic treatments and the absence of germs or mycobacteria in the BAL fluid contradicted the hypothesis; a primary pulmonary neoplasia of the type of a mucus-secreting adenocarcinoma or multiple pulmonary metastases of extrapulmonary origin, but was not supported by the presence of tumor cells in the bronchoalveolar lavage fluid.
The need for a surgical pulmonary biopsy has been called into question, in order to establish the diagnosis with certainty. Despite the advanced age, the patient had a good overall condition with no signs of heart failure, with a normal electrocardiogram, and the ventilatory function measured by spirometry was normal (vital capacity of 1.77 L - 86.8% of the predicted value; FEV1 of 1.55 L - 93.6% of the predicted value; FEV1/VC value of 87%).
The patient was transferred to the thoracic surgery department and pulmonary biopsy was performed in the middle lobe through a thoracoscopic approach. The postoperative evolution was without complications, the patient being discharged after 3 days.
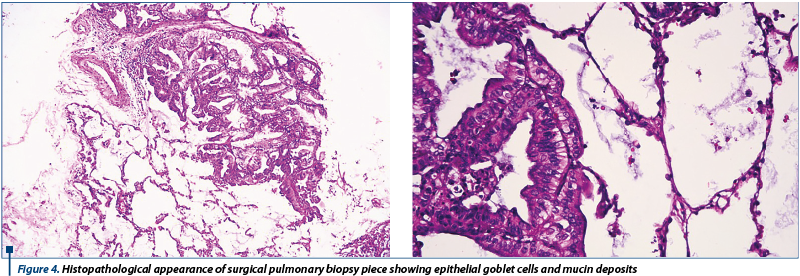
The histopathological examination of the resection piece revealed a mucinous adenocarcinoma with neoplastic infiltration and a predominantly lepidic pattern, acinar and papillary zoning, consisting of goblet cell carcinoma cellular elements (Figure 4).
The immunohistochemical examination revealed negative TTF1 in tumor cells, positive in the alveolar epithelium, Ck7 positive in tumor cells, 30% positive KI67; conclusion: adenocarcinoma infiltrates, without being able to identify with certainty the primitive pulmonary histogenesis or metastasis from a bilio-pancreatic adenocarcinoma.
Genetic tests revealed the absence of ALK and EGFR mutations.
Even after the elucidation of the malignancy and the histological type of adenocarcinoma, it remained questionable whether the patient had a primitive pulmonary carcinoma or pulmonary metastases from an extrapulmonary adenocarcinoma. For this, additional investigations have been carried out.
Mammography did not reveal mammary tumors. Repeated CT scan with the inclusion of the cerebral, abdominal and pelvic segments excluded abdominal or genital tumors or adenopathies, revealing only an 11 mm right anexial cyst with a residual cyst aspect. Abdominal echography did not reveal biliary or pancreatic changes.
The patient was subsequently hospitalized in the oncology department where therapy with gemcitabine and platinum salts was initiated, being well-tolerated, and improved the cough.
Discussions
Mucinous pulmonary adenocarcinoma, previously called bronchioalveolar carcinoma, is the least common type of lung adenocarcinoma, with a frequency of 2-6% of non-small pulmonary carcinomas(1,2). It was originally described as a form of peripheral carcinoma, growing as a single layer of malignant cells along the terminal airways.
Mucus production is characteristic of this type of adenocarcinoma(2,3). Patient survival depends on the extent of the disease at the time of diagnosis, but the predominantly lepidic type appears to have better survival than other histological types(4).
The international classification of lung adenocarcinomas(1) recommended the renunciation of the term bronchio-alveolar carcinoma, this category being replaced by several histological subtypes:
- In situ adenocarcinoma (AIS), which may be non-mucinous and rarely mucinous.
- Minimally Invasive Adenocarcinoma (MIA).
- Predominantly lepidic adenocarcinoma (non-mucinous).
- Predominantly invasive adenocarcinoma with a lepidic component.
- Invasive mucinous adenocarcinoma (previously called mucinous bronchio-alveolar carcinoma).
Histologically, in mucinous adenocarcinoma, tumor cells have a morphologically distinctive goblet cell or columnar cell appearance with intracytoplasmic abundant mucin. Cellular atypia are missing or insignificant. Alveolar spaces often contain mucin. These tumors may present a mixture of lepidic, acinar, papillary, micropapillary or solid growth elements. Unlike AIS or MIA types, it is characterized by dimensions over 3 cm, invasion over 0.5 cm, multiple nodules or lacking a circumscribed border with milliar spread in the surrounding parenchyma(1).
These tumors tend to exhibit KRAS mutations and most often lack the expression of thyroid transcription factor-1(3,5).
From the clinical point of view, these carcinomas have a long evolution, with symptoms dominated by productive chronic cough with mucous expectoration that can become abundant, originating in mucus production of tumor cells(6). From the imaging point of view, the initial changes on standard pulmonary X-ray suggest a pneumonia that does not improve under antibiotic treatment, and the appearance over time of new condensations in both lungs is characteristic. The thoracic CT examination detects, besides the condensation processes, nodular opacities of various dimensions, predominantly in upper lobes, with ill defined limits, different sizes and the presence of aeric bronchogram, pseudocavities and hyperlucencies. Changes are not characteristic, predisposing to diagnostic confusion(7).
