Modificări în incidenţa hipertensiunii induse de sarcină în 2007 versus 2017 în Spitalul Clinic de Obstetrică şi Ginecologie „Prof. Dr. Panait Sîrbu” Bucureşti
Changes in the incidence of pregnancy-induced hypertension in 2007 versus 2017 in the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology, Bucharest
Abstract
Pregnancy-induced hypertension is a common disease with important effects in maternal and fetal morbidity and mortality. The continuous study of its evolution in the population can help us to highlight new risk factors, the possible natural growth trend of the disease in pregnant women and the curative measures that can be taken. The purpose of this study is to observe the changes in the incidence of pregnancy-induced hypertension and its complications at a distance of 10 years. In order to achieve this goal, two study groups were compiled, including the births from 2007 and those from 2017 at the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology. The main findings of the study revealed an increasing trend of the incidence of pregnancy-induced hypertension, an apparent stagnation of the HELLP incidence, and a decrease in eclampsia.Keywords
hypertension in pregnancypreeclampsiaeclampsiaHELLP syndromeRezumat
Hipertensiunea indusă de sarcină este o patologie frecvent întâlnită, cu efecte importante în morbiditatea şi mortalitatea materno-fetală. Studiul continuu asupra evoluţiei acesteia în populaţie ne poate ajuta să evidenţiem noi factori de risc, eventuala tendinţă naturală de creştere a bolii la gravide şi măsurile curative care se pot lua. Scopul studiului de faţă rezidă în observarea modificării incidenţei hipertensiunii induse de sarcină şi a complicaţiilor acesteia la o distanţă de 10 ani. Pentru atingerea scopului s-au folosit două loturi de studiu cuprinzând naşterile din cadrul Spitalului Clinic de Obstetrică-Ginecologie „Prof. Dr. Panait Sîrbu” în 2007 şi 2017. Principalele rezultate ale studiului relevă o tendinţă de creştere a incidenţei hipertensiunii induse de sarcină, o aparentă stagnare a incidenţei HELLP şi o scădere a cazurilor de eclampsie.Cuvinte Cheie
hipertensiune în sarcinăpreeclampsieeclampsiesindrom HELLPIntroduction
Pregnancy-induced hypertension is a common pathology complicating between 3% and 10% of all pregnancies, with important effects on maternal and fetal morbidity and mortality. The continuous study of its evolution in the population can help us highlight new risk factors, the possible natural growth trend of the disease in pregnant women and the curative measures that can be taken.
The blood pressure of a pregnant woman undergo changes during pregnancy. The first trimester of pregnancy is accompanied by a decrease in blood pressure caused by active vasodilation, obtained through the action of local mediators such as prostacyclin and nitric oxide. This reduction in blood pressure predominantly changes the diastolic pressure, with a decrease of 10 mmHg often seen between 13 and 20 weeks of gestation(1).
Blood pressure continues to decrease until 22-24 weeks, when a physiological threshold is reached. After this time, there is a slow, gradual increase in blood pressure up to the levels prior to the pregnancy, characteristic to each patient.
Another change is the lowering of blood pressure immediately after birth, increasing then in the first five days of postpartum. Even women whose blood pressure has shown normal values during pregnancy may experience transient hypertension in the first postpartum period, perhaps reflecting a degree of vasomotor instability.
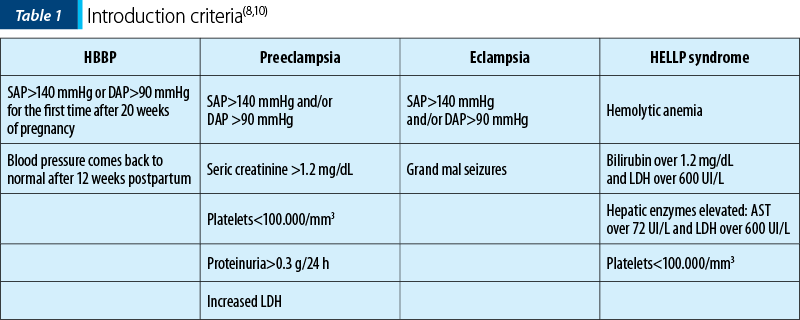
High blood pressure in pregnancy (HBBP) occurs when the “physiological threshold” of oscillations is exceeded and is manifested by systolic arterial pressure (SAP) >140 mmHg or diastolic arterial pressure (DAP) >90 mmHg for the first time in pregnancy after the 20th week, the blood pressure returning to normal after 12 weeks postpartum(2,3).
Preeclampsia is one of the most important complications of HBBP, the major cause of mortality and maternal-fetal morbidity. Specialty literature indicates a 5-7% incidence of preeclampsia in the general population of pregnant women. The mechanisms of preeclampsia are incompletely elucidated, the most accepted theory being that of the ineffective trophoblastic invasion of the spiral arteries of the uterus(4).
Eclampsia develops consecutively to preeclampsia, with specific symptoms, which anticipate seizures, such as confusion, photophobia, persistent migraines, epigastric pain or right hippocampus. It is a medical emergency, with serious complications, such as cerebral haemorrhage, acute renal failure, aspiration pneumonia, cardiac arrest. The only curative treatment of eclampsia is birth. According to the American College of Obstetricians and Gynecologists (ACOG), eclampsia is defined by the presence of grand mal seizures, newly developed in a pregnancy diagnosed with preeclampsia, which can manifest itself before, during or after the termination of labor. If the symptoms occur more than 48-72 hours postpartum or if seizures occur during antiepileptic treatment with magnesium sulphate, differential diagnosis should be done with arteriovenous malformation, an aneurysm rupture or idiopathic convulsion(4,5).
HELLP syndrome – whose name comes from the main associated changes: hemolysis, elevated liver enzymes and low platelets – may be associated with preeclampsia or may develop independently. The causes of the syndrome are incompletely elucidated. The pathological changes occur as a result of vasospasm, changes in vascular tone and coagulation defects, leading to endothelial lesions, platelet activation, and consequently the activation of the coagulation cascade(6,7).
This study aims to observe the changes in the incidence of pregnancy-induced hypertension and its main complications at a distance of 10 years in a third-degree maternity.
Materials and method
All the births of 2007 and 2017 at the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology were investigated, establishing the number of pregnant women with pregnancy-induced hypertension or complications.
HTAIS and complications cases (preeclampsia, eclampsia, HELLP syndrome) in 2007 vs. 2017
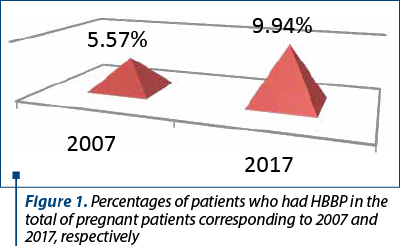
All pregnacies were studied, the first group was from 2007, with a total of 3412 pregnant women, of whom 198 (5.57%) were diagnosed with HBBP or complications, and the second group was from 2017, with a total of 3699 births, out of which 367 (9.94%) cases had HBBP or complications (preeclampsia, eclampsia, HELLP syndrome) – Figure 1.
The incidence of HTAIS (including preeclampsia, eclampsia, HELLP syndrome) by age group
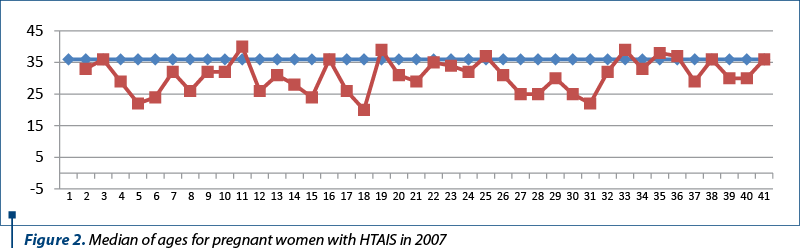
The group studied from the year 2007 showed ages between 19 and 42 years old. The mean age at which HBBP occurred (with or without complications) was 36 years old (Figure 2).
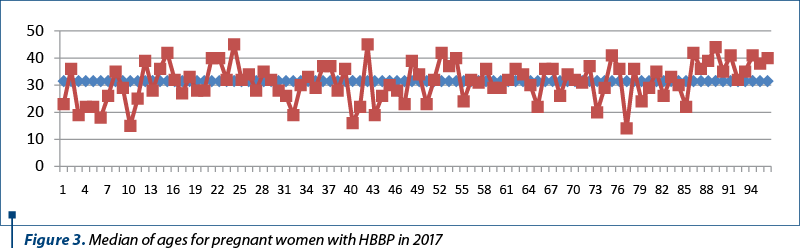
Of the total of 367 patients aged 14 to 45 years old, corresponding to 2017, an average of 32 years old for HBBP appearance (with or without complications) was calculated, 4 years lower than the average of 2007 (Figure 3).
The role of parity in the occurrence of HBBP (including cases of preeclampsia, eclampsia and HELLP syndrome)
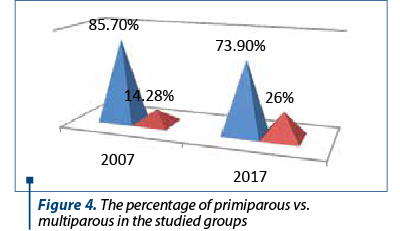
In both groups, HBBP prevalence (with or without complications) was higher in primiparous than in multiparous. For 2007, 85.7% of pregnancies developing HBBP (with or without complications) were primiparous, the percentage decreasing discretely to 73.9% in 2017 (Figure 4).
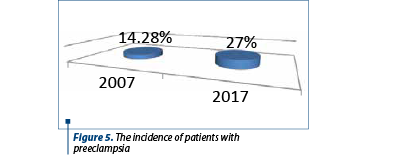
Incidence of preeclampsia in 2007 vs. 2017
The incidence of preeclampsia was registered in a higher percentage in 2017 (27%) compared to 2007 (14.28%), from the total percentage of patients with tensional pathology (Figure 5).
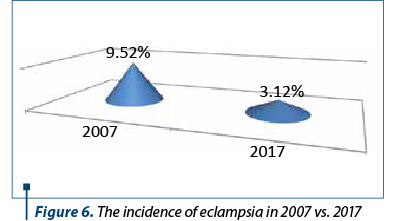
Incidence of patients with eclampsia in 2007 vs. 2017
In the case of eclampsia, there was a decrease of the percentage of pregnant women with this pathology, only 3.12% in 2017 compared to 9.53% in 2007 (Figure 6).
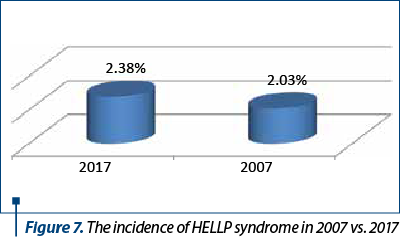
The incidence of HELLP syndrome in 2007 vs. 2017
After selecting and calculating the percentages of the groups, it became apparent that the proportion of pregnant women who had HELLP syndrome remained roughly unchanged at 10 years (Figure 7).
Discussion
The study reveals the importance of the early diagnosis and preventive medical conduct in HBBP cases. A proper management of pregnant women at risk reduced the percentage of HBBP consecutive complications(9).
The results are probably due to a correct tracking of pregnancies and the interdisciplinary collaboration (obstetrics-gynecology, cardiology, internal medicine, family medicine), and a decrease in the number of uninvestigated patients during pregnancy.
In 2018, the Mayo Clinic proposed preventive treatment with low-doses of acetylsalicylic acid for preeclampsia, starting at 12 weeks of gestation, especially in cases involving risk factors, or calcium supplementation in pre-pregnancy.
The European Society of Cardiology Guidelines for the Management of Cardiovascular Diseases During Pregnancy recommends the pharmacological treatment of hypertension during pregnancy only for women with severe hypertension.
In the other cases, a proper screening, changing lifestyle, eating habits and of other environmental factors that can be risk factors are sufficient in the HBBP management.
Conclusions
The study revealed an increasing tendency in HBBP (uncomplicated or associated with proteinuria) largely due to a better antenatal diagnosis and a decrease in the number of uninvestigated patients.
The mean age at which patients developed HBBP is lower in the 2017 age group (32 years old) compared to 2007 (36 years old).
There is a statistically significant increase in patients with hypertension in pregnancy, in those with prelampsia (14.2% in 2007 vs. 27% in 2017), a stagnation in HELLP syndrome (2.03% in 2007 vs. 2.38% in 2017), and a decrease in cases of eclampsia (9.5% in 2007 vs. 3.10% in 2017).
The patients’ compliance with treatment, and the easier access to information and prevention led to a decrease in the number of uninvestigated pregnant women and of complicated cases.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Kattah AG, Garovic VD. The management of hypertension in pregnancy. Adv Chronic Kidney Dis. 2013;20(3):229-39.
- Friel LA. Hypertension in pregnancy. https://www.msdmanuals.com/gynecology-and-obstetrics/pregnancy-complicated-by-disease (accessed 20.09.2018).
- Mustafa R, Ahmed S, Gupta A, Venuto RC. A comprehensive review of hypertension in pregnancy. J Pregnancy. 2012;105918:12.
- Williams Obstetrics, 24th ed, 2014, Hypertensive disorders; section 11:728-80.
- Bell MJ. A Historical Overview of Preeclampsia-Eclampsia. J Obstet Gynecol Neonatal Nurs. 2010;39(5):510-8.
- Lindheimer MD, Taler SJ, Cunningham FG. Hypertension in pregnancy. J Am Soc Hhypertens. 2008;2(6):484-94.
- Gillon TE, Pels A, von Dadelszen P, MacDonell K, Magee LA. Hypertensive disorders of pregnancy: a systematic review of international clinical practice guidelines. PLoS One. 2014;9(12):e113715.
- Tranquilli AL, Dekker G, Magee L, Roberts J, Sibai BM, Steyn W, Zeeman GG, Brown MA. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. 2014 Apr;4(2):97-104.
- Redman CWG, Jacobson SL, Russell R. Hypertension in pregnancy. Front Biosci. 2007: 2877-85.
- ACOG. Task force on hypertension in pregnancy. Practice Guideline. 2013:13-21; 31-47.
- https://www.acog.org/~/media/Task%20Force%20and%20Work%20Group%20Reports/public/HypertensioninPregnancy.pdf
