Artificial intelligence (AI) is a fascinating field that has captured the attention of scientists and researchers. The definitions of AI have changed and evolved. The contemporary definition focuses on the ability of artificial systems to learn from data and perform specific tasks, such as voice and visual recognition or decision-making based on complex information. Artificial intelligence has evolved from rigidly programmed systems to ones that can learn and adapt autonomously. AI has represented a significant evolution in the medical field, bringing fundamental changes in disease diagnosis, treatment and management. There are several ways in which it can be used in pediatrics: assisted diagnosis and prognosis, designing personalized treatment regimens, real-time monitoring of patients, assistance in consultations and remote care, and medical education and training. Despite all the advantages that AI brings, doctors’ reluctance remains an important obstacle to its adoption. Concerns about the ethical and legal aspects of using AI in medical practice may drive this reluctance. Ethical and legal issues include patient data privacy, accountability, transparency of AI algorithms, and error detection. Clear regulations are needed to address these issues in medical practice. Artificial intelligence should not and will never replace the experience and expertise of doctors. AI in pediatrics should always complement doctors based on a multidisciplinary approach involving human medical consultation and decision-making in a wider context.
Introduction to the use of artificial intelligence in pediatrics
Introducere în utilizarea inteligenţei artificiale în pediatrie
First published: 30 iunie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Pedi.70.2.2023.8303
Abstract
Rezumat
Inteligenţa artificială (IA) reprezintă un domeniu fascinant, care a captat atenţia oamenilor de ştiinţă şi a cercetătorilor. Definiţiile IA s-au schimbat şi au evoluat de-a lungul timpului. Definiţia contemporană se concentrează pe capacitatea sistemelor artificiale de a învăţa din date şi de a realiza sarcini specifice, precum recunoaşterea vocală şi vizuală sau luarea deciziilor bazate pe informaţii complexe. Inteligenţa artificială a evoluat de la sistemele programate rigid la cele care pot învăţa şi se pot adapta în mod autonom. IA a reprezentat o evoluţie semnificativă în domeniul medical, aducând schimbări fundamentale în diagnosticul, tratamentul şi managementul bolilor. Există mai multe modalităţi în care IA poate fi utilizată în pediatrie: diagnosticul şi prognosticul asistat, proiectarea de scheme de tratament personalizate, monitorizarea în timp real a pacienţilor, asistenţă în consultaţii şi îngrijire la distanţă şi în educaţie medicală şi formare. Cu toate avantajele aduse de IA, reticenţa medicilor rămâne un obstacol important în adoptarea acesteia. Îngrijorările legate de aspectele etice şi legale privind utilizarea ei în practica medicală pot determina această reticenţă. Probleme etice şi legale includ confidenţialitatea datelor pacienţilor, responsabilitatea, transparenţa algoritmilor AI şi depistarea erorilor. Sunt necesare reglementări clare pentru a aborda aceste aspecte în practica medicală. Inteligenţa artificială nu trebuie şi nu va înlocui niciodată experienţa şi expertiza medicilor. Utilizarea IA în pediatrie ar trebui să fie întotdeauna complementară medicilor, să se bazeze pe o abordare multidisciplinară, implicând consultarea medicală umană şi luarea deciziilor într-un context mai larg
Definitions of artificial intelligence over time: an evolutionary perspective
Artificial intelligence (AI) is a fascinating field that has captured the attention of scientists and researchers. Definitions of AI have changed and evolved, reflecting both technological progress and researchers’ perspectives and concerns(1). Alan Turing’s idea in 1950 to use computers to simulate critical thinking was the primordial element of the existence of AI(2). From the initial definition proposed by McCarthy in 1955 to more recent approaches that emphasize machine learning and the ability of artificial systems to solve complex problems, the concept of artificial intelligence has become increasingly sophisticated. These definitions allow us to understand and appreciate the significant contributions of the field and assess the impact and prospects of AI in various areas of our lives.
The original classic definition was proposed by John McCarthy, who considered artificial intelligence to be “the science and engineering of creating intelligent machines and, in particular, intelligent computer programs. It is related to using computers to understand the mechanisms of human intelligence, but AI should not be limited to biologically observable and quantifiable methods”(3). This definition established the foundations of the study of artificial intelligence and paved the way for developing algorithms and intelligent systems(3).
