Dermatofibrosarcoma protuberans (DFSP) is a rare form of skin cancer characterized by local aggressiveness, typically affecting individuals in the young to middle-aged adult range. The authors of this article aimed to present the clinical picture, as well as the therapeutic approach to a patient undergoing oncological surveillance with DFSP, analyzing the therapeutic response rate based on data published in specialized journals. A 72-year-old man was admitted to the radiation oncology department, having
a 75/58 mm tumoral mass on the right posterior cervical region. The patient underwent two radical tumor excision surgeries and interval skin grafting, leading to a negative prognosis for the patient, as the tumor reappeared aggressively in a short period, four months, more exactly. The study highlighted the importance of surgical intervention, such as wide local excision, in preventing recurrence and the major role of initiating timely adjuvant treatment, including radiotherapy. The previously performed studies
suggest that radiotherapy can be beneficial following resection with negative margins, and it can serve as primary therapy for patients with inoperable or incompletely excised DFSP. In this case, the only therapeutic response was stopping the progression of the tumor growth and macroscopic changes of the tumor surface with areas of necrosis. This study also discusses the use of imatinib as the only left therapeutic option, due to the lack of radiotherapy response.
Clinical and therapeutic particularities in dermatofibrosarcoma protuberans – a case report
Particularităţi clinice şi terapeutice în dermatofibrosarcomul protuberans – studiu de caz
First published: 27 martie 2024
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.66.1.2024.9382
Abstract
Rezumat
Dermatofibrosarcomul protuberans (DFSP) este o formă rară de cancer cutanat, caracterizată prin agresivitate locală, întâlnită cu predilecţie la populaţia de vârstă tânără până la vârstă mijlocie. Autorii articolului şi-au propus să prezinte tabloul clinic, precum şi abordarea terapeutică în cazul unui pacient aflat sub supraveghere oncologică pentru DFSP, analizând rata de răspuns terapeutic corelată cu datele publicate în revistele de specialitate. Un bărbat în vârstă de 72 de ani a fost internat în departamentul de radioterapie pentru apariţia unei mase tumorale de 75/58 mm în regiunea cervicală posterioară dreaptă. Pacientul a urmat două intervenţii chirurgicale de excizie incompletă a tumorii şi grefare cu lambou cutanat, excizia incompletă fiind un factor de prognostic nefavorabil, cu decelarea recidivei tumorale într-un timp relativ scurt, mai exact, în patru luni. Studiul a subliniat importanţa intervenţiei chirurgicale, care constă în excizie locală largă pentru prevenirea recurenţei, şi rolul major al iniţierii în timp util a tratamentului adjuvant, inclusiv a radioterapiei. Studiile anterior efectuate sugerează că radioterapia poate fi benefică după rezecţia tumorală cu margini de excizie negative şi poate servi ca terapie primară pentru pacienţii cu DFSP inoperabil sau excizat incomplet. În cazul acestui pacient, răspunsul terapeutic a constat în încetinirea progresiei tumorale şi instalarea macroscopică a fenomenului de necroză la nivelul suprafeţei tumorale. În acest studiu, autorii discută, de asemenea, importanţa imatinibului ca singura opţiune terapeutică în lipsa răspunsului la radioterapie.
Introduction
Dermatofibrosarcoma protuberans (DFSP) is a type of sarcoma characterized by local aggressiveness and low malignancy rate, typically affecting individuals in the middle-aged adult range. DFSP typically manifests on the trunk in 50-60% of cases, on the proximal extremities in 20-30%, and on the head and neck in 10-15% of cases. It commonly targets the shoulder or pelvic area. Initially, it appears as a painless, red, hardened patch, which later progresses into a violet or red-brown mass ranging from one to several centimeters in size, and also in its macroscopical aspect(1).
Given the rarity of this oncological entity, the authors of the article aimed to present the clinical picture, as well as the therapeutic approach to a patient undergoing oncological surveillance with dermatofibrosarcoma protuberans, analyzing the therapeutic response rate based on data published in specialized journals.
Background
A 72-year-old man was admitted to the radiation oncology department after he accused the occurrence of a 75/58 mm tumoral mass on the right posterior cervical region (Figure 1).

