Introduction. The pharyngeal extension of the parotid gland is an extension of the gland from the deep face of the parotid gland to the pharyngeal wall. This extension explains the spread of parotid pathology to the parapharyngeal space and the infratemporal fossa. Materials and method. We present the clinical case of a 54-year-old female patient with a left parotid gland tumor with three previous surgeries, with recurrence at less than one year after surgery. The cervical MRI examination revealed a multiloculated tumor with extension at the left infratemporal fossa. We complemented the classical surgical approach with a transmandibular approach for the radical ablation of the tumor. The histopathology result was capillary hemangioma. Discussion. We update some notions of surgical anatomy about the infratemporal fossa and discuss the particular aspects of the tumor extension in the presented case. We also discuss the histological particularities of the operated tumor. Conclusions. Large tumors of the parotid gland may also involve pharyngeal extension of the gland. High-performance imaging is required for the correct assessment of tumor extension. A planning of the surgical approach is necessary, and the transmandibular approach can widen the access for a radical ablation of such a tumor.
Tumorile prelungirii faringiene a glandei parotide. Comentarii pe marginea unui caz clinic de hemangiom recidivant
Tumors of pharyngeal extension of the parotid gland. Comments on a clinical case of recurrent hemangioma
First published: 13 decembrie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Orl.45.4.2019.2726
Abstract
Rezumat
Introducere. Prelungirea faringiană a glandei parotide este o extensie a glandei dinspre faţa profundă a lojei parotidiene către peretele faringian. Această prelungire explică extensia patologiei parotidiene către spaţiul parafaringian şi fosa infratemporală. Materiale şi metodă. Prezentăm cazul clinic al unei paciente de 54 de ani, cu o tumoră parotidiană stângă operată iterativ de trei ori, cu recidivă la mai puţin de un an după chirurgie. Examenul IRM cervical a evidenţiat o tumoră multiloculată cu extensie la nivelul fosei infratemporale stângi. Am completat abordul chirurgical clasic cu un abord transmandibular pentru ablaţia radicală a tumorii. Histopatologia a fost de hemangiom capilar. Discuţie. Vom reactualiza câteva noţiuni de anatomie chirurgicală despre fosa infratemporală şi vom discuta aspectele particulare ale extensiei tumorale în cazul prezentat. Vom aborda şi particularităţile histologice ale tumorii operate. Concluzii. Tumorile voluminoase ale glandei parotide pot implica şi prelungirea faringiană a glandei. Imagistica de înaltă performanţă este obligatorie pentru aprecierea corectă a extensiei tumorale. Este necesară o planificare a abordului chirurgical, iar abordul transmandibular poate lărgi accesul în vederea unei ablaţii radicale a unei astfel de tumori.
Introduction
The parotid lodge is open to its deep face through a slot facing the lateral wall of the pharynx. Through this slot, an extension of the deep lobe of the parotid gland enters through the lateral wall of the pharynx, also representing a path of extension of the pathology as tumors and suppurations from the parotid lodge to the maxillo-pharyngeal space(1). Thus, a tumor involving the deep lobe of the parotid gland can extend to the parapharyngeal space and the infratemporal fossa. There are described three levels of parapharyngeal extension of the deep lobe. At level 1, the tumor extension follows the line of minimum resistance between the ascending branch of the mandible and the mastoid, below the angle of the mandible, being in relation to the pterygoid muscles. At level 2, the extension is made posteriorly of the pterygoid muscles, being in relation to the pterygoid plexus and the internal maxillary artery. At level 3, the tumor extension pushes the superior constrictor muscle and the medial buccinator muscle and enters the parapharyngeal space(2), the clinical expression being the swelling in the pharyngeal lateral wall that can be seen at bucopharyngoscopy.
The parapharyngeal space has one prestyloid compartment and one retrostyloid compartment, separated by the styloid diaphragm, a complex muscular fibrous ligamental structure consisting of the posterior belly of the digastric muscle, the stylohyoid, styloglossus and stylopharyngeus muscles and the stylohyoid and stylomandibular ligaments(3). The tumors of the deep lobe of the parotid gland extend anteriorly from this diaphragm into the prestyloid compartment(4).
The infratemporal fossa represents an irregular retromaxillary space that has as an upper limit – the large medial sphenoid wing and the temporal bone until the infratemporal ridge; medial – the lateral surface of the lateral blade of the pterygoid process; anterior – posterior wall of the maxilla; inferior – communicates with the neck(5). This inferior communication is partially closed by the medial pterygoid muscle. Subsequent to this muscle, the parapharyngeal space communicates with the infratemporal fossa(6). Conley classifies infratemporal fossa tumors into primary tumors, originating in fossa structures (25-30%)(5,6), and tumors by contiguity, which extend into the infratemporal fossa from neighboring structures, most commonly from the parotid gland, but also from the paranasal sinuses, nasopharynx, middle cerebral fossa and external auditory canal(5-7). The extension of a parotid tumor at the level of the infratemporal fossa requires a transmandibular surgical approach for correct exposure and safe ablation(5,8).
