Substance use disorder is frequent in patients with schizophrenia and dramatically worsens their outcome. A series of theories have been advanced to explain the frequent associations between substance use disorder and schizophrenia. Several groups have proposed substance abuse as a trigger factor for the onset of schizophrenia in vulnerable individuals. On the other hand, personality traits such as dissocial or borderline can constitute an interface between psychotic disorder and excessive use of both legal and illegal psychoactive substances. Some reports suggest that patients with schizophrenia and a history of substance use can have an earlier onset age for schizophrenia. In addition, most investigators report that schizophrenia patients experiment negative effects after using even small amounts of psychoactive substances. Therefore, we present the case of a 28-year-old male with a long history of psychoactive substance use and early presentations in the pediatric neuropsychiatry outpatient department.
Asocierea dintre uzul mai multor substanţe psihoactive şi schizofrenie –management farmacologic şi psihoterapeutic
Association between multiple psychoactive substance use and schizophrenia – pharmacological and psychotherapeutic management
First published: 29 noiembrie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Psih.75.4.2023.8929
Abstract
Rezumat
Tulburarea consumului de substanţe este frecventă la pacienţii cu schizofrenie şi agravează dramatic prognosticul acestora. Au fost propuse o serie de teorii pentru a explica asocierea frecventă dintre tulburarea consumului de substanţe şi schizofrenie. Mai multe grupuri au propus ca factor declanşator consumul de substanţe în apariţia schizofreniei la persoanele vulnerabile. Pe de altă parte, trăsături de personalitate precum cele disociale sau borderline pot constitui o interfaţă între tulburarea psihotică şi consumul excesiv de substanţe psihoactive licite şi ilicite. Există o serie de rapoarte care sugerează că pacienţii cu schizofrenie şi istoric de consum de substanţe pot avea o vârstă precoce de debut a bolii. În plus, majoritatea investigatorilor raportează că pacienţii cu schizofrenie experimentează efecte negative în urma utilizării chiar şi a unor cantităţi mici de substanţă. Astfel, prezentăm cazul unui bărbat de 28 de ani, cu o lungă istorie de consum de substanţe psihoactive şi prezentare precoce în ambulatoriul Clinicii de Neuropsihiatrie Infantilă.
Introduction
Schizophrenia is a chronic illness characterized by hallucinations, delusions, disorganized thinking or behavior and associated disability, that occurs in approximately 1% of the population worldwide. Nearly 50% of people with schizophrenia, including those within their first episode (usually occurring in late adolescence or early adulthood), have a lifetime history of substance use disorder, a rate at least three times as high as seen in the general population(1). Alcohol, cannabis and cocaine tend to be the primary substances of abuse. In addition, 70% to 90% of patients with schizophrenia smoke cigarettes, as compared to approximately 21% of the people within the general population(2).
Case presentation
A 28-year-old Caucasian male, with a long history of consultations in the neuropsychiatry ambulatory, starting at the age of 6 years old, was brought by his parents to the emergency department of the Timişoara Psychiatry Clinic for a discordant psychopathologic panel dominated by psychotic symptoms with psychomotor agitation secondary to delirious-hallucinatory experiences, psychotic anxiety, verbal, thinking and behavioral disorganization and influence and passivity. He was hospitalized with the diagnosis of other acute and transitory psychotic disorders, and in 72 hours, based on the disease history and the ICD-10 criteria, the diagnosis of paranoid schizophrenia was established.
From the family history, we retain: mother – essential hypertension, type 2 diabetes; paternal grandmother – schizophrenia.
From his medical and psychiatric history, with clinical relevance, we retain that the patient was diagnosed at the age of 6 years old with hyperkinetic disorder with attention deficit (ADHD), at the age of 22, a pineal gland cystic formation was identified on an MRI, and at the age of 23, he was diagnosed with Graves-Basedow disease. As secondary psychiatric diagnostics, we retain: mixed and other personality disorders (emotionally unstable, impulsive, and borderline); mental and behavior disorders due to multiple drug use and use of other psychoactive substances, harmful use.