From his medical history, the patient was first addressed to the oncologist in March 2023 for a similar tumoral mass which was operated on the following month using wide local excision followed by a free lap reconstructive surgery. After resection, the histopathological report showed a partially fragmented tumoral mass which weighed 1015 grams and was divided into two fragments. Macroscopically, the bigger fragment had 15.5/12/9.5 cm, having a multinodular aspect with multiple ulcerative areas and a skin layer over it. The smaller fragments sum up to 15.5/14.5/5 cm. The histopathological aspect shows suggestive elements of dermatofibrosarcoma protuberans.
The result of the immunohistochemical examination performed on the resected specimen concluded that the morphological appearance and the immunohistochemical profile were consistent with the diagnosis of dermatofibrosarcoma protuberans, invading the striated muscle.
After surgery, the patient did not see the medical oncologist for an oncological checkup and to continue the adjuvant treatment until after a four-month interval, when a contrast-enhanced MRI examination of the cervical region revealed significant tumor recurrence of the previously known lesion, exhibiting the same contrast pattern and mass effect.
The patient underwent a new extensive surgical intervention during which the newly appeared tumor formation at that time was excised, and a new skin flap was applied. The histopathological bulletin data once again proved the diagnosis of dermatofibrosarcoma protuberans, histological differentiation grade G2, according to FNCLCC, which was excised under safe surgical conditions.
Due to the patient’s advanced age and having undergone two surgical interventions within half a year, involving tissue reconstruction in the affected region, the oncologist decided to postpone radiotherapy treatment for four months, because the skin flap needed a longer time to heal.
Similarly, considering the patient’s age and the associated cardiovascular comorbidities, it was decided to postpone systemic therapy and evaluate the appropriate timeframe of its administration based on the response to local radiotherapy treatment.
Four months later, upon repeating the MRI examination, the maintenance imagistic aspect of the tumor mass in the right posterior cervical soft tissue was observed.
We mention that, after the second surgical intervention, the clinical aspect showed complete surgical excision with apparently no evidence of tumoral tissue invasion. Therefore, at the four-month interval MRI checkup, what was pathologically detected likely represented a continuation of local progression, demonstrating increased tumor aggressiveness despite the moderate malignancy grade (G2).
The patient showed up to the radiotherapy department upon the oncologist’s recommendation for consultation and the initiation of specialized treatment. Following CT scanning and medical record analysis, it was decided to initiate radiotherapy as treatment.
Upon objective examination, we observed an oval-shaped tumor mass located in the right posterior cervical region, approximately 75/58 mm in size, with a pink-reddish color, minimal marginal areas of necrosis, ulceration, and bleeding (Figure 1). The surface of the tumor was friable, shiny, and showed signs of inflammation. Daily cleaning of the lesion and application of basic silver nitrate band-aids were recommended.
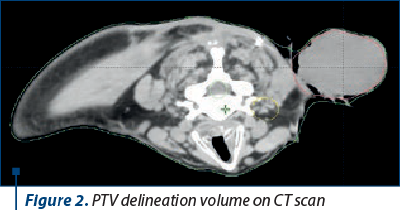
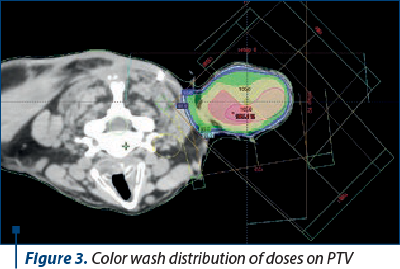
The radiotherapeutic treatment plan included initial CT scanning on a GE Medical Systems CT scanner, in headfirst prone position, followed by contouring which includes the creation of planning target volumes and organs at risk (OARs). Regarding the treatment plan and the structures delineated, the clinical target volume (CTV) of the tumor formation and its planning target volume (PTV) were delineated, adding a margin of 0.3 mm to the CTV (Figures 2 and 3).
Following the treatment plan implementation, the organs at risk were outlined, including the right brachial plexus. This anatomical structure received a maximum radiation dose of 29.51 Gray and a mean radiation dose of 5.72 Gray, as determined by the dosimetric evaluation. Monitoring the macroscopic evolution of the tumor weekly, it was observed that its dimensions remained the same as those at the time of presentation. Additionally, on the surface of the tumor, the progression of superficial necrosis was observed, which was present in a larger area compared to the initiation of treatment (Figures 4 and 5).


