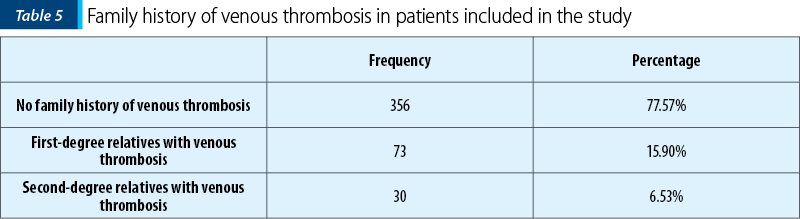
Thrombophilia refers to a predisposition to hypercoagulable state and can be identified in 30-50% of the cases of venous thromboembolism. The etiology of thrombophilia is multifactorial and related to both acquired and inherited factors. In our study, 22.45% of the patients had a positive family history of venous thrombosis. Most of the patients had two (64.7%) or three (24%) spontaneous abortions, but cases of five or six recurrent miscarriages at the same patient were recorded in our study. Thrombophilia is diagnosed only by blood tests, and the current guidelines recommend that thrombophilia testing should be considered in case of recurrent miscarriages or fetal death.
Trombofilia ereditară şi complicaţiile obstetricale mediate de placentă
Inherited thrombophilia and placenta-mediated pregnancy complications
First published: 13 martie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.27.1.2020.2871
Abstract
Rezumat
Trombofilia se referă la o predispoziţie către o stare de hipercoagulabilitate şi poate fi identificată în 30-50% din cazurile de tromboembolism venos. Etiologia trombofiliei este multifactorială şi legată atât de factori dobândiţi, cât şi ereditari. În studiul nostru, 22,45% dintre paciente au avut antecedente familiale de tromboză venoasă. Majoritatea pacientelor au avut câte două (64,7%) sau trei (24%) avorturi spontane, dar au fost înregistrate şi cazuri de cinci sau şase avorturi recurente la aceeaşi pacientă. Trombofilia este diagnosticată prin analize de sânge, iar ghidurile actuale recomandă ca testarea trombofiliei să fie luată în considerare în caz de avorturi recurente sau de moarte fetală intrauterină.
Introduction
Thrombophilias have been linked in many studies to adverse pregnancy outcomes, such as preeclampsia, placental abruption, fetal growth restriction, stillbirth, thrombosis and recurrent pregnancy loss(1).
The hypercoagulable state in pregnancy is normal, but it increases the risk of thrombotic complications in patients with inherited thrombophilias. The condition creates a pathological hypercoaguable state which leads to arterial and venous thrombosis at the site of implantation or in the placental blood vessels(2). The latest studies suggest that hypercoagulation is the main pathophysiological mechanism which leads to uteroplacental insufficiency(3,4). The placenta’s infarcts have been defined as localized area of coagulative necrosis in the placenta’s parenchyma. Increased syncytial knots, most commonly seen with maternal vascular underperfusion, were also assessed not only in maternal, but also in fetus thrombophilia(5).
Thrombophilia has no symptoms when it is not complicated. Many patients with thrombophilia do not develop a blood clot and never have symptoms.
Thrombophilia is diagnosed by laboratory testing. The current guidelines suggest that thrombophilia testing should be recommended in case of recurrent miscarriage or fetal death.
A blood clot in an artery is called arterial thrombosis. Depending on which artery is affected, a blood clot in an artery can cause placenta-mediated pregnancy complications(6). Thus, the possible symptoms of arterial thrombosis due to thrombophilia are repeated miscarriages, preeclampsia, intrauterine fetal growth or fetal death(7).