In the 1960s, the definition of AI evolved towards a more behavior-centric approach. Allen Newell and Herbert Simon defined artificial intelligence as “the activity that aims to make machines behave in ways that, if done by humans, would be considered intelligent”(4). This definition emphasizes the importance of intelligent behavior within artificial systems.
In the 1980s, the definition of AI was expanded to include the cognitive approach and the concept of general artificial intelligence (GAI). GAI refers to artificial systems that can perform human intellectual tasks(5). This definition involves developing systems that can understand, learn and solve problems similarly to humans.
In Artificial Intelligence: A Modern Approach, Peter Norvig and Stuart Russell defined AI as “the study of agents that receive perceptions from the environment and, by analyzing them, manage to perform actions”(6). Patrick Winston considers artificial intelligence a set of “constraint-enabled algorithms, exposed through representations that support models that target loops that interconnect thought, perception, and response, respectively”(7).
The contemporary definition of AI has been adapted in the context of technological advances and the development of learning algorithms. There are several subsets of artificial intelligence, such as machine learning, structured deep learning, natural language processing, and computer vision. Machine learning refers to the ability of artificial intelligence to identify and analyze patterns, improving the experience based on data sets. Deep learning is related to the role of neural networks that allow AI to learn and make decisions independently. Natural language processing allows AI to take data from human language and make decisions based on this data. Computer vision represents the process by which artificial intelligence takes information and learns from analyzing sets of images and movies(2). The contemporary definition focuses on the ability of artificial systems to learn from data and perform specific tasks, such as voice and visual recognition or decision-making based on complex information. This highlights the evolution of the concept from rigidly programmed systems to those that can learn and adapt autonomously.
A brief history of AI in medicine
Artificial intelligence represents a significant evolution in the medical field, bringing fundamental changes in disease diagnosis, treatment and management. Over time, AI has enabled improved diagnostic accuracy, accelerated decision-making, and optimized patient care outcomes.
Pioneering AI in healthcare. In the 70s, the first applications of artificial intelligence in medicine were developed, emphasizing expert diagnostic systems. A notable example is the MYCIN system, developed at the Stanford University, which uses expert diagnostic rules to diagnose bacterial infections and recommend appropriate treatment(8).
With the advent of artificial neural networks in the 80s and 90s, AI began to tackle complex diagnostic problems. The introduction of deep neural networks has demonstrated their ability to recognize complex patterns in medical data(9). Thus, the way was opened for advanced applications of medical image recognition, such as cancer detection in mammographic imaging(10).
The advancement of technology and the increase in the amount of medical data available have allowed AI to evolve through data analysis and machine learning techniques. The emergence of deep learning algorithms has allowed remarkable achievements in diagnosing and prognosis medical conditions, such as the role of deep neural networks in dermatological classification with an accuracy similar to that of dermatology specialists(11).
Artificial intelligence has significantly developed personalized medicine, tailoring treatments and medical interventions to patients’ needs. Genetic and molecular data analysis applications have allowed the identification of prognostic markers for various conditions and the identification of appropriate patient treatments(12).
Virtual healthcare is another direction in which AI has brought significant medical advances. AI-based chatbots, virtual assistants and mobile applications enable patients to quickly access medical information, preliminary diagnosis and symptom management(13).
Possible use of AI in pediatrics
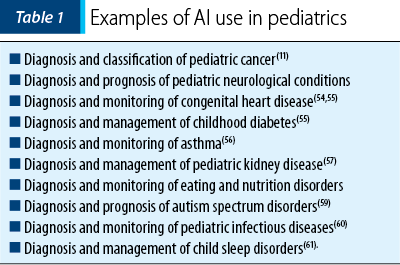
Artificial intelligence has significant potential in pediatrics, with the ability to improve diagnosis and treatment in children. There are several ways AI can be used in pediatrics; here are some examples.