During irradiation, after 20 sessions of radiotherapy, totaling a dose of 60 Gray (3 Gray/fraction), the post-therapeutic aspect was one of stable disease (Figure 6),

contradicting the results published in specialized journals, which specify the existence of a therapeutic response in cases of DFSP. Although the final aspect regarding the dimensions of the tumor was stationary disease, we need to point out the fact that, after the macroscopic evaluation, tumoral necrosis was observed almost on all of the tumoral surface. In the case of the presented patient, the therapeutic factors that negatively influenced the response to radiotherapy were the delayed initiation of radiotherapy due to the risk of dehiscence of the skin flap, considering that the optimal interval for initiating treatment to achieve a therapeutic response after irradiation is as early as possible after surgical intervention.
Also, an unfavorable histopathological prognostic factor that influences the response to radiotherapy is the safety of surgical resection margins. Specialized publications report beneficial results of adjuvant radiotherapy in cases where tumors are excised with oncological safe margins of 1 cm. The recommended surgical technique for DFSP is the Mohs technique, which is a meticulous method used to remove skin cancer while preserving healthy tissue. The procedure involves several key steps, including tumor removal (the visible tumor and a small amount of surrounding tissue are surgically excised), tissue examination (the removed tissue is promptly examined under a microscope to detect any cancer cells at the margins), and closure (once the cancer is entirely excised, the wound is closed using appropriate methods). Mohs surgery boasts high cure rates and minimal tissue loss, making it especially advantageous for treating skin cancer, particularly in cosmetically sensitive regions. Additionally, in cases where through this technique the oncological safe resection margins cannot be ensured, wide excision of the tumor is recommended.
In the case of the presented patient, during the second surgical intervention for recurrence, issues were encountered in properly managing the surgical treatment protocol at the time of excision and reconstruction using a skin flap. Despite the necessity for a wide excision, given the tumor’s location in an anatomically significant region for mobility of the musculoskeletal system, an attempt was made to perform an optimal tumor excision to ensure both functional and esthetic outcomes. However, it was not possible to achieve an excision with oncological safe margins. This surgical deficit, due to the tumor’s location, along with the delayed initiation of radiotherapy for three months due to the risk of skin flap dehiscence, constituted unfavorable histopathological and therapeutic prognostic factors that led to a lack of response to radiation therapy.
Although data from specialized literature report the existence of a therapeutic response for DFSP treated radically with oncological safe margins and adjuvant radiotherapy, in the case of our patient, the inability to ensure a radical intervention due to tumor localization and the delayed radiotherapy led to a lack of therapeutic response after adjuvant radiotherapy. However, considering that the patient had contraindications for systemic therapy due to associated comorbidities and that the treatment ensuring the key to therapeutic success in DFSP is local surgery followed by adjuvant radiotherapy, it was decided to proceed with radiotherapy even after the delayed or suboptimal therapeutic interval.
The clinical evaluation post-radiotherapy revealed a stable dimensional disease aspect (7/5 cm versus 6.8/5 cm), however, with the onset of tumor necrosis detected by the change in color appearance on the tumor’s surface from reddish at the beginning of treatment to dark brown at the end of irradiation. The aspect of stable disease has an unfavorable impact on the patient’s prognosis, which remains reserved, with the only therapeutic alternative being the administration of targeted molecular therapy, namely imatinib.
Discussion
Characterized by slow growth, dermatofibrosarcoma protuberans commonly manifests itself as a superficial nodule on the trunk or limbs(2). In the initial stages of DFSP, patients typically observe a slow-growing, small, firm, painless, skin-colored dermal plaque, subcutaneous thickening, or atrophic non-protuberant lesion. Without treatment, these tumors can invade deeper layers such as the fascia, muscle and bone, and they occasionally metastasize to distant organs in advanced stages. The tumor cells commonly metastasize to the lungs, brain, bones, visceral organs, lymph nodes, and soft tissues. This gradual growth process takes several months. Dermatofibrosarcoma protuberans are most often found on the trunk, followed by the proximal extremities, and then the head and neck(3). Despite its local aggressiveness and frequent recurrence post-surgery, the prognosis is typically favorable with effective treatment(2).
