Riscurile pentru sănătatea mamei în cazul sarcinilor la vârste extreme
Mother’s health risks in extreme age pregnancies
Abstract
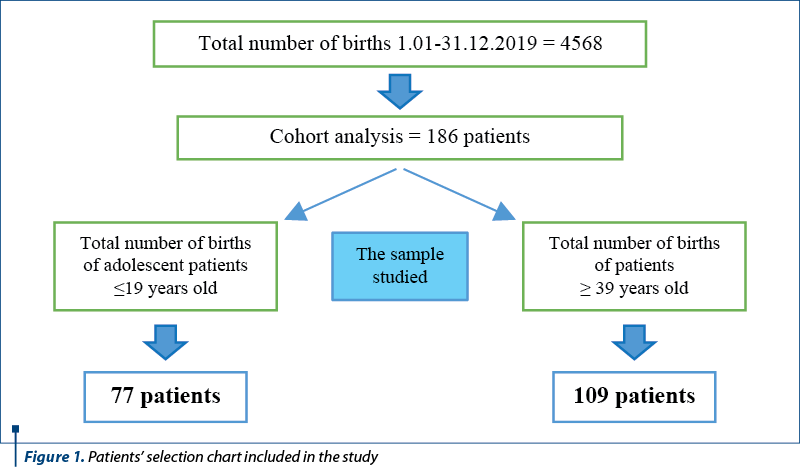
Introduction. Pathologies associated with pregnancy at extreme ages have potential significant clinical implications for both maternal and fetal health. Identifying the most common pathologies associated with pregnancy at extreme ages is a first step in the development and adaptation of protocols for health management given by midwives and nurses to patients in the prenatal, intrapartum and postpartum periods, according to the main risk factors related to age. Materials and method. The objective of the study was to evaluate a group of 186 pregnant patients who were hospitalized for childbirth in the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology, Bucharest, within 12 months. The main objective of the study was to identify the main pathologies associated with pregnancy at extreme ages. All pregnant patients of 19 years old or younger and of 39 years of age or older at the time of admission were included in the analysis. During the study, a quantitative research method was developed that evaluated several aspects, thus outlining the medical profile of patients. Results. Age comparative analysis of the data regarding the associated pathologies revealed that the prevalence of diabetes and hypertension was significantly higher among pregnant women in the second age group (39 years or older), while the scarred uterus had a higher frequency in pregnant women in the up to 19 years old group. The results of the study also indicate a higher frequency of missed pregnancies and intrauterine growth restrictions of fetuses in the patients group aged 39 years and older. Conclusions. The results of the study suggest the need for distinct approaches of healthcare for the two categories, taking into account the main issues identified. In the case of patients up to 19 years old, most of them at their first pregnancy but with fewer pathological implications, the healthcare management must include a stronger educational component (given the lack of experience in raising and caring for the newborn), while for the group of at least 39 years old, specific interventions are needed to focus on improving the knowledge, attitudes and practices of midwives and nurses regarding the prevention and provision of healthcare to patients at risk of developing pregnancy-related pathologies. Implementing healthcare education programs among adolescents can be helpful in ensuring a proper planning and in preventing unwanted pregnancies.Keywords
midwivesnurseshealth careelderly pregnancypregnant teenagersRezumat
Introducere. Patologiile asociate sarcinilor la vârste extreme au implicaţii clinice potenţiale semnificative atât asupra stării de sănătate a mamei, cât şi a fătului. Identificarea celor mai frecvente patologii asociate sarcinilor la vârste extreme reprezintă un prim pas în dezvoltarea şi adaptarea protocoalelor de acordare a îngrijirilor de sănătate acordate de moaşe şi asistenţi medicali pacientelor în perioada prenatală, intrapartum şi post-partum, având în vedere principalii factori de risc legaţi de vârstă. Materiale şi metodă. Obiectivul studiului a fost de a evalua un lot de 186 de paciente însărcinate care au fost internate în Spitalul Clinic de Obstetrică-Ginecologie „Prof. Dr. Panait Sîrbu”, Bucureşti, în decursul a 12 luni, pentru naştere. Studiul a avut ca obiectiv principal identificarea principalelor patologii asociate sarcinilor la vârste extreme. În cadrul analizei au fost incluse toate gravidele care la internare au prezentat vârsta cronologică mai mică sau egală cu 19 ani şi mai mare sau egală cu 39 de ani. În cadrul studiului a fost dezvoltată o metodă de cercetare cantitativă care a evaluat mai multe aspecte ce au conturat profilul medical al pacientelor. Rezultate. Analiza comparativă, pe categorii de vârstă, a datelor referitoare la patologiile asociate relevă faptul că prevalenţa diabetului zaharat şi a hipertensiunii arteriale a fost semnificativ mai ridicată în rândul gravidelor din grupa a doua de vârstă (39 de ani şi peste), în timp ce uterul cicatricial a avut o frecvenţă mai mare la gravidele din grupa de vârstă de maximum 18 ani. De asemenea, rezultatele studiului au mai indicat o frecvenţă mai mare a sarcinilor pierdute şi a restricţiilor intrauterine de dezvoltare a fătului în lotul pacientelor cu vârsta de 39 de ani şi peste. Concluzii. Rezultatele studiului sugerează necesitatea unor abordări de îngrijire distincte pentru cele două categorii, care să ţină cont de principalele aspecte identificate. În cazul pacientelor de maximum 18 ani, majoritatea aflate la prima sarcină, dar cu mai puţine implicaţii patologice, abordarea trebuie să includă o componentă educaţională mai accentuată (dată fiind lipsa de experienţă în creşterea şi îngrijirea nou-născutului), în timp ce, pentru categoria de 39 de ani şi peste, sunt necesare intervenţii specifice care să fie centrate pe îmbunătăţirea cunoştinţelor, atitudinilor şi practicilor moşelor şi asistenţilor medicali în ceea ce priveşte prevenirea şi acordarea îngrijirilor de sănătate pacientelor care prezintă riscul de a dezvolta aceste patologii asociate sarcinii. Implementarea programelor de educaţie sanitară în rândul adolescentelor poate fi de ajutor în asigurarea unei planificări adecvate şi în prevenţia sarcinilor nedorite la adolescente.Cuvinte Cheie
moaşeasistenţi medicaliîngrijiri de sănătatesarcină la vârstă avansatăadolescentă însărcinatăIntroduction
Pregnancy at an extreme age is a common medical condition today, probably due to the lack of sex education for adolescents and young girls or to social, economic or educational issues for women over the age of 35. Several studies have evaluated this situation and have shown that pregnancy at extreme ages can generate a number of important complications for the mother’s but also for the fetus’ health.
The literature defines advanced maternal age as the mother’s age of 35 years old or more at childbirth. This situation is common nowadays, the maternal age registering annual increases both in our country and in other countries. In the United States of America, maternal age increased significantly from 1970 to 2000, during which an increase in births among women over the age of 35 rose from 5% to 13%(1,2).
Numerous studies have concluded that a pregnancy which occurs at an advanced age can predispose a woman to a number of complications, such as preeclampsia, placenta praevia, gestational diabetes, premature birth or even neonatal death. The woman’s advanced age generates a certain degree of infertility, which is why patients address to assisted reproductive technology like in vitro fertilization with donated oocytes, a procedure that can lead to multiple pregnancies, premature births or increased maternal morbidity(3-5).
The results of a study conducted in Spain on a sample of 3315 births in 2014 indicated the association between advanced maternal age and the presence of repeated abortions and the increased risk of developing gestational diabetes, especially among primiparous women. Also, advanced maternal age has been associated with the need for caesarean section in both primiparous and multiparous women(2).
A systematic analysis conducted by Leader and co-workers regarding maternal and neonatal outcomes in mothers over the age of 35 indicated a 2.6-fold higher probability of losing the fetus. Thus, newborns from elderly patients were 2.49 times more likely to have a low Apgar score in the first 5 minutes.
Another study on pregnant women over the age of 35 showed a significant increase as regards the risk of developing hypertensive conditions, while the risk of caesarean delivery and gestational diabetes increased linearly with age. Another result of the study was that intrapartum mortality, neonatal mortality and infant mortality increase with maternal age from the age of 30 years old(6).
Similar results were obtained in another retrospective cohort study conducted by Arya and her colleagues in Texas. This study showed a higher incidence of gestational diabetes, pre-gestational diabetes, chronic hypertension, high blood pressure due to pregnancy, multiple pregnancies, oligohydramnios, polyhydramnios, placenta praevia, postpartum hemorrhage, low birth weight infants and gout(5).
Studies in teenage pregnancy have shown an increased risk of preterm birth(7). Premature labor, anemia and Chlamydia infection were the most common medical problems seen in adolescents under the age of 15, combined with poor prenatal monitoring(8). Recent studies have suggested that teenage pregnancies do not have as many complications as initially thought. However, the conclusion of a prospective cohort study, conducted by Goonewardene and Deeyagaha Waduge, and performed in a hospital in Galle, Sri Lanka, showed that pregnancies in adolescents, especially those under the age of 17, are at significantly higher risk of complications. Many of these pregnancies are unplanned and could be prevented through counseling programs(9).
Another healthcare problem reported by researchers in pregnant adolescents was depression. Multiple social, cultural and emotional factors can be involved in the onset of pregnancy, leading in some cases to unwanted or unplanned pregnancies. The conclusions of the study conducted by Pereira and his collaborators revealed that depression was more intense among early adolescents than among adolescents over 15 years old(10).
In Romania, statistical data indicate a significant number of births in the 15-19 age group, but also under the age of 15 years old. In 2019, 262 births were reported in urban areas among adolescents under the age of 15, while 5559 births were reported for the 15-19 years old age group. The study indicates that in rural areas these figures double, meaning there were 440 births in adolescents under 15 years old and 11,428 births in the age group of 15-19 years old(11).
Another study, aimed to monitor pregnancies in adolescents in Romania, given the sociodemographic, educational and cultural profile of young women at risk of becoming mothers before the age of 18, identified the lack of a coherent policy and standards of practice of healthcare professionals in the field of reproductive health, regarding adolescents. The study draws the attention to the lack of healthcare education programs offered to adolescents. Sex education in schools, at this time, is sporadically conducted and is optional, which is why it does not ensure the systematic transmission of the necessary information to ensure safe sexual behavior in order to prevent unwanted pregnancies. Another issue reported in this study was the lack of standards for counseling adolescents, especially those from disadvantaged environments, but also the lack of professionals with clear responsibilities in counseling adolescents on contraception. The number of healthcare professionals trained in the field of contraception in adolescents and in family planning is inadequate, due to the lack of specific training programs that can be attended by staff with basic medical training, such as doctors, midwives, nurses etc.(12)
Midwives and nurses are the professionals with the most appropriate training and position in the healthcare systems who can disseminate the information needed to prevent unwanted pregnancies or to identify early signs of the most common complications of pregnancy at an extreme age. One of the core responsibilities of midwives and nurses is health education and the provision of quality information and family planning counseling, thus facilitating actions to protect health in groups considered at risk(13).
Given the risks to the health of the mother and the newborn, the study aims to identify the main pathologies associated with pregnancy at extreme ages, in order to develop a series of training materials for midwives, nurses and mothers.
Methodology
The aim of the study was to identify the most common pathologies that can affect patients with extreme age pregnancies, in order to develop specific training programs for nurses and midwives and to create healthcare protocols adapted to the identified pathologies, as well as medical education guides for patients.
This research started the analysis from the hypothesis that pregnancy at extreme ages is associated with significant maternal and fetal outcomes.
In this retrospective study, two reference groups were formed for which the medical information coming out from the observation sheets was collected. The first group consisted of all pregnant patients who gave birth in the “Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology aged between 14 and 19 years old. The second group consisted of patients aged 39 or older. The study included in the analysis 77 patients aged ≤19 years old and 109 patients aged ≥39 years old, hospitalized between 1.01 and 31.12.2019.
Although advanced maternal age was considered to be the mother’s age of 35 years or older, our study included mothers aged 39 or older, based on the results of previous research which showed that increased maternal age is associated with several maternal and fetal complications(2,14). The study included only patients who were hospitalized in the “Prof. Dr. Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology for childbirth, excluding patients who were hospitalized for another type of care.
A quantitative research method was used which collected and analyzed data on: age of patients, parity, gestation, the method by which the pregnancy was obtained, type of birth, pathologies associated with gestation, treatments performed during pregnancy, the presence of other maternal and neonatal complications, fetal birth weight, premature birth and newborn Apgar score.
Results
1.1. Ethical considerations
The study was conducted based on the approval of the Ethics Commission of the “Panait Sîrbu” Clinical Hospital of Obstetrics and Gynecology. The patients signed an informed consent at hospitalization asking for their consent for processing medical data in order to improve healthcare management. The patients were assured of the anonymity of the data processed, and they were informed that they could refuse the data collection for scientific purposes.
1.2.Results – statistical analysis of data
The data obtained were processed using the SPSS 20.0 program, using both descriptive (frequency) and inferential statistics (calculation of the chi-square coefficient, to establish the significance of differences recorded according to the age category of patients).
1.2.1. Age distribution of pregnant patients included in the study
The study included 77 pregnant patients aged 14-19 years old and 109 pregnant patients aged 39 to 50 years old (Figures 2 and 3).
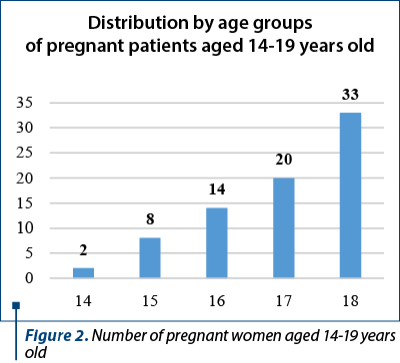
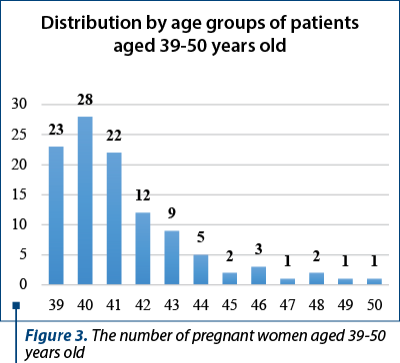
As it can be seen from Figures 2 and 3, the number of pregnant adolescent patients increases with age, while in the case of patients aged between 39 and 50 years old, the number decreases with increasing age.
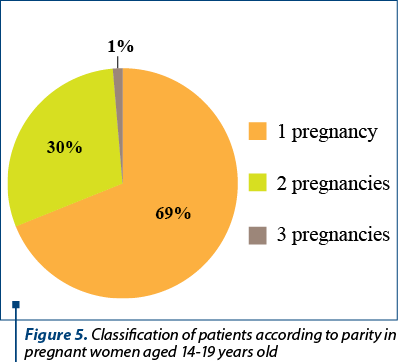
In the case of adolescent patients, it can be seen that 69% had one pregnancy in history, 30% had two pregnancies, while 1% of the total number of patients had three previous pregnancies.
Comparative analysis of data on age category and periods of gestation and birth
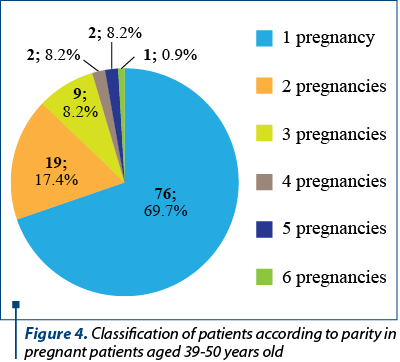
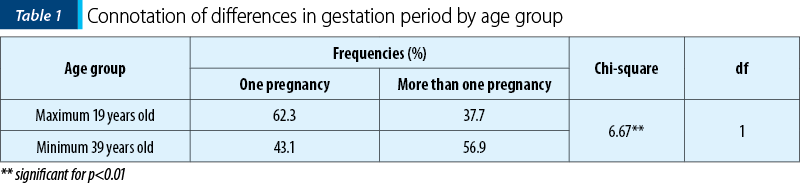
The comparative analysis of the data collected on the percentages of multiparous pregnant women in the age group over 39 years old is significantly higher than among those up to 19 years old (Table 1).
1.2.3. Analysis of data on the existence of lost pregnancies in the two groups included in the study
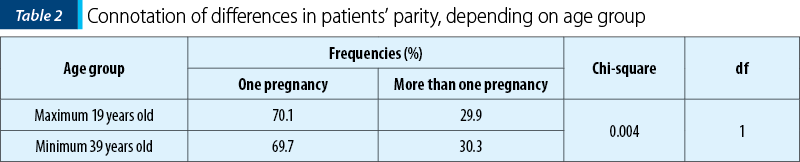
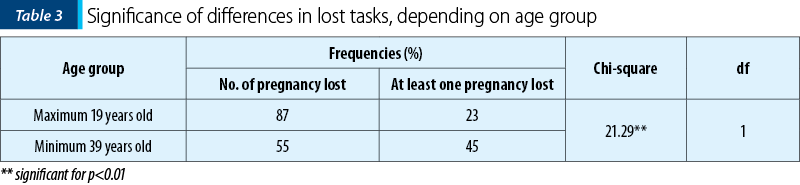
Data processing indicates that the percentages of pregnant patients at first birth are approximately similar in the two groups (Table 2), which is explained by the significantly higher frequency of missed pregnancies among those of at least 39 years old (Table 3).
As it results from Table 4, for the age group up to 19 years old, the pregnancies were obtained entirely by natural means, while in the case of the 39 years and over category, almost half of the pregnancies (43.1%) were the result of in vitro fertilization.
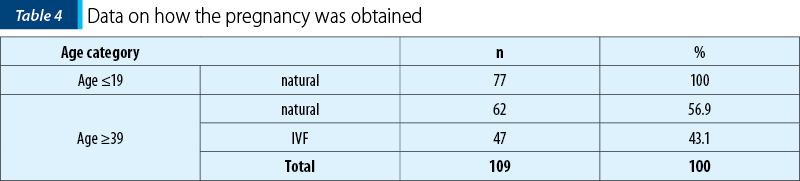
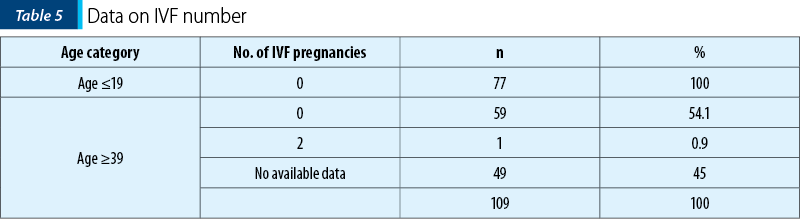
The information regarding the number of in vitro fertilizations is relatively incomplete (for 45% of patients aged 39 and over there is no information – Table 5).
1.2.3. Analysis of data on the presence of premature births and the presence of intrauterine growth restrictions in the fetus
Both prematurity and intrauterine growth restrictions in the fetus are complications caused by pregnancy at extreme ages, known and demonstrated in previous research.
Also, in our research, the percentage of premature infants was higher in pregnant women aged at least 39 years old (Table 6), as well as in the case of intrauterine growth restrictions of the fetus (Table 7).
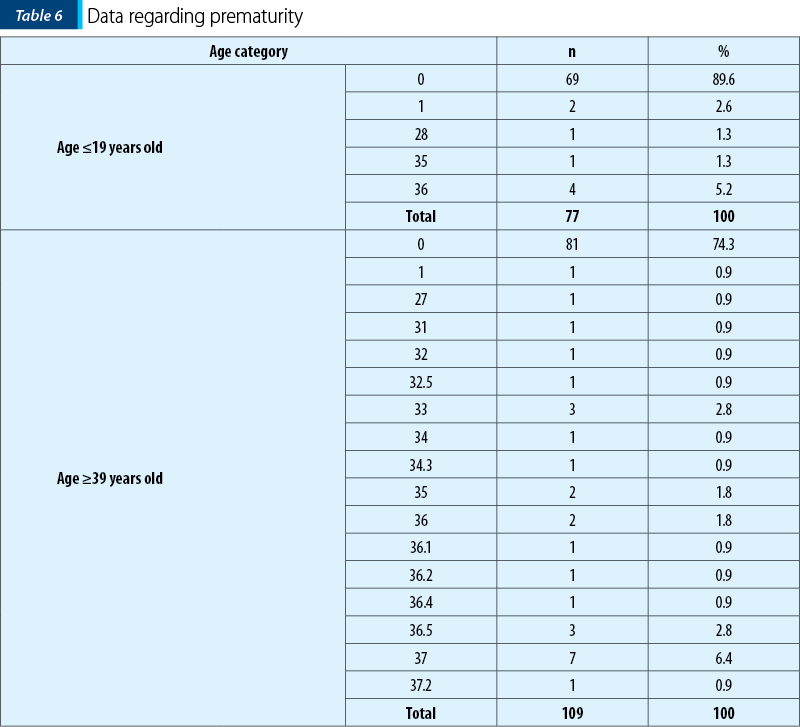