AI-assisted diagnosis and prognosis in pediatrics is a burgeoning field with the potential to revolutionize children’s health care. By using machine learning algorithms and analyzing complex medical data, AI can support the early diagnosis of pediatric conditions and contribute to forecasting their evolution. AI can analyze medical data (medical history, lab results or images) to help diagnose and predict pediatric conditions. Thus, it can detect patterns and signals that may escape human observation and provide assistance in the rapid and accurate identification of specific diseases. Artificial intelligence can be trained to detect early signs of rare diseases or help diagnose chronic diseases.
AI-assisted diagnosis in pediatrics is achieved through the following steps:
- Collection and centralization of medical data from patients, parents, or electronic medical registration systems.
- Data preprocessing by standardizing and preparing it for analysis. It is necessary to remove errors or incomplete data and transform the data into a format suitable for AI algorithms.
- Training the AI algorithm (such as convolutional neural networks – CNNs, or decision trees) using reference data sets where for each case in the training data set, the correct diagnosis is known. The algorithm learns to recognize patterns and make correlations between input data and the correct diagnosis.
- Algorithm validation using a separate and independent validation data set that may contain new and unknown examples to evaluate the algorithm’s performance in correct diagnosis.
- Algorithm testing and evaluation are done on test datasets independent of those used in training and validation. The algorithm’s performance in AI-assisted diagnosis is compared with the diagnosis given by specialized doctors, analyzing the accuracy, sensitivity, specificity, or other relevant parameters.
- Implementation in clinical practice is done if the AI algorithm demonstrates sufficiently good performance in validation and testing. At this stage, the interaction between the algorithm and healthcare professionals is managed to use AI-assisted diagnosis in the decision-making process.
A crucial aspect of AI-assisted diagnosis is collecting and analyzing relevant medical data. By training a convolutional neural network on a large set of dermoscopic images, the AI achieved results comparable to those of professional dermatologists in classifying skin cancer. This approach could also be applied to diagnosing skin cancer in children, improving diagnostic accuracy and early interventions(11).
Regarding prediction, AI algorithms can analyze and interpret children’s clinical and genetic data to estimate the risk of developing certain conditions. Mollahosseini et al.(14) used convolutional neural networks to detect autism spectrum disorders in brain magnetic resonance images. This approach highlighted the potential of AI to provide early diagnosis and assessment of severity in children with autism, facilitating early and personalized interventions.
Artificial intelligence can improve the prediction of some conditions’ evolution by analyzing longitudinal clinical data and predictive models. Rajpurkar et al.(15) developed a convolutional neural network for diagnosing pneumonia on chest radiographs, which achieved results comparable to those of specialized radiologists, providing the opportunity to predict disease progression and assess response to treatment. Diagnosing and managing congenital heart disease in children can benefit from AI, facilitating a personalized and accurate approach to patients(16). Mental illnesses represent a significant challenge in pediatrics, and AI can be used in their detection and classification to support early diagnosis and intervention(17).
The design of personalized treatment schemes is crucial in ensuring adequate care tailored to the needs of each child. AI offers significant opportunities, contributing to the development of personalized treatment approaches based on medical data and patient information. AI can consider individual factors (weight, age, medical history and allergies) to recommend effective and safe treatments.
Collecting and analyzing relevant medical data play an essential role in the design of personalized treatment regimens. Perer et al.(18) evaluated data analysis approaches, such as data mining and identifying relevant patterns in clinical data. An important aspect is integrating children’s clinical and genetic data to identify prognostic markers for various pediatric conditions(19).
Individualization of drug doses is an essential aspect of pediatric treatment. AI can help determine the optimal dose of drugs according to the individual characteristics of the child, such as in the pediatric treatment of hypertension(20). Sherwin et al.(21) highlight the use of AI in pharmacokinetic and pharmacodynamic modeling in pediatrics, contributing to the optimization of treatment and the minimization of side effects, being able to predict a child’s response to administered drugs. Artificial intelligence can help identify children at increased risk of adverse drug reactions(22). Wang et al.(23) evaluated the use of AI in pediatric pharmacogenetic modeling and its implications for designing personalized treatment regimens. Pharmacogenetics is essential for understanding individual drug responses by identifying genetic variants relevant to treatment response.