Materials and method
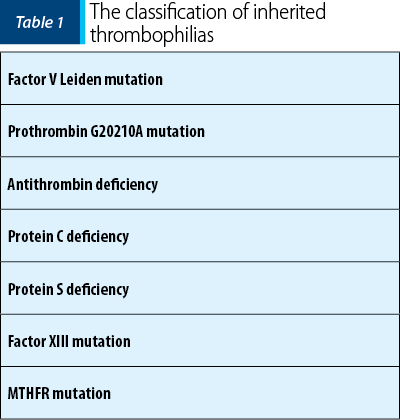
We included in our study 459 pregnant women with gestational ages ranging from 14 weeks to 28 weeks. All patients included in the study were tested for hereditary thrombophilia, and the laboratory samples included: factor V Leiden, homocysteine, prothrombin G20210A mutations and antithrombin, protein S and protein C deficiencies, gene MTHFR mutation, and mutation of factor XIII.
This study was approved by the Ethical Committee of the Bucharest Emergency University Hospital, and the informed consent was obtained from each woman.
All data are presented as mean ± standard error of the mean. All statistical analyses were performed using SPSS version 21. Also, Cramér’s V (Cramér’s phi) test and cluster analysis were performed. P<0.05 was considered to indicate a statistically significant difference.
Results
The average age of patients included in the study was 33 years old (±5.20), the average weight was 68 kg (±12.42), the average height was 165 cm (±10.20), and the average Body Mass Index was 25.20 (±4.62).
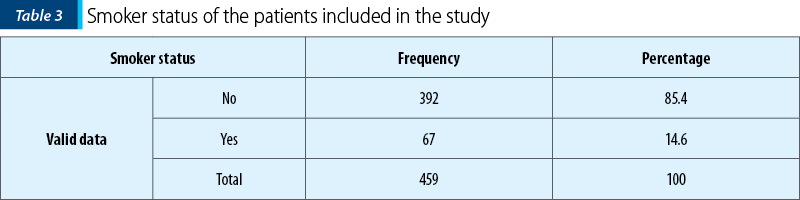
The patients included in the study were living mostly in urban areas (384 patients; 83.7%) and were nonsmokers (392 patients; 85.4%). A small proportion of patients were smokers (14.6%).

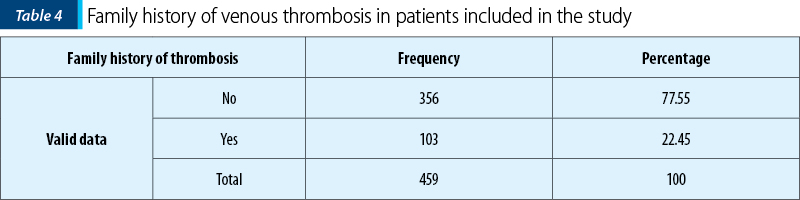
A total of 22.45% of patients had positive family history of venous thrombosis. Furthermore, 15.90% of them had family history of first-degree relatives who have been diagnosed with venous thrombosis.
The women with inherited thrombophilia, especially those with combined defects, have an increased risk of fetal loss, particularly stillbirth.
In our study group, the most common type of thrombophilic mutation was MTHFR mutation (25.7%), followed by the prothrombin gene mutation (20.9%) and the Leiden factor V mutation (15.7%).
Miscarriage is the most common complication of early pregnancy. The average number of spontaneous abortions in the patients included in our study was three, the average number of pregnancies lost in the first trimester was two, and the average number of pregnancies lost in both the second and third trimesters was one, respectively zero.
The majority of patients lost two (64.7%) or three (24%) pregnancies, but cases of five missed pregnancies (2%) or six missed pregnancies (0.2%) were recorded in our study.
Discussion
In our study group, the most common type of thrombophilic mutation was MTHFR mutation (25.7%), followed by the prothrombin gene mutation (20.9%). Also, a huge number of patients (64.7%) with thrombophilic pattern had two spontaneous abortions. The risk of fetal loss was increased in women with thrombophilia.
Recurrent miscarriage is defined as the loss of three or more consecutive pregnancies before 20 weeks of gestation(8). Thrombophilia is a common cause of pregnancy loss and is reported in 40-50% of cases. Combined thrombophilia has been identified by several researchers as a cause of recurrent miscarriage, but the frequency of combined thrombophilia is not known exactly(9).