In this patient’s case, the disease progression has been rapid and aggressive. The tumor growth rate was high, and the postoperative recurrence occurred after both wide excision surgeries, albeit within the limits of technical feasibility, considering the irradiated region. The literature indicates the possibility of distant metastasis in the absence of treatment, yet metastasis was not evident on the last MRI, despite the patient not receiving adjuvant treatment for eight months. Therefore, the particularity of this case lies primarily in the high tumor aggressiveness, with the occurrence of two tumor recurrences within an eight-month interval, despite the moderately differentiated malignancy grade.
Dermatofibrosarcoma protuberans is characterized by a slow progression and infrequent metastasis. However, it often exhibits extensive subclinical spread and recurs frequently following standard excision. DFSP, a rare form of skin cancer, can benefit significantly from Mohs surgery due to its effectiveness. If Mohs surgery is not feasible, staged excision with proper confirmation of clear margins by pathology can also serve as an effective treatment for DFSP(4).
The treatment of choice in this case was initially surgical excision, with the use of a skin flap for reconstructing the esthetic deficit created by tumor excision. Due to recurrence after the first intervention in a short period, it was decided, four months later, to again remove the recurrent tumor formation using the same type of surgical intervention, namely limited excision with esthetic deficit reconstruction through another skin flap. Because two large skin grafts were performed in less than six months on an elderly patient in a poorly vascularized area with significant joint mobility, there were issues with securing the skin flap, necessitating a delay in radiotherapy to promote proper healing of the used skin flap. Thus, surgical treatment was not a radical therapeutic alternative that would imply a favorable prognosis, and the lack of assurance of surgical radicality as well as the increased tumor aggressiveness certainly explain the occurrence of tumor recurrence in a short time interval.
In cases were achieving negative margins post-surgery for DFSP proves to be challenging, the consideration of adjuvant radiotherapy (RT) may be warranted to enhance local control and mitigate potential cosmetic or functional complications(5).
Specialized studies have demonstrated the long-term efficacy of adjuvant postoperative radiotherapy under the condition of early initiation, specifically immediately after surgery. We decided on radiotherapy despite deep tumor invasion at the surgical margins in both surgical interventions, as systemic therapy couldn’t be administered, with the only possible treatment being local radiotherapy aimed at reducing the risk of local recurrence. Although adjuvant radiotherapy was administered at maximum doses with curative intent, the delay in irradiation had a negative impact on the therapeutic response, resulting in a stable tumor size (7/5 cm versus 6.8/5 cm), with the onset of tumor necrosis clinically detectable by the change in macroscopic appearance on the tumor surface.
If surgery is not feasible or would result in undesirable functional or cosmetic consequences, radiotherapy is an alternative treatment choice, if not previously preoperatively administered, or imatinib mesylate is indicated. Imatinib mesylate, an FDA-approved protein tyrosine kinase inhibitor, is recommended for treating unresectable, recurrent and/or metastatic DFSP in adults due to its ability to inhibit PDGF receptor overactivity in tumor cells. Given the DFSP’s recurrent nature, potential therapy with imatinib and radiotherapy could avoid functional impairment, as further resection would lead to functional loss(6).
Imatinib mesylate, an oral tyrosine kinase inhibitor used for recurrent, unresectable and metastatic DFSP, is not primarily aimed at cure but rather at management. This medication competitively inhibits ATP binding to the PDGF-beta receptor, thereby slowing kinase activity, restraining tumor growth, and promoting apoptosis. Patients with the t (17;22) translocation tend to respond better to imatinib mesylate, with studies indicating a response rate of approximately 65%(7).
The treatment with imatinib has provided favorable and excellent long-term prognostic results over time. Although it is known that this therapeutic agent is a very good alternative for adjuvant treatment in the case of our patient, its initiation was postponed due to associated comorbidities, namely cardiovascular pathologies. The patient did not have contraindications related to cardiovascular comorbidities, so imatinib therapy could be initiated. However, considering the aspect of stable disease after the administered radiotherapy, the patient remains an ideal candidate for this therapy with the aim of delaying the recurrence of local or distant tumor growth.