Life and work conditions: affirmatively, the patient lived in an urban area, with his parents, in adequate conditions. We mention that he was currently unemployed and he had never worked.
Behavior: smoker – 20 cigarettes per day, psychoactive substances – cannabis 1 g/day (affirmatively, from the age of 14 years old, reaching a consumption of 1 g/day from the age of 25 which continues in the present); speed – once a month; designer drugs – occasionally; alcohol – occasionally; coffee – occasionally (based on the report from the patient).
Clinical exam: in normal limits and no relevant clinical alterations were highlighted. We mention a BMI of 16.2; blood pressure 121/77 mmHg, HR 89b /min, and temperature 36.2 ºC.
The following psychometric scales were applied: PANSS Scale, T=110 (P=38, N=22, G=50), SCL-90 scale with elevated indexes for psychosis and paranoid thoughts; the word association test highlighted poor idea association, proverb familiarity – deficient abstract thinking; PAS scale – emotionally unstable personality disorder (impulsive and borderline) and accentuated personality traits type dissocial and schizoid.
Psychodiagnostic examination: “person with psychoactive immaturity, selective social contact with isolation and muster, affective lability, possible tendencies for thymic oscillations, need for recognition. Signs of mixed mood alterations with psychotic elements. There are no clear signs of organic affection”.
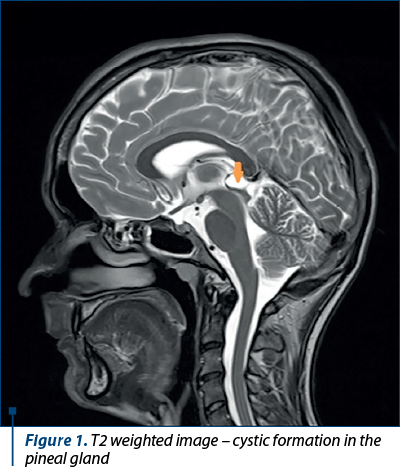
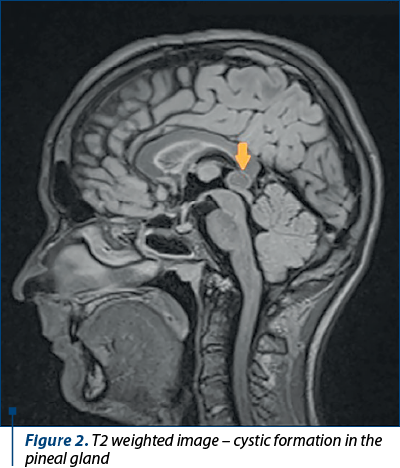
MRI – skull with contrast
The MRI of the skull with contract revealed round, smooth-edged, low protein content formation with homogeneous signal situated in the pineal cyst, with peripheral rim enhancement in contract imaging, with 1.66/1.3/2 cm (Figure 1, Figure 2 – T2 weighted image)
Disease history. The patient was first admitted to the pediatric neuropsychiatry specialty outpatient department with the diagnosis of hyperkinetic disorder with attention deficit, for which he received treatment that he didn’t take, following the will of his parents. At 14 years old, he started the use of psychoactive substances which constantly increased in frequency and intensity, reaching approximately 1 g/day of marijuana at the age of 25 and, occasionally, speed and designer drugs. From the anamnestic and heteroanamnestic data, we can trace back a possible onset even from the age of 14 years old and duration of untreated psychosis of around one year, anterior to the current admission in the hospital.
Psychic examination
Patient in negligent hospital attire, partially preserved body and clothing hygiene, temporally-spatially oriented, situational, auto- and allopsychic, clear field of consciousness. Mental contact is established relatively easily, but most of the time it shows an uncooperative attitude towards the medical staff. Eye contact is relatively maintained with the examining physician throughout the interview.
-
Mimic-gestural expressiveness: hyperexpressiveness, frequent grimaces, ample gestures sometimes having a bizarre character.
-
Attention: hypoprosexia of concentration and persistence, selective attention disorders.
-
Memory: fixation and evocation hypomnesia.