Designing personalized radiation therapy regimens in pediatric oncology is particularly important; AI can help identify target areas and optimize radiation doses(24). The role of AI in the management of pediatric diabetes, including continuous monitoring of blood glucose and adaptation of insulin doses according to the individual needs of children, was demonstrated by Li et al.(25) In the case of rare diseases, designing personalized treatment regimens can be difficult due to lack of data and limited experience. Artificial intelligence may represent the solution(26-28).
Real-time patient monitoring in pediatrics is crucial to ensure effective and safe care. It can be done with the help of AI, tracking children’s vital signs, such as heart rate, blood pressure and blood oxygen levels(29). AI can detect abnormal variations or deterioration in a child’s health in intensive care units and alert medical staff for immediate intervention before severe complications occur(30).
Artificial intelligence can be helpful in noninvasive monitoring of glucose levels in the child, using techniques such as infrared spectroscopy and spectroscopic data analysis to obtain accurate measurements(31). Another application of AI may be in analyzing electroencephalographic (EEG) signals to help diagnose and monitor epilepsy in children(32). The evaluation of medical images (chest radiographs and ultrasounds) can provide crucial information about the condition of pediatric patients, helping to identify and diagnose some conditions in real time(33). Children with developmental disorders may benefit from real-time behavioral monitoring and assessment(34). AI-assisted monitoring of respiratory parameters can be crucial in managing respiratory conditions in children(35), providing essential information for medical decision-making. Using algorithms to recognize facial expressions and physiological signals with the help of AI, pain can be identified and quantified(36).
Artificial intelligence can be extensively integrated into the pediatric healthcare system, connecting electronic health record systems, monitoring systems, and medical devices to improve workflow and provide coordinated care(37).
Consultation assistance and remote care. Artificial intelligence can help interpret symptoms, provide information about treatments, and guide parents in correctly administering medications. When physical access to medical services is limited, AI can assist in telemedicine and remote medical consultation(12,35,38). Through chatbots or virtual assistants, AI can answer questions from patients and parents, provide information about conditions and treatments, and guide the administration of the correct medications. AI can help monitor pediatric patients’ vital parameters and physiological signs, facilitating prompt intervention and preventing complications. Effective doctor-patient communication is essential in remote consultations, and AI can support this process(39).
Medical education and training. Artificial intelligence can be used to develop interactive modules and simulations that help students and residents learn about pediatric diseases and diagnostic and treatment strategies. Medical simulation provides a safe and realistic environment for pediatricians to learn and train. AI can bring complex and personalized scenarios to develop clinical skills(40,41). Virtual and augmented reality can bring interactive and immersive learning experiences for pediatricians, such as virtual simulations, three-dimensional visualization of anatomy, and virtual clinical practice(42). Artificial intelligence can also be used to develop systems for automatic and objective assessment of medical knowledge(43). Personalized learning is essential to optimizing the pediatric training process. Artificial intelligence can be used to tailor educational materials and learning strategies to the individual needs of pediatricians(44).
Simulating doctor-patient interactions is important in training communication and relationship skills in pediatrics. Artificial intelligence can create realistic and interactive simulation scenarios, allowing pediatricians to practice and develop communication skills or social-emotional competencies(45).
The ethical challenges of AI in pediatrics
The use of artificial intelligence involves the collection and analysis of large amounts of personal patient data, including sensitive medical information. Protecting privacy and applying patient data protection standards are essential(46).
As AI algorithms make critical patient decisions, responsibility and accountability become key issues. It is necessary to identify and establish who is responsible for the decisions made by the algorithms and how they can be challenged or monitored. Mittelstadt et al.(47) present several aspects of ethical responsibility in the context of AI relevant in pediatrics.
Ethical responsibility requires that AI algorithms be transparent and explained so that how they reach their conclusions can be understood and their correctness and fairness can be verified. This is essential to gain the trust of physicians and avoid unwanted biases or systematic errors(29).
Ethical responsibility in AI involves ensuring justice and fairness in automated processes and decisions. AI algorithms must be trained on representative data and be sensitive to population diversity to avoid discrimination or inequities in diagnosis and treatment. Ensuring fair accuracy and impartiality is essential in the pediatric context(47).