Case report
We present the case of a 54-year-old female patient with a left parotid gland tumor operated iteratively three times, the last time 25 years ago from the time of admission, with a local recurrence less than one year after every surgery. She presented left peripheral facial nerve palsy in the inferior territory after the second operation. The tumor has shown accelerated growth over the last 6 months. At the moment of admission in our clinic, the patient had a large tumor in the left parotid region, with a firm but not hard consistency that suggested non-malignancy, without invasion of the skin, without palpable adenopathy. The tumor had spread in the masseter region, with discrete trismus. Also, left peripheral facial paralysis was found, especially in the lower territory (Figure 1).

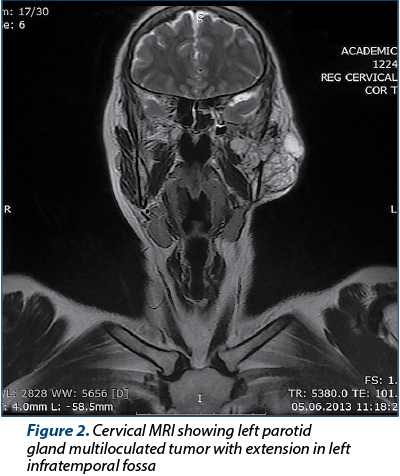
The cervical MRI examination revealed a multiloculated left parotid gland tumor, in hypersignal on T2-weighted MRI, with important enhancement after contrast administration, and showed an extension in the left infratemporal fossa (Figure 2).
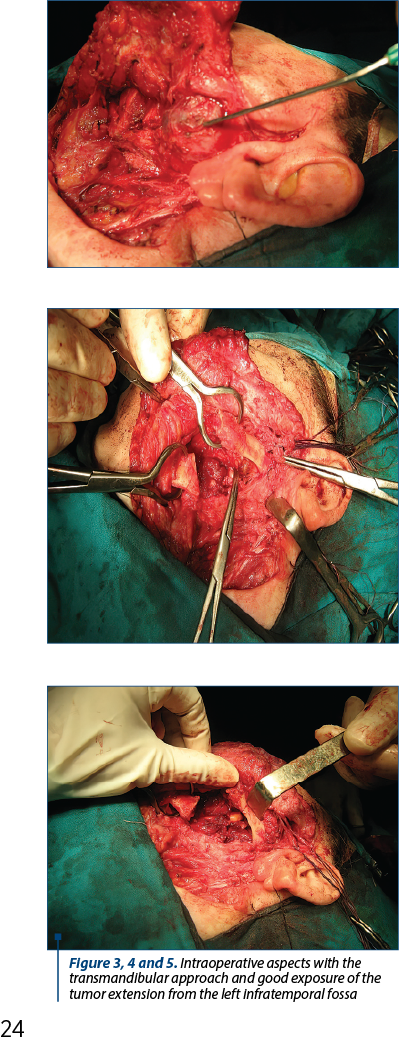
The surgery was performed in a mixed team with the maxillo-facial surgeon. We used a modified Redon-type approach combined with a left transmandibular approach to allow a good exposure of the tumor. The mandibulotomy was made at the angle of mandible and allowed a good view of the tumor extension which was in contact with left internal maxillary artery, venous pterygoid plexus, left lingual nerve and with the posterior wall of maxillary sinus. The hemostasis was difficult, but we succeeded due to the right exposure. We performed an extended revision left parotidectomy with partial preservation of the left facial nerve, achieving radical ablation of the parotid tumor with left infratemporal extension (Figures 3, 4 and 5). The histopathological and immunohistochemical result was capillary hemangioma.

The evolution of the case was favorable. The left peripheral facial palsy and trismus were slightly accentuated. The patient was monitored by clinical examination and by cervical MRI for 5 years and had no local recurrence (Figure 6).
Discussion
Hemangiomas are vascular tumors that can be cavernous or capillary, depending on the size of the blood vessels(9). Parotid gland localization is more unusual and is suitable for differential diagnosis with lymphangioma, a proliferation of lymphatic vessels considered to be congenital and found in childhood(9-11). Almost 75% of cases involve the head and neck region, the submandibular and parotid regions being the most common locations(10,11). Hemangio-lymphangiomas are also described in literature, which are lymphangiomas with a vascular component(10). We consider this case to be rather in this category, although immunohistochemistry confirmed the form of capillary hemangioma. The multiloculated character of the lesion and the recurrence after previous surgical interventions also advocate for an aspect of hemangio-lymphangioma. Tumor extension from the deep lobe to the infratemporal fossa explains the recurrence after the three previous surgeries, probably representing a tumor residue.