-
Perception: elementary auditory hallucinations (“Dad laughs in my right ear”); complex auditory hallucinations; comments (“I hear my mother in my left ear talking about me”); imperatives (“run away, run away”); kinesthetic hallucinations (“I feel two-way energy in the back”); interoceptive hallucinations (“I’ve had a stomach ache for two years”, “I feel pressure in my lungs”); visual illusions (“the salon colleague is a bigger demon and the other colleague is a smaller demon”).
-
Thinking: slightly accelerated ideo-verbal flow, tachypsychia; abstraction disorders with a tendency to hyperconcrete thinking, relaxation of associations of ideas with circumstantial, tangential and digressive thinking; disordered contents of thought – multiple delusional ideas with a paranoid theme, poorly systematized and bizarrely non-plausible, sensitive-relational (“Everywhere I go, people look at me like a stranger and always talk about me, they gossip”), pursuit (“I feel like someone is following me, some kind of cult, tech-savvy organization”), persecution (“I was photographed on the street and these pictures can hurt me”, “I know what I have to do in the future, I have to reveal the truth, I can bring out the positive energy because I connect on low frequencies with the collective voices in my head; I felt like I am sent by the source; I have a blueprint for anything”); ideas of transparency of thought and xenopathic influence (“These organizations know my thoughts; there is a programmer who directs me and others”).
-
Executive dysfunctions: difficulties in organizing, solving problems, sequencing and prioritizing complex activities and lack of working memory.
-
Behavior: psychomotor agitation; hallucinatory-delusional motivated behavior; verbal heteroaggression towards medical staff; clastic behavior; soliloquy; increased vital energy; suspicion; irascibility; hostility; rapes/bursts of self-aggression and physical and verbal heteroaggression towards the family at home; verbal aggression towards medical staff; impulsivity; compelling craving to use psychoactive substances (“craving”) followed by compulsive substance use; marked social withdrawal.
-
Conative-volitional level: lack of spontaneity, interests and curiosity; reduction of goal-oriented behaviors (apathetic syndrome), with the restriction of the general level of activity to instinctively and hedonically motivated behaviors.
-
Affect: dysphoric mood; emotional inversion towards the family; anxiety secondary to hallucinatory-delusional feelings; irritability; low tolerance for frustration.
-
Appetite: slightly increased;
-
Nictemeral rhythm: mixed insomnia
-
Insight: absent.
We support our diagnosis based on the history of the disease, the psychiatric exam, the psychodiagnostic exam, psychometric scale and ICD-10 criteria: influence and passivity, imperative, appellative and commentary hallucinations, persistent delusional ideas of all types, persistent hallucinations of all types, followed by temporary delusional ideas. Incoherence, irrelevant talking, neologisms due to alterations and interruptions in the train of thought. Time criterion is met for more than one month. We support the diagnosis of paranoid schizophrenia (F20.0). We support the diagnosis of mixed personality disorder (emotionally unstable, type impulsive and borderline) F61: marked tendency to act impulsively, without regard to consequences, affective instability with behavioral explosions, and lack of impulsion control, inner void/emptiness sensation. We support the diagnosis of mental and behavior disorder due to multiple drug use and use of other psychoactive substances, harmful use (F19.1): pattern of multiple psychoactive substance use, which affects the health at the mental and somatic level.(3)
We conducted the differential diagnosis with the following disorders: psychotic disorder with delusions due to unknown physiological conditions/organic mental disorder (tumor-induced, stroke etc.) – the MRI didn’t highlight alterations to support this diagnosis. Schizoaffective disorder – for diagnosis, we need a period of a major depressive episode (or manic episode) to coexist with schizophrenia symptoms, and there must be a period of at least two weeks in which schizophrenia symptoms manifest and the affective ones are diminished or absent. Schizophrenia-like psychotic disorder induced by psychoactive substances – in this situation, diverse psychotic symptoms are limited to the use or withdrawal from psychoactive substances, and there is also a period of six months of abstinence in which the symptoms disappear. Severe depression episode with psychotic symptoms – psychotic symptoms are transient and limited to the duration of the affective episode. Manic episode with psychotic symptoms (hallucinations and delusions are developed in the context of the affective disorder and they don’t persist). Persistent delusional disorder – it is defined by the presence of delusions and the absence of hallucinations. Acute and transient psychotic disorder – it doesn’t last more than one month. Schizotypal disorder – it presents a pattern of social and interpersonal deficits, marked by acute discomfort in close relationships, as well as cognitive and perceptual distortions and behavior eccentricity which usually appear during teenage years and tend to constantly manifest over a long time. Simple schizophrenia – negative symptoms without a history of positive symptoms.