Decisional responsibility. Although AI algorithms can assist in decision-making, physicians are responsible for interpreting algorithm-generated results and making informed and ethical decisions in patient care. AI algorithms should be supportive tools, not replace human medical responsibility and expertise(47).
AI algorithms are not immune to errors and may have limitations. Ethical accountability involves detecting and managing errors in a transparent and accountable manner. Developing appropriate mechanisms for monitoring and evaluating algorithms’ performance and correcting and updating them according to clinical feedback and new scientific findings are essential. Physicians’ reluctance or distrust of the results of AI algorithms may be influenced by errors in the algorithms or by the difficulty of understanding how they reached their conclusions(47).
The use of artificial intelligence in pediatrics raises questions regarding the professional responsibility of doctors and the risk of being replaced by algorithms. It is essential to clearly define the physician’s role in the decision-making process and ensure that AI is a supportive tool, and not a substitute for the physician. Professional responsibility also involves proper oversight of AI technologies used in medical practice. Physicians must be involved in developing, validating and updating AI algorithms to ensure they are accurate, safe and appropriate for their patients. There also needs accountability in identifying and addressing potential ethical, legal or security issues associated with using AI in medicine(48).
Influence on communication and the doctor-patient relationship. It is essential that physicians maintain their role as primary communicators with patients and clearly explain how AI is being used in their care. Transparency and clarity in communication are essential to avoid confusion and build patient confidence in using AI(47).
Physicians’ reluctance to use artificial intelligence in medical practice
The use of artificial intelligence in medicine has a significant potential for improving diagnosis, treatment and patient management. However, physicians’ reluctance to adopt AI remains a significant obstacle for several reasons. Physicians may be reluctant due to several concerns regarding ethical and legal aspects of using AI in medical practice. These concerns include the privacy of patient data, accountability and transparency of AI algorithms. Clear guidelines and regulations are needed to address these issues(49). Doctors may be reluctant to use artificial intelligence if they do not clearly understand how the algorithms work and do not trust their accuracy. Thus, transparency and understanding in implementing and using AI in medical practice are emphasized(50). The doctor-patient relationship is essential in healthcare, and AI can raise concerns about losing human interaction and personalization in healthcare. Integrating artificial intelligence into medical practice must be done to complement and enhance the doctor-patient relationship(12).
How can we overcome the obstacles and reluctance of doctors? Providing adequate medical training in AI can help doctors understand and correctly use this technology. Integration of AI into continuing medical education programs is needed(1,51). Collaboration and involvement of physicians in developing and implementing AI can increase their confidence and acceptance. Collaboration between medical professionals and researchers in developing AI systems in medicine is essential(52). Some universities have introduced new programs to educate medical engineering professionals who, based on clinical experience and digital expertise, can solve modern medicine’s new problems(62). Responsible and ethical implementation of AI in medical practice can help earn the trust of doctors. Compliance with ethical principles of transparency and accountability in AI implementation is essential(53,62). With adequate support, under the conditions of future technological development with new AI models, and with an appropriate legislative framework, doctors can become key partners in AI’s responsible and effective use in ensuring optimal patient management(63).
It is important to note that, despite its potential, AI does not and will never replace the experience and expertise of physicians(47,62). AI in pediatrics should always be complementary to doctors, based on a multidisciplinary approach, which also involves human medical consultation and decision-making in a broader context. Artificial intelligence must be integrated into an ethical and legal framework, respecting data privacy and ensuring effective collaboration between healthcare professionals and AI technology.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.

Bibliografie
- Knake LA. Artificial inteligence in pediatrics: the future is now. Pediatric Research. 2023;93:445-446.
- Kaul V, Enslin S, Gross SA. History of artificial intelligence in medicine. Gastrointestinal Endoscopy. 2020;92(4):807-12.
- McCarthy J, Minsky ML, Rochester N, Shannon CE. A proposal for the Dartmouth summer research project on artificial intelligence. AI Magazine. 1995;27(4):12-14.
- Newell A, Simon HA. Computer science as empirical inquiry: symbols and search. Communications of the ACM. 1976;19(3):113-126.