These chromosomal alterations lead to the development of a distinct fusion gene, COL1A1-PDGFB, identifiable in both ring chromosomes and translocations. Currently, the COL1A1-PDGFB fusion gene stands as the sole identified fusion gene associated with this tumor type(8). This leads to the increased expression of the COL1A1-PDGFB fusion protein, which further matures into a homodimer PDGF-BB. Consequently, there is continuous autocrine activation of the PDGFB receptor (PDGFRB), a protein tyrosine kinase known to act as a potent growth factor(8).
During the previously conducted research, we came across a study on the effects of imatinib on DFSP, in which the authors described the case of a patient experiencing local recurrence and metastasis of DFSP, who underwent treatment with imatinib mesylate at a dosage of 400 mg/day. The tumor was analyzed using FISH technique to detect specific rearrangements of the PDGFB locus. Response and potential side effects were monitored through physical examinations and imaging studies. FISH analysis revealed PDGFB rearrangement, indicating multiplication of the PDGFB fusion locus within a ring chromosome. The physical examination showed a positive response within the first month of treatment, and subsequent computed tomography and fluorodeoxyglucose positron emission tomography scans confirmed the complete response to imatinib treatment. The patient has now been in sustained complete remission for 20 months(9).
A study published in 2016 presented a case of recurrent dermatofibrosarcoma protuberans and its management through radical excision and skin grafting. The case report highlights the successful management of recurrent DFSP, leading to a positive prognosis for the patient. The study emphasizes the importance of the appropriate time of proceeding surgical intervention, such as wide local excision, in preventing the recurrence of DFSP. Additionally, it discusses the clinical features of DFSP, regarding significant local destructive effects, and the changes it gets as it progresses. The majority of DFSP cases exhibit a specific genetic fusion transcript that contributes to its pathogenesis(10).
Another study published in 2020 investigated the role of radiotherapy in the management of dermatofibrosarcoma protuberans. The research included 28 patients with DFSP who underwent radiotherapy, with a median follow-up period of five years. The study revealed that adjuvant radiotherapy resulted in 93-98% local control rates at five and ten years. The findings suggest that radiotherapy can be beneficial following resection with close or positive margins when re-excision is not feasible, and can serve as primary therapy for patients with inoperable or incompletely excised DFSP. However, the study emphasizes the fact that the role of adjuvant radiotherapy in DFSP remains a topic of debate, considering the need for further research to determine optimal dosage(11).
Mohammadreza Amjadzadeh and Parvin Mousavi Ghanavati discussed in their study from April 2020 the management of dermatofibrosarcoma protuberans and its prognosis. The study highlights the importance of complete surgical excision with a wide margin of surrounding tissue to prevent recurrence. The study analyzes the role of radiation therapy in the local management of DFSP, with early studies demonstrating its benefits in unresectable or incompletely excised cases. The study also discusses the use of imatinib with radiation therapy, suggesting that this combination may be effective in managing DFSP, particularly in cases where surgery is not possible or incomplete(11).
Many skin tumors are formed with different cell types, such as fibroblasts, endothelial cells, and smooth muscle cells. These tumors often display a spindle cell morphology, and specific morphological characteristics help determine the origin of the cell and a more accurate diagnosis. For example, smooth muscle cells typically have nuclei shaped like cigars with rounded ends. Dermatofibromas are benign growths characterized by a hyperplastic epidermis that often display hyperpigmentation, termed “dirty feet”. Unlike dermatofibrosarcoma protuberans, atypical fibroxanthomas exhibit significant cytologic atypia of spindled and epithelioid cells within the dermis(10,12).
Conclusions
We decided to present this clinical case, considering the rarity of this pathological entity and the therapeutic approach in which, despite following a recommended treatment protocol, the response rate was not in line with the data from specialized literature. Therapeutic risk factors, such as initiating radiotherapy at a suboptimal interval and histoprognostic factors represented by tumor invasion into deep tissues that do not ensure the radicality of the surgical intervention, were the ones that had negatively influenced the response to radiotherapy. Additionally, the lack of response to the performed therapies reflects the unfavorable prognosis of this patient. Thus, the only therapeutic alternative is molecular targeted therapy with imatinib (Glivec®), with previous studies revealing a response to this medication.
Corresponding author: Anda-Elena Crişan E-mail: anda_crisan2005@yahoo.com
Conflict of interest: none declared.
Financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.

Bibliografie
-
Bolognia J, Jorizzo JL, Schaffer JV. Dermatology. 3rd Ed. Philadelphia: Elsevier Saunders, 2012, p. 1973.
-
Al Barwani AS, Taif S, Al Mazrouai RA, Al Muzahmi KS, Alrawi A. Dermatofibrosarcoma Protuberans: Insights into a Rare Soft Tissue Tumor. J Clin Imaging Sci. 2016;6:16.
-
Hao X, Billings SD, Wu F, et al. Dermatofibrosarcoma Protuberans: Update on the Diagnosis and Treatment. J Clin Med. 2020;9(6):1752.
-
Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, McMichael AJ, Orringer JS (Eds.). Fitzpatrick’s Dermatology, 9th Ed. McGraw-Hill Education, 2019, p. 3768.
-
DuBay D, Cimmino V, Lowe L, Johnson TM, Sondak VK. Low recurrence rate after surgery for dermatofibrosarcoma protuberans: a multidisciplinary approach from a single institution. Cancer. 2004;100(5):1008-16.
-
NCCN Clinical Practice Guidelines in Oncology for Dermatofibrosarcoma Protuberans. https://www.nccn.org/professionals/physician_gls/default.aspx
-
Hu M, Kuo S. Adjuvant radiotherapy for dermatofibrosarcoma protuberans: a case report. Therapeutic Radiology and Oncology. 2019;3. doi:10.21037/tro.2019.08.0
-
Rutkowski P, Klimczak A, Ługowska I, et al. Long-term results of treatment of advanced dermatofibrosarcoma protuberans (DFSP) with imatinib mesylate - The impact of fibrosarcomatous transformation. Eur J Surg Oncol. 2017;43(6):1134-1141.
-
Labropoulos SV, Fletcher JA, Oliveira AM, Papadopoulos S, Razis ED. Sustained complete remission of metastatic dermatofibrosarcoma protuberans with imatinib mesylate. Anticancer Drugs. 2005;16(4):461-466.
-
Ahmad I, Mir MA, Bariar LM, Afroz N. Recurrent Dermatofibrosarcoma Protuberance and its Management with Radical Excision and Interval Skin Grafting: A Case Report. World J Plast Surg. 2016 Jan;5(1):67-71.
-
Amjadzadeh M, Mousavi Ghanavati P. Patient with recurrence dermatofibrosarcoma protuberans: A case report. Clin Case Rep. 2020;8:1192-1194.
-
Haas RL, Keus RB, Loftus BM, Rutgers EJ, van Coevorden F, Bartelink H. The role of radiotherapy in the local management of dermatofibrosarcoma protuberans. Soft Tissue Tumours Working Group. Eur J Cancer. 1997;33(7):1055-1060.
Articole din ediţiile anterioare
Cancerul, o problemă nerezolvată
Pornind de la ideea că eşecul nostru de a vindeca cancerul vine din lipsa noastră de a înţelege complexitatea sa, ştiinţa contemporană priveşte tre...
Tratamentul paliativ şi suportiv în cancerul bronhopulmonar avansat
Lucrarea caută să prezinte concis aspecte esenţiale în terapia paliativă şi suportivă a cancerului bronhopulmonar avansat. Se face distincţia între...
Rolul radioterapiei în managementul metastazelor osoase
Metastazele osoase (MO) sunt întâlnite la unu din doi pacienți oncologici, de la prezentare sau pe parcursul evoluției bolii. Ca o regulă fundament...
Evoluţia raportului neutrofile-limfocite (NLR) şi a raportului trombocite-limfocite în timpul polichimioterapiei în cancerele capului şi gâtului
Identificarea unor biomarkeri prognostici şi predictivi în patologia oncologică este un deziderat al cercetării translaţionale în cancer.