During his admission, the patient received psychopharmacological treatment with: injectable haloperidol for psychomotor agitation control, Romparkin® 6 mg/day, initial oral treatment with paliperidone 12 mg/day, continued after clinical stabilization with Xeplion® 150 mg i.m. (long-lasting injectable formula of paliperidone) first dose, followed by the next dose on the 8th day of treatment. He will later receive monthly injections of 150 mg Xeplion® i.m., Orfiril Long® 1000 mg/day, Diazepam® 10 mg/day, Neurotop® 600 mg/day and Imovane® 7.5 mg/day when needed.
Besides pharmacological treatment, which is the base of the treatment of schizophrenia, psychotherapy offers the needed emotional support in managing the structural and the psychosocial deficits characteristic of the disease. Vocational rehabilitation, occupational therapy, music therapy and art therapy play an essential role in the evolution of schizophrenia patients. Dialectic behavioral therapy is considered the gold standard in the treatment of patients with borderline personality. Supportive therapy and psychoeducation are necessary for knowing the disease and for the early recognition of the signs that may announce a new episode.
Complications
Medication: extrapyramidal syndrome (acute dystonia, akathisia, parkinsonism, tardive dystonia), life-threatening neuroleptic malignant syndrome, hyperprolactinemia (amenorrhea-galactorrhea syndrome in women and gynecomastia in men, sexual dysfunction), metabolic syndrome (obesity, dyslipidemia, high waist circumference), hematological (clozapine can determine agranulocytosis.
Chronic: due to unhealthy behaviors (excessive smoking and the use of psychoactive substances) and also due to group genetic vulnerability, schizophrenia patients often develop cardiovascular, respiratory and metabolic complications.
Psychiatric: anxiety, depression, mania, suicide risk (50% of schizophrenia patients have a suicide attempt, and 10-15% achieve suicide).
Social: decreased quality of life, social withdrawal, family relations dysfunctions (leading to separations, divorce) social support network reduction, loss of productivity with early disease-based retirement, occasional dissocial behavior. The stigmatization issue is very important for these patients, who are often marginalized by society and therefore have much more reduced access to health services in general, as well as social services with consecutive life expectancy repercussions.
Short-term evolution: under drug treatment, the evolution can be favorable, with the remission of most positive symptoms, but with the partial persistence of cognitive and negative symptoms, especially due to poor adherence to psychopharmacological and psychotherapeutic treatment. The long-term evolution is often prolonged and episode-like, dotted by acute episodes with active symptoms which are intertwined with partial remission episodes, with the persistence of residual symptoms which confer the debilitating aspect of this disease.
The natural evolution of the disease: with the progression of the disease, acute episodes get longer and more frequent, detrimental to the remission episodes which get shorter, poorer and weaker in quality; sometimes, the evolution can be chronic from the debut of the disease up until the end of the patients’ life.
Regarding prognostic, the balance is partially aligned, managing to identify negative prognostic factors (male gender, psychoactive substance use, young age at debut, treatment noncompliance), as well as positive prognostic factors (good premorbid functionality, present social support network, absence of genetic load in first-degree relatives, administration of injectable long-lasting antipsychotic Xeplion® which may reduce the frequency of relapses and the need of hospital admissions).
The case particularity consisted especially in the existence of prolonged use of psychoactive substances, and in terms of symptoms, we retain the apparition of kinesthetic hallucinations and visual illusions with a mystical theme, as well as the cystic formation of the pineal gland.