- Nilsson NJ. Artificial intelligence: A new synthesis. Morgan Kaufmann, 1998.
- Norvig P, Russell S. Artificial Intelligence: A Modern Approach. Prentice Hall, 1995.
- Winston PH. Artificial Intelligence. 2nd Ed. Addison-Wesley Publishing Company, 1977.
- Shortliffe, EH, Buchanan BG, Feigenbaum EA. Rule-based expert systems: The MYCIN experiments of the Stanford Heuristic Programming Project. Addison-Wesley, 1975.
- Rumelhart DE, Hinton GE, Williams RJ. Learning representations by back-propagating errors. Nature. 1986;323(6088):533-536.
- LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 1998;521(7553):436-444.
- Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks [published correction appears in Nature. 2017 Jun 28;546(7660):686]. Nature. 2017;542(7639):115-118.
- Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44-56.
- Denecke K, Bamidis P, Bond C, et al. Ethical Issues of Social Media Usage in Healthcare. Yearb Med Inform. 2015;10(1):137-147.
- Mollahosseini A, Hasani B, Mahoor MH. Feeding alexnet with anatomical signatures for autism spectrum disorder detection: A framework for analysis of brain imaging data. IEEE Transactions on Cognitive and Developmental Systems. 2017;10(4):1004-1013.
- Rajpurkar P, Irvin J, Zhu K, Yang B, Mehta H, Duan T, Ng A. CheXNet: Radiologist-level pneumonia detection on chest X-rays with deep learning. arXiv. 2017;arXiv:1711.05225.
- Majumder A, Abidin NS, Azman W, Kassim AM, Mahayiddin AA, Ariffin AF, Hassan AA. Artificial intelligence applications in pediatric congenital heart disease. Journal of Clinical Medicine. 2020;9(3):637.
- Pestian JP, Matykiewicz P, Grupp-Phelan J, Linn-Gust M, South B. Applications of natural language processing and machine learning in pediatric psychiatry. Journal of the American Academy of Child & Adolescent Psychiatry. 2019;58(2):120-128.
- Perer A, Wang F, Hu J. Mining treatment history of patients for clinical research. ACM Transactions on Intelligent Systems and Technology. 2014;5(4):1-27.
- Zeng J, Cai Y, Yang G, Zhang Z, Cui Q. Integrating multi-omics data for discovery of personalized treatment biomarkers in pediatric cancers. BMC Genomics. 2015;16(Suppl 7):S2.
- Alshamsi S, Almaghrabi H, Alnafisah A, Alghamdi M, Aljuhani S. Personalization of pediatric hypertension treatment using artificial intelligence. Saudi Journal of Kidney Diseases and Transplantation. 2020;31(4):748-756.
- Sherwin CMT, Baluom M, Brennan C, Brundage RC. Applications of artificial intelligence for pediatric pharmacokinetics and pharmacodynamics: A scoping review. Clinical Pharmacology & Therapeutics. 2020;108(5):989-1004.
- Bernarde C, Calmels MN, Molimard M, Morisset J, Escudier B. Artificial intelligence to detect severe adverse drug reactions in oncology. Journal of Clinical Medicine. 2020;9(8):2570.
- Wang J, Chen R, Chen L, Cai Y. Artificial intelligence in pediatric pharmacogenomics: Challenges and perspectives. World Journal of Pediatrics. 2020;16(5):438-444.
- Shiraishi J, Inoue M, Sato M, Hiraoka M, Nakamura K. Artificial intelligence for treatment planning in pediatric radiation oncology: A scoping review. Cancer Medicine. 2021;10(8):2622-2634.
- Li X, Xu Z, Xiao J, Zhang M, Li Q, Chen S. Artificial intelligence-based system for personalized glucose prediction and insulin dosage adjustment: An application of closed-loop insulin delivery for type 1 diabetes management. Diabetes Therapy. 2019;10(3):1023-1033.
- Kourou K, Exarchos TP, Exarchos KP, Karamouzis MV, Fotiadis DI. Machine learning applications in cancer prognosis and prediction. Computational and structural biotechnology Journal. 2015;13:8-17.