We consider that high-performance imaging such as cervical MRI is mandatory and can properly highlight the tumor extension.
The transmandibular surgical approach, with osteotomy at the angle of the mandible, allowed the direct visualization of the tumor(3,4), which was in contact with the lingual nerve and the internal maxillary artery, and its ablation with the correct control of hemostasis.
Regarding the facial nerve, it is certain that the surgical reintervention was a new trauma, with postoperative fibrosis, explaining the left facial palsy progression despite the preservation of the middle and upper fascicles of the facial nerve. Radical ablation of the tumor, en-bloc, with the invaded left masseter muscle, as well as with the extension of the left infratemporal fossa, provided surgical healing.
Conclusions
Tumors that exclusively involve the pharyngeal extension of the parotid gland are rare. Most commonly, these are large tumors of the parotid gland, which also involve pharyngeal extension. High-performance imaging MRI type with reconstruction is required for the correct assessment of tumor extension. A planning of the surgical approach is necessary, and the transmandibular approach can widen the access for a radical ablation of such tumors.
Conflict of interests: The authors declare no conflict of intersts.
Bibliografie
- Dass A, Gupta N, Singhal SK, Verma H. Tumours of Deep Lobe of Parotid Gland: Our Experience. Indian J Surg. 2015 Dec; 77(Suppl3):945-8.
- Lore JM, Medina J. Deep lobectomy of Parotid Salivary gland. An Atlas of Head & Neck Surgery. 2005; Elsevier Inc., 868-72.
- Bozza F, Vigili MG, Ruscito P, Marzetti A, Marzetti F. Surgical management of parapharyngeal space tumours: result of 10-year follow-up. Acta Otorhinolaryngol Ital. 2009 Feb; 29(1):10-15.
- Cassoni A, Terenzi V, Della Monaco M, Bartoli D, Battisti A, Rajabtork ZO, Valentini V. Parapharyngeal space benign tumours: our experience. J Craniomaxillofac Surg. 2014 Mar; 42(2):101-5.
- Tiwari R, Jasper JQ, Egeler S, Ludi S. Tumors of the Infratemporal Fossa. Skull Base Surgery. 2000 Febr; 10(1):1-9.
- Kalish LH, Ng T, Da Cruz MJ. Pseudogout mimicking an infratemporal fossa tumor. Head Neck. 2010 Jan; 32(1):127-32.
- Basaran B, Polat B, Unsaler S, Ulusan M, Aslan I, Hafiz G. Parapharyngeal space tumours: the efficiency of a transcervical approach without mandibulotomy. Acta Otrhinolaryngol Ital. 2014 Oct; 34(5):310-6.
- Mansour OI, Carrau RL, Snyderman CH, Kassam AB. Preauricular Infratemporal Fossa Surgical Approach: Modifications of the Technique and Surgical Indications. Skull Base. 2004 Aug; 14(3):143-151.
- Thakral A, Sharma SM. Cervicofacial hemangiomas: pattern, clinical management and treatment outcomes. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013 Dec; 116(6): e457-64.
- Vrînceanu D, Dorobăţ BC, Sajin M, Mogoanţă CA, Oprişcan IC, Hîncu MC, Georgescu MG. Cystic lymphangioma of nasopharynx in a 54-year-old man – case report. A new histogenetic hypothesis. Rom J Morphol Embryol. 2018 Aug; 59(2):577-584.
- Adams DM, Lucky AW. Cervicofacial vascular anomalies. I. Hemangiomas and other benign vascular tumors. Semin Pediatr Surg. 2006 May; 15(2):124-32.
Articole din ediţiile anterioare
Etiopatogenia cancerului de hipofaringe
Lucrarea reprezintă o trecere în revistă a factorilor de risc și a modalităților prin care aceștia intervin în etiopatogenia cancerului de hipofari...
Tulburările de deglutiţie în patologia tumorală cervico-facială – strategie diagnostică şi terapeutică
Disfagia orofaringiană se defineşte prin perturbarea pasajului bolului alimentar de la gură până la esofag, respectiv printr-o tulburare a deglutiţ...
Tumora de glomus carotidian. Prezentare de caz clinic
Tumorile glomice sau paraganglioamele sunt tumori rar întâlnite, cu creştere lentă şi de obicei benigne. Acestea se pot întâlni la nivelul arte...
Reabilitarea deglutiţiei într-un caz de tumoră parafaringiană gigantă. Prezentare de caz
Autorii prezintă un caz de tumoră parafaringiană prestiliană voluminoasă (diametrul peste 10 cm), cu aspect histopatologic de adenom pleomorf de gl...