Positive diagnosis is based on histopathological and immunohistochemical confirmation, though it is often difficult to distinguish between a primitive pulmonary carcinoma and secondary determinations from a carcinoma outside the lungs.
Primary mucinous pulmonary adenocarcinomas are rare tumors, however, literature citations are marked by classification difficulties(8-11).
Also in the case of our non-smoker patient, the symptomatic evolution of the disease was marked by confusion with a pneumonia or a chronic obstructive disease, and the diagnosis could only be confirmed by surgical lung biopsy.
Conclusion
The presented case raises the problem of the difficult differential diagnosis of a rare type of pulmonary cancer, primary mucinous adenocarcinoma, in which positive diagnosis and differentiation from other infectious or inflammatory pulmonary diseases could only be performed by surgical pulmonary biopsy.
Bibliografie
2. Marchetti A, Buttitta F, Pellegrini S, Chella A, Bertacca G, Filardo A, Tognoni V, Ferreli F, Signorini E, Angeletti CA, Bevilacqua G. Bronchioloalveolar lung carcinomas: K-ras mutations are constant events in the mucinous subtype. J Pathol. 1996;179:254–259.
3. Marchetti A, Buttitta F, Pellegrini S, Chella A, Bertacca G, Filardo A, Tognoni V, Ferreli F, Signorini E, Angeletti CA, Bevilacqua G. Bronchioloalveolar lung carcinomas: K-ras mutations are constant events in the mucinous subtype. J Pathol. 1996 Jul;179(3):254-9.
4. Hung JJ, Jeng WJ, Chou TY, Hsu WH, Wu KJ, Huang BS, Wu YC. Prognostic value of the new International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society lung adenocarcinoma classification on death and recurrence in completely resected stage I lung adenocarcinoma. Ann Surg. 2013 Dec;258(6):1079-86.
5. Zhen Chen, Xiaoyan Liu, Jing Zhao, Hanjin Yang, XiaodongTeng. Correlation of EGFR mutation and histological subtype according to the IASLC/ATS/ERS classification of lung adenocarcinoma. Int J ClinExpPathol. 2014; 7(11): 8039–8045.
6. Clayton F. Bronchioloalveolar carcinomas. Cell types, patterns of growth, and prognostic correlates. Cancer. 1986 Apr 15;57(8):1555-64.
7. Karthikeyan D. High Resolution Computed Tomography of the Lungs – A Practical Guideline, second edition. The Health Sciences Publishers 2015, p. 145-146.
8. Yan Liu, He-Long Zhang, Jia-Zhuan Mei, Yan-Wei Guo, Rui-Jun Li, Si-Dong Wei, Fu Tian, Lu Yang, Hui Wang. Primary mucinous adenocarcinoma of the lung: A case report and review of the literature. OncolLett. 2017 Sep; 14(3): 3701–3704.
9. Cabibi D, Sciuto A, Geraci G, Lo Nigro C, Modica G, Cajozzo M. Cystic mucinous adenocarcinoma of the lung: a case report. J Cardiothorac Surg. 2011; 6: 128.
10. Takanashi Y, Tajima S, Tsukui M, Shinmura K, Hayakawa T, Takahashi T, Neyatani H, Funai K. Non-Mucinous Lepidic Predominant Adenocarcinoma Presenting with Extensive Aerogenous Spread. Rare Tumors. 2016 Dec 7;8(4):6580.
11. Xu X, Guo Y, Li Q, Yang L, Kang J. Invasive mucinous adenocarcinoma with lepidic-predominant pattern coexisted with tuberculosis: a case report. Front Med. 2017 Jul 8. doi: 10.1007/s11684-017-0545-4. [Epub ahead of print]
Articole din ediţiile anterioare
Abordarea chirurgicala a unui nodul pulmonar solitar la un pacient cu o neoplazie in antecedente
Un nodul pulmonar solitar reprezintă o opacitate radiologică, mai mică de 3 centimetri, înconjurată de parenechim pulmonar normal, fără alte modifi...
Carcinomul pulmonar scuamos
Cancerul pulmonar fără celule mici scuamos este unul dintre cancerele care nu are încă un avantaj cert în cadrul terapiei țintite. Deși rezultatele...
Un al doilea cancer pulmonar primar, cu masă intracardiacă dezvoltată după malignitate renală – prezentare de caz şi review al literaturii
Metastazele cardiace nu sunt pe atât de rare pe cât se consideră, incidenţa lor fiind cuprinsă între 2,3% şi 18,3%, cel mai adesea secundare ca...
Radiomica şi radiogenomica în managementul cancerului bronhopulmonar – o scurtă recenzie
Cancerul bronhopulmonar este principala cauză a mortalităţii prin cancer, diagnosticul tardiv fiind una dintre cauzele asociate cu decesul şi cu ...