The optimal management of leiomyomas during caesarean delivery remains unclear, as it may be considered feasible and a safe procedure, or an absolute contraindication. Recent meta-analyses suggest that caesarean myomectomy is associated with clinical insignificant increase in operative time, blood loss and hospital stay, especially with multiple and large-size myomas, and should be taken into consideration by experienced surgeons with appropriate hemostatic techniques and tertiary-care centers. We present the case of a patient diagnosed with a large submucous leiomyoma who underwent caesarean myomectomy, with an excellent postoperative outcome. We also review the most recent data published in literature regarding the advantages and downsides of performing this surgical intervention.
Large submucous myoma in pregnancy: is caesarean myomectomy an option?
Fibrom uterin submucos voluminos în sarcină: este miomectomia intrapartum o opţiune?
First published: 27 noiembrie 2023
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.42.4.2023.8985
Abstract
Rezumat
Managementul optim al leiomioamelor uterine în cazul pacientelor care nasc prin operaţie cezariană rămâne un subiect de dezbatere, întrucât extirparea lor poate fi considerată oportună şi sigură sau, din contră, total contraindicată. Studii recente sugerează că miomectomia intrapartum se asociază cu o creştere nesemnificativă a timpului operator, a sângerării şi a duratei de spitalizare, în special în cazul fibroamelor mari sau multiple, şi ar trebui luată în considerare de către chirurgii experimentaţi din centrele terţiare care au acces la tehnici moderne de hemostază. În această lucrare, prezentăm cazul unei paciente diagnosticate cu un fibrom submucos voluminos, care a beneficiat de miomectomie intrapartum, cu prognostic postoperatoriu excelent. De asemenea, raportăm şi rezultatele celor mai recente studii publicate în literatură asupra avantajelor şi dezavantajelor acestui tip de intervenţie chirurgicală.
Introduction
Leiomyomas are the most common benign tumors of the reproductive tract in women of childbearing age(1). The prevalence of uterine leiomyomas during pregnancy has been increasing along with the advancing age of women, so they place an additional burden on obstetricians during the course of antenatal care(2).
Routine myomectomy at the time of caesarean section has been condemned in the past due to the fear of uncontrolled hemorrhage and peripartum hysterectomy. However, in modern obstetrics, studies have shown that it does not increase complications or transfusion rates, and it appears to be a safe procedure in selected patients(3-7).
In the present paper, we report the case of a successful myomectomy performed during the caesarean section, and also we assess the available data published in literature regarding this intervention.
Case report
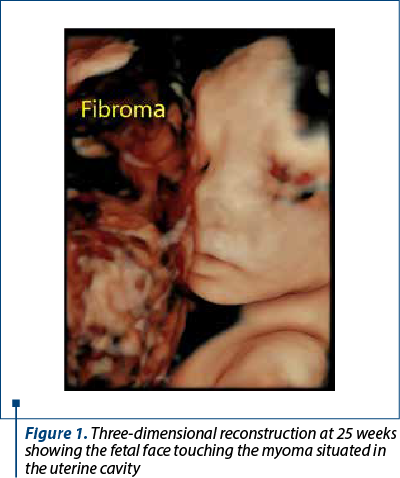
A 36-year-old gravida 1 (births 0, abortus 0) Caucasian woman diagnosed with a large submucous uterine leiomyoma received prenatal care in our department of fetal medicine. The patient had been diagnosed before pregnancy with uterine leiomyoma, but her physician did not offer myomectomy at that time. The pregnancy was spontaneous and planned. She had a normal NIPT (non-invasive prenatal testing) result, and all three ultrasonographic examinations for screening for fetal anomalies were normal. What is to be mentioned is that all throughout the pregnancy, the fetal movements were reduced during ultrasound examinations because of the submucosal development and the size of the fibroid (Figure 1). Still, the patient had no symptoms during pregnancy (such as pain or vaginal bleeding), and all the antenatal tests were normal, so her antenatal period was completely uneventful.