- Bombaci M, Sorrentino R, Vitiello F. Artificial intelligence for precision medicine in pediatric cancer. Frontiers in Pediatrics. 2019;7:260.
- Salpietro V, Ruggieri M, D’Amico A, Zappia M. Artificial intelligence and rare pediatric diseases: A bibliometric analysis and systematic review. International Journal of Molecular Sciences. 2021;22(7):3785.
- Rajkomar A, Oren E, Chen K, et al. Scalable and accurate deep learning with electronic health records. NPJ Digit Med. 2018;1:18.
- Hsieh CH, Chang CJ, Hsiao YT, Wu TY, Li CH. Early warning score with machine learning to predict septic shock in the emergency department. Journal of Clinical Medicine. 2020;9(5):1333.
- Quah AL, Heng LX, Goh YL. Artificial intelligence in non-invasive glucose monitoring for pediatric diabetes management. Sensors. 2021;21(10):3396.
- Acharya UR, Oh SL, Hagiwara Y, Tan JH, Adeli H. Deep convolutional neural network for the automated detection and diagnosis of seizure using EEG signals. Comput Biol Med. 2018;100:270-278.
- McKinney SM, Sieniek M, Godbole V, et al. International evaluation of an AI system for breast cancer screening [published correction appears in Nature. 2020 Oct;586(7829):E19]. Nature. 2020;577(7788):89-94.
- Courchesne E, Pramparo T, Gazestani VH, Lombardo MV, Pierce K, Lewis NE. The ASD Living Biology: from cell proliferation to clinical phenotype. Mol Psychiatry. 2019;24(1):88-107.
- Nemati S, Holder A, Razmi F, Stanley MD, Clifford GD, Buchman TG. An Interpretable Machine Learning Model for Accurate Prediction of Sepsis in the ICU. Crit Care Med. 2018;46(4):547-553.
- Holsti L, Oberlander TF, Brant R, Stenstrom R. Pain in nonverbal children with medical problems: A content analysis of pain diaries and interviews. Journal of Pediatric Psychology. 2019;44(8):959-968.
- Obermeyer Z, Emanuel EJ, Schwartzstein RM. Machine learning in medicine. New England Journal of Medicine. 2019;380(14):1347-1358.
- Paranjape K, Schinkel M, Nannan Panday RS, Car J, Nanayakkara P. The Digital Health Evidence Consortium. Interventions by healthcare professionals to improve management of noncommunicable diseases in children in low- and middle-income countries: A systematic review. BMJ Global Health. 2020;5(8):e002084.
- Coravos A, Khozin S, Mandl KD. Developing and adopting safe and effective digital biomarkers to improve patient outcomes. NPJ Digital Medicine. 2019;2(1):1-4.
- Cheng A, Nadkarni VM, Mink R, Kessler D, Vetterly C, Saville B, Schiavenato M. E-learning improves pediatric residents’ acute care skills. Pediatric Critical Care Medicine. 2019;20(9):835-842.
- Gallego JC, Moreno-Ger P, Fernández-Manjón B. Analytics on medical education big data using multilayer clustering for providing feedback and recommendations. Sensors. 2020;20(8):2292.
- Chirico A, Lucidi F, De Laurentiis M, Milanese C, Napoli A, Giordano A. Virtual Reality in Health System: Beyond Entertainment. A Mini-Review on the Efficacy of VR During Cancer Treatment. J Cell Physiol. 2016;231(2):275-287.
- Onishi H, Tsutsui S, Furukawa TA, Oki T, Okamoto K. Computer-based assessment of clinical skills for pediatric residents. Pediatrics International. 2018;60(10):947-953.
- Jena S, Jamatia A, Bhattacharya U. An AI-based learning system for personalized learning: Architecture, application, and impact analysis. Journal of Educational Technology & Society. 2020;23(3):127-139.
- Cheng A, Hunt EA, Grant D, Lin Y, Grant V, Hecker K, Kessler D. Virtual patient simulation improves patient-physician communication skills in pediatric residents. Pediatrics. 2021;147(4):e2020024542.
- Celi LA, Davidzon G, Johnson AE, Komorowski M, Marshall DC, Nair SS, Paik KE. Bridging the artificial intelligence and clinical worlds: A roadmap for effective collaboration. Critical Care Medicine. 2020;48(9):1289-1296.