Discussion
The unspecified vulnerability background, burdened by the hyperkinetic disorder with behavior disorder, may suggest a genetic vulnerability that materialized at the adult age in a psychotic disorder. On the other hand, a possible biological vulnerability materialized in the imaging alteration suggestive of the pineal gland cyst, as well as the existence of the untreated endocrine illness (thyrotoxicosis) at the recommendation of the endocrinologist thanks to normal levels of thyroid hormones.
The existence of a possible early prodrome even from the teenage years is supported in this case by the poor premorbid adaptation with a progressive decline of school performance, with the lack of job integration upon finishing school and the apparition of psychoactive substance use, the presence of negative symptoms of the disease, as well as low social relation levels.
We underline the negative evolution of the disease from the association of a considerable number of negative prognostic factors but, at the same time, it is worth mentioning the lack of family involvement in motivating the patient to adhere to the treatment.
Also, there is an elevated level of expressed emotions from the mother, with an intrusive and controlling behavior, with intimacy intrusion, paired with a faded father figure with a lack of interaction and implication with the patient. On the other hand, we mention the negative impact of the psychoactive substance use on the therapeutic responsiveness of the patient due to the accentuation of cerebral neurotransmission imbalance (especially in catecholaminergic transmission) at the receptor level by the amplification of displasticity of the involved receptors in triggering and maintaining psychotic symptoms and possibly going further at the level of secondary messengers and genetic expression caused by the use of psychoactive substances.
Moreover, it is worth mentioning the patoplastic character of the patient’s personality which negatively contributed to the later evolution of the disease and psychoactive substance use, the personality being an interface between the disease and the used psychoactive substances.
Conclusions
The presented case constitutes an additional argument to the fact that multiple psychoactive substance use is one of the frequent psychiatric comorbidities associated with schizophrenia; also, in this patient’s case, the use of speed, designer drugs and marijuana can be considered a precipitating factor in the apparition of schizophrenia. On the other hand, personality traits like dissocial or borderline can constitute an interface between the psychotic disorder and the excessive use of legal and illegal psychoactive substances and, lastly, the fact that the patient was first admitted in the outpatient department of pediatric neuropsychiatry at the age of 6, followed by poor adherence to the recommended treatment.
Early intervention programs and relapse prevention play an essential role in the evolution of these patients.
Bibliografie
- Khokhar JY, Dwiel LL, Henricks AM, Doucette WT, Green AI. The link between schizophrenia and substance use disorder: A unifying hypothesis. Schizophr Res. 2018;194:78-85.
- Green AI, Noordsy DL, Brunette MF, O’Keefe C. Substance abuse and schizophrenia: pharmacotherapeutic intervention. J Subst Abuse Treat. 2008;34(1):61-71.
- World Health Organization (WHO). The ICD-10 Classification of Mental and Behavioural Disorders. World Health Organization, 1993.
Articole din ediţiile anterioare
Iluziile perceptive – un posibil candidat în diagnosticul schizofreniei? (partea I)
Schizofrenia ca tulburare psihopatologică este marcată de manifestări disfuncţionale neurocognitive, mai ales la nivelul funcţiilor senzoriale şi c...
„Părinţii mei chiar sunt canibali.“ Schizofrenie paranoidă şi tulburare de personalitate narcisică
Prezentăm cazul unui pacient în vârstă de 35 de ani, diagnosticat cu schizofrenie la vârsta de 22 de ani, cu o personalitate premorbidă dizarmonică...
The concept of integrative psychiatry and the assessment of risk factors of antisocial potential in patients with schizophrenia
Psihiatria integrativă urmăreşte asocierea la perspectiva biologică a unor factori complementari cu rol în profilaxia şi tratamentul tulburărilor m...
Canabidiolul – zeci de ani de cercetare şi utilizările clinice actuale
Deşi majoritatea cercetărilor referitoare la canabis s-au concentrat asupra delta-9-trans-tetrahidrocanabinolului (THC), recent alte componente ale...