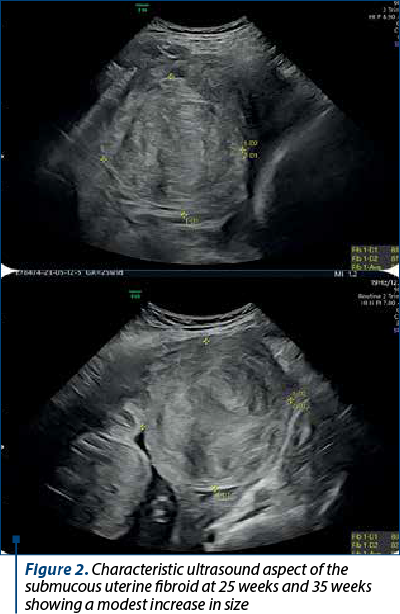
The uterine leiomyoma had a modest increase in size throughout the pregnancy, from 81.4 mm diameter at 25 weeks to 88 mm at 35 weeks of gestation (Figure 2).
At 38 weeks, the patient delivered by caesarean section; an informed written consent was obtained from her after adequate counseling was offered regarding the risk of excessive bleeding, need for blood transfusion, and peripartum hysterectomy. Her preoperative hemoglobin was 11.6 g/dL, hematocrit was 35.3%, and her blood group was A positive. Adequate blood products were arranged, and a multidisciplinary team was involved (obstetrician-gynecologists, anesthesiologists and neonatologists).
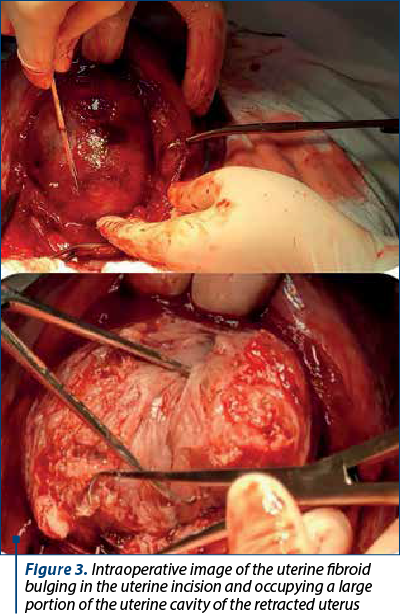
After the extraction of the fetus and the placenta, a large submucous isthmic uterine mass was observed. We decided to perform myomectomy as the fibroid was bulging into the incision line, occupying a large portion of the uterine cavity and causing difficulty in performing the uterine suture (Figure 3). Prophylactically, carbetocin infusion was administered. The fibroid was easily enucleated and the myoma bed was closed with delayed absorbable sutures followed by normal closure of the uterine incision with a single-layer suture. A complete hemostasis was achieved. The total duration of the intervention was 50 minutes. Broad-spectrum antibiotics and analgesics were administered in the postoperative period. Her post-surgery hemoglobin was 9.7 g/dL, and hematocrit was 29.2%, thus not requiring any blood transfusion. We only recommended iron supplements for three months.
The patient had an uneventful recovery, being discharged on the fourth day after surgery. At the follow-up examination at six weeks postpartum, the uterus was completely involuted and the repeated ultrasound examination showed no uterine fibroid. The pathological report of the specimen confirmed the uterine leiomyoma.
Discussion
The surgical removal of leiomyomas at the time of caesarean section is still considered a controversial issue, as many obstetricians do not advocate myomectomy in order to avoid severe hemorrhage. However, many recent studies have concluded that the procedure is not dangerous and does not lead to complications in the hands of an experienced obstetrician.
Careful selection of cases should be done in order to minimize complications.
Intramural myomas, myomas over 7 cm in size and multiple myomas are associated with more intraoperative hemorrhage and prolonged operation duration(6). Moreover, bleeding can be prevented by uterotonic infusion (oxytocin or carbetocin) or by ligating the uterine arteries using a tourniquet(8,9). In our case, although the size of the fibroid was increased, its position in the uterine cavity made enucleation easy, and we did not need to perform uterine artery ligation, as bleeding was not threatening. Actually, the myometrium is more elastic and less fragile during pregnancy compared to non-pregnancy, so it is easier to suture during caesarean myomectomy(10).