One of the most proeminent investigations regarding the impact of maternal thrombophilia on placental changes during pregnancy was performed by Rogers et al. They found a statistical association of increased syncytial knotting and hypervascular villi with maternal FVL mutation, suggesting that hypoxia of the placental vascular bed occurs more frequently in mothers with FVL mutation than in those without this mutation(10).
Conclusions
Family history is a risk indicator for the first venous thrombosis. In clinical practice, family history may be more useful for risk assessment than thrombophilia testing.
Inherited thrombophilia should be considered if the patient has recurrent thrombosis at a young age and positive family history.
Thrombophilia remains a major problem due to the medical, psychological and social implications on the women diagnosed with this disease.
Conflicts of interests: The authors declare no conflict of interests.
Bibliografie
- Abu-Heija A. Thrombophilia and recurrent pregnancy loss: Is heparin still the drug of choice? Sultan Qaboos Univ Med J. 2014; 14(1):e26–e36.
- Redline RW. Thrombophilia and placental pathology. Clin Obstet Gynecol. 2006; 49(4):885-94.
- Ramírez YL, Vivenes M, Miller A, Pulido A, Mora JL, Arocha-Piñango CL, Marchi R. Prevalence of the coagulation factor XIII polymorphism Val34Leu in women with recurrent miscarriage. Clin Chim Acta. 2006; 374(1-2):69-74.
- Bick RL. Recurrent miscarriage syndrome and infertility caused by blood coagulation protein or platelet defects. Hematol Oncol Clin North Am. 2000; 14(5):1117-31.
- Van den Boogaard E, Cohn DM, Korevaar JC, Dawood F, Vissenberg R, Middeldorp S, et al. Number and sequence of preceding miscarriages and maternal age for the prediction of antiphospholipid syndrome in women with recurrent miscarriage. Fertil Steril. 2013; 99(1):188-92.
- Mitriuc D. Trombofilia şi complicaţiile sarcinii – aspecte de etiopatogenie şi fiziopatologie. Bul Perinatol. 2017; 74(2):84-8.
- Ivanov P, Tsvyatkovska T. Pregnancy thrombophilia: the unsuspected risk. BoD – Books on Demand. 2013.
- Saravelos SH, Li TC. Unexplained recurrent miscarriage: how can we explain it? Hum Reprod. 2012; 27(7):1882-6.
- Visser J, Ulander VM, Helmerhorst FM, Lampinen K, Morin-Papunen L, Bloemenkamp KW, Kaaja RJ. Thromboprophylaxis for recurrent miscarriage in women with or without thrombophilia. Thromb Haemost. 2011; 105(02):295-301.
- Brenner B. Inherited thrombophilia and pregnancy loss. Thromb Haemost. 1999; 82(08):634-40.
Articole din ediţiile anterioare
Managementul displaziilor cervicale în contextul sarcinii
Neoplazia cervicală intraepitelială şi cancerul cervical sunt cele mai frecvente diagnostice citologice întâlnite în populaţia pacientelor gravide ...
Efectele vitaminei D în sarcină
Naşterea, creşterea, dezvoltarea, reproducerea şi îmbătrânirea în condiţii fiziologice pot fi realizate fără a diminua rolul celorlalte aspecte ...
Coagularea intravasculară diseminată produsă la domiciliu în al treilea trimestru al sarcinii - două cazuri clinice
Coagularea intravasculară diseminată (CID), asociată sarcinii şi naşterii, este un eveniment rar, cu evoluţie potenţial fatală; studiile indică o i...
Sarcina depăşită cronologic – riscuri şi management
În România, sarcina depăşită cronologic este definită ca o sarcină cu durată mai mare de 41 de săptămâni şi 0 zile. Determinarea unei sarcini...