- Mittelstadt BD, Allo P, Taddeo M, Wachter S, Floridi L. The ethics of algorithms: Mapping the debate. Big Data & Society. 2019;6(2):2053951719848263.
- Emanuel EJ, Wachter RM, Krumholz HM. Artificial intelligence in health care: Will the value match the hype? JAMA. 2019;321(23):2281-2282.
- Ong JC, Geifman N, Chokshi S, Patil S. Ethical implications of artificial intelligence in health care. JAMA. 2018;320(23):2413-2414.
- Lee KC, Hsieh WL. Physicians’ perspectives on artificial intelligence-based pathology: a survey of the pathologists in Taiwan. Journal of Pathology Informatics. 2019;10:9.
- Sockolow P, Rodakowski J. AI in healthcare education: Making technology work for learners and teachers. MedEdPublish. 2019;8(1):1-11.
- Nguyen TD, Tran TN, Pham TH, Pham HT. Artificial intelligence in medicine: current opportunities and issues on its adoption in healthcare. In: Proceedings of the 11th International Conference on Knowledge and Systems Engineering. 2019; pp. 7-12.
- Gong K, Xu Z, Chen Y, Li Z, Bai W, Zhu Y. Ethical implications of artificial intelligence in medical imaging: A systematic review. European Journal of Radiology. 2020;124:108770.
- Wang S, Summers RM, Raghavan V. Deep learning for robust segmentation of noisy medical images. Annals of Biomedical Engineering. 2017;45(7):1605-1617.
- Inan OT, Haritos T, Sulemanji M. Use of artificial intelligence in the care of children with congenital heart disease in the era of home monitoring. Progress in Pediatric Cardiology. 2020;58:101265.
- Schiekofer S, Beyerlein A. An introduction to deep learning for the pediatric endocrinologist. Pediatric Endocrinology Reviews. 2018;16(Suppl. 1):140-144.
- Basheti IA, Qunaibi E, Aburuz S. Predictive modeling of asthma exacerbations in pediatric patients using machine learning techniques. Respiratory Care. 2019;64(6):691-701.
- Dreyer G, Reid S. Artificial intelligence in pediatric radiology: Recent advances and future directions. Pediatric Radiology. 2019;49(2):143-150.
- Klironomos S, Karantanos T, Politou M. Artificial intelligence in pediatric gastroenterology: Recent advances and future perspectives. World Journal of Gastroenterology. 2020;26(36):5427-5439.
- Kassahun Y, Solla ED. Machine learning approach to autism classification based on resting-state EEG connectivity. Frontiers in Neuroinformatics. 2019;13:11.
- Perez EM, Madeira MR, Nery JS, Santana MA, Ferreira D. Detection of pneumonia using machine learning models: Systematic review and meta-analysis. PloS One. 2020;15(2):e0229383.
- Gozal D. Artificial intelligence in pediatric sleep medicine. Sleep Medicine Clinics. 2019;14(4):463-473.
- Briganti G, Le Moine O. Artificial Intelligence in Medicine: Today and Tomorrow. Front Med (Lausanne). 2020;7:27.
- Li YW, Liu F, Zhang TN, Xu F, Gao YC, Wu T. Artificial intelligence in pediatrics. Chinese Medical Journal. 2020;133(3):358-360.
Articole din ediţiile anterioare
Actualităţi în diagnosticul hepatitei autoimune la copil
Tipurile de boli hepatice autoimune recunoscute la populaţia pediatrică sunt: hepatita autoimună (AIH), colangita sclerozantă autoimună (...
Consangvinitatea − la limita dintre etic şi patologic
Căsătoriile consangvine sunt definite ca fiind acele căsătorii în care partenerii au un ascendent comun. Consangvinitatea pune probleme atât de ...
Neuropsihiatria pediatrică dintr-o privire. O boală rară, ca o condamnare: sindromul Pitt-Hopkins
Sindromul Pitt-Hopkins reprezintă o afectare genetică mai puţin dezbătută în literatura de specialitate de la noi şi chiar şi din străinătate. Cu ...