A recent retrospective cohort study identified the risk factors of intraoperative hemorrhage during caesarean myomectomy; the results showed that lower segmental location and the diameter (over 8 cm) were significant independent risk factors, this data highlighting that our case was a high-risk one(11). On the other hand, leaving a large myoma in place may increase the risk of postpartum bleeding, degeneration, spontaneous abortion and preterm labor in a future pregnancy(12).
It is not less true that nearly all studies supporting caesarean myomectomy are retrospective, this suggesting that evidence may still be weak. With increasing reports in favor of this intervention, the risk-benefit ratio should be still evaluated with randomized controlled trials in order to achieve more clear data.
Conclusions
The idea of performing caesarean myomectomy appears to be winsome in selected cases. Although it may prolong the operative time, it may have benefits, including avoiding another operation to remove the uterine fibroids. If it is performed by experienced surgical teams in a properly equipped center, it can be a safe procedure to be implemented in routine practice.
Conflict of interest: none declared.
financial support: none declared.
This work is permanently accessible online free of charge and published under the CC-BY licence.

Bibliografie
-
Garg P, Bansal R. Cesarean myomectomy: a case report and review of the literature. J Med Case Rep. 2021;15(1):193.
-
Kellal I, El Haddouchi N, Lecuyer AI, Body G, Perrotin F, Marret H. Leiomyoma during pregnancy: which complications?. Gynecol Obstet Fertil. 2010;38(10):569-75.
-
El-Refaie W, Hassan M, Abdelhafez MS. Myomectomy during cesarean section: a retrospective cohort study. J Gynecol Obstet Human Reprod. 2020:49(10):101900.
-
Sparic R, Kadija S, Stefanovic A, et al. Cesarean myomectomy in modern obstetrics: more light and fewer shadows. J Obstet Gynaecol Res. 2017;43(5):798-804.
-
Goyal M, Dawood AS, Elbohoty SB, et al. Cesarean myomectomy in the last ten years; a true shift from contraindication to indication: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2021;256:145-57.
-
Huang Y, Ming X, Li Z. Feasibility and safety of performing cesarean myomectomy: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2022;35(13):2619-27.
-
Pergiatolis V, Sinanidis I, Louloudis IE, et al. Perioperative complications of cesarean delivery myomectomy: a meta-analysis. Obstet Gynecol. 2017;130(6):1295-303.
-
Kwaeukume EY. Caesarean myomectomy. Afr J Reprod Health. 2002;6(3):38-43.
-
Sapmaz E, Celik H, Altungul A. Bilateral ascending uterine artery ligation vs. tourniquet use for hemostasis in cesarean myomectomy. A comparison. J Reprod Med. 2003;48(12):950-4.
-
Li H, Du J, Jin L, Shi Z, Liu M. Myomectomy during cesarean section. Acta Obstet Gynecol Scand. 2009;88(2):183-6.
-
Kwon JY, Byun JH, Shin I, et al. Risk factors for intraoperative hemorrhage during cesarean myomectomy. Taiwan J Obstet Gynecol. 2021;60(1):41-4.
-
Febo G, Tessarolo M, Leo L, Arduino S, Wierdis T, Lanza L. Surgical management of leiomyomata in pregnancy. Clin Exp Obstet Gynecol. 1997;24(2):76-8.
Articole din ediţiile anterioare
Interdisciplinary dental approach to a pregnant patient undergoing orthodontic treatment – case report
Dental treatment in pregnant women requires some particularities that limit and condition the therapeutic maneuvers(1). Endodontic pathologies in t...
Pregnancy-related low back pain – the benefits and results of rehabilitation medicine techniques
Pregnancy-related low back pain is one of the most common musculoskeletal complaints by pregnant women, resulting in an increased inability to per...
Giant isthmic fibromatous nodule developing within the cervix – clinical case
The fibromatous nodule (uterine fibroid) is a benign tumor that develops from tissue similar to the uterine muscle, being aided by an increased lev...
The metabolic pattern for monitoring and management of gestational diabetes
Globally, the prevalence rate of overweight or obesity between 1980 and 2013 increased by 27.5% for adults and by 47.1% for children, to a total of...