Malignant melanoma is gaining a higher incidence every year, especially in older white men. Being a serious disease with many possible complications and secondary determinations, it should be identified earlier, and screening methods should be implemented to decrease the cases of advanced melanoma.
Un caz clinic de melanom malign de spate
A clinical case of a malignant melanoma of the back
First published: 27 aprilie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.46.1.2019.2310
Abstract
Rezumat
Melanomul malign are o incidenţă tot mai mare în fiecare an, în special la bărbaţii mai în vârstă. Fiind o boală gravă cu multe complicaţii posibile şi cu multe posibilităţi de determinări secundare, acesta trebuie identificat mai devreme, iar screeningul prezentat în acest articol ar trebui implementat pentru reducerea cazurilor de melanom avansat.
Case report
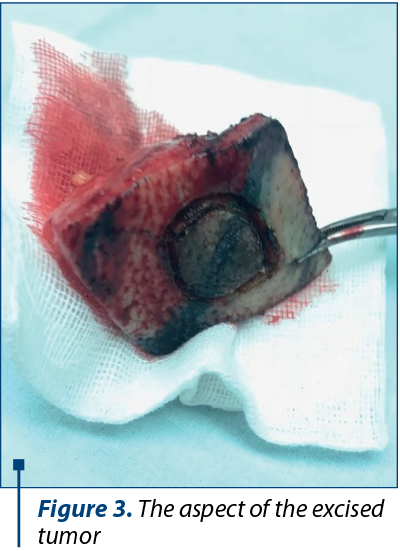
A male Romanian patient, 69 years old, was admitted to the Plastic Surgery Unit at the Bucharest University Emergency Hospital, complaining of the arising of a cutaneous tumor on the back, interscapullary, which had been growing rapidly in size and had bled several times in the previous six months. It was a firm dark brown tumor, adherent to the skin, with no bleeding or ulceration at the moment of examination. The patient performed a dermatological consult which raised the suspicion of malignant melanoma(1).
Considering the history of the lesion, the patient was admitted into the hospital and after regular investigations performed (blood samples and EKG) he was planned for surgery.
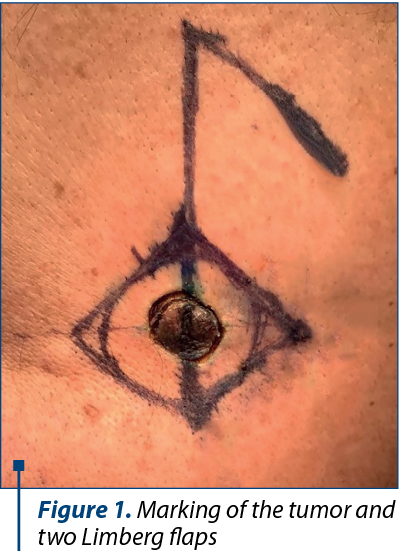
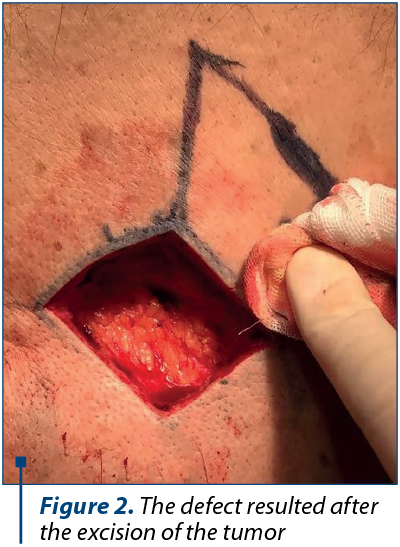
The operation implied a circular incision with the electric cautery followed by another incision placed on the exterior of the previous one performed with a scalpel, and the excision of the tumor with subcutaneous fat with a 20 mm margin (Figure 1 and Figure 2). The resulting defect was then covered by creating one local Limberg flap. After minutious haemostasis and adequate cleaning of the wound, the suture was performed in anatomical layers (Figure 4).

The following days the patient was assessed and dressings were performed daily. The evolution was favorable, with the wounds healing nicely, without any complication. On the third day, the patient was admitted out of the hospital with the recommendations of continuing the antibiotherapy, pain killers (if needed), and follow-up at 7 and 14 days.
The histopathology result 21 days after the operation confirmed the initial suspicion and elaborated the result of malignant melanoma with Clarck III and Breslow index >0.76 mm (~1.3 mm) and complete excision of the tumor.
Discussion
Malignant melanoma is not a rare disease in Romania. Being a serious disease, very aggressive and with potential of bad prognosis, it is of outmost importance that it is diagnosed as fast as possible, thus increasing the chances of survival(1).
Several studies have been performed on this subject, and in one of these, Osterlind found that some characteristics influence the evolution of the disease, with women and younger patients having better prognosis and survival rates than men and older people, and better localized tumors being less aggressive than the disseminated ones(1,2).
The patient from our study had a localized lesion in the instercapullary region, but had higher risk, being an older male. Also, malignant melanoma seems to be more frequent in whites, as well as in Africans and others(3,4).
An important aspect on this issue is the classification of the malignant melanoma. Several classifications for malignant melanomas have been described along the time, which include the Breslow, Clark and TNM classifications (the latter being the most elaborated of these). The more summarized versions are the first two, with Breslow indicating the depth of the lesion and offering a prediction of the future evolution, while Clark is used to describe mostly the thin forms of melanoma(5,6).
Breslow classification:
-
Thickness of 0.75 mm or less.
-
Thickness of 0.76-1.5 mm.
-
Thickness of 1.51-4 mm.
-
Thickness greater than 4 mm.
Clark classification:
-
Level I – involves only the epidermis (in situ melanoma).
-
Level II – invades papillary dermis, but not the papillary-reticular interface.
-
Level III – invades the papillary dermis up to the interface, but without the reticular dermis.
-
Level IV – invades the reticular dermis, but not the subcutaneous tissue.
-
Level V – invasion into the subcutaneous tissue.
Conclusions
Malignant melanoma is gaining a rapidly increasing incidence yearly worldwide. It remains an important and challenging problem because of the subclinical micrometastases that it may generate and which can affect the other organs at the same time in which the primary lesions is being treated. Hence the importance of clinical trials and screening in evading complications(1,6).
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Yagi KI, Wani HU, Tinguria MB, Al-Qahtani DM. Malignant melanoma of the skin: a case report from the Eastern region (Dammam Central Hospital), Saudi Arabia and epidemiological review. Journal of Family & Community Medicine. 2000; 7(2):67-71.
- Osterlind A, Kjems E. Survival of Danish Cancer Patients 1943-1987. Malignant Melanoma of the Skin. APMIS Suppl. 1993; 33:149-55.
- Katsambas A, Nicolaidou E. Cutaneous Malignant Melanoma and Sun Exposure Recent Developments in Epidemiology. Arch Dermatol. 1996; 132(4):444–50.
- Mason MD, Allman R, Quibell M. Adhesion Molecules in Melanoma – more than just superglue. J.R. Soc. Med. 1996; 89(7):393–5.
- American Joint Committee on Cancer. Malignant melanoma of the skin. American Joint Committee on Cancer: AJCC Cancer Staging Manual. 1997; 5th ed. Philadelphia, Pa: Lippincott-Raven; 163-70.
- Neligan CP. Plastic Surgery, 3rd edition. Elsevier Saunders, 2013.
Articole din ediţiile anterioare
Integrated Palliative Outcome Scale (iPOS) for the early detection of palliative care needs of cancer patients
În cadrul unui studiu prospectiv, a fost aplicat chestionarul iPOS la 103 pacienţi. Cu ajutorul întrebărilor la care au răspuns pacienţii, s-au i...
Screeningul naţional pentru cancerul de col uterin. Experienţă preliminară pentru screeningul cancerului de sân
Introducere. Cancerul de col uterin reprezintă o problemă de sănătate publică în România, anual fiind diagnosticate 4000 de femei şi înregistrate 2...
Combinaţie de agenţi imunoterapeutici utilizată în melanomul metastatic – prezentare de caz
Melanomul malign metastatic are un prognostic nefavorabil, cu o supravieţuire globală care până nu demult era de 8-12 luni. Actualmente, prin apari...
Prevenirea cancerului prin intermediul unor programe de screening
Prevenţia cancerului prin screening este o resursă importantă care ar trebui folosită judicios, în special prin programe de sănătate la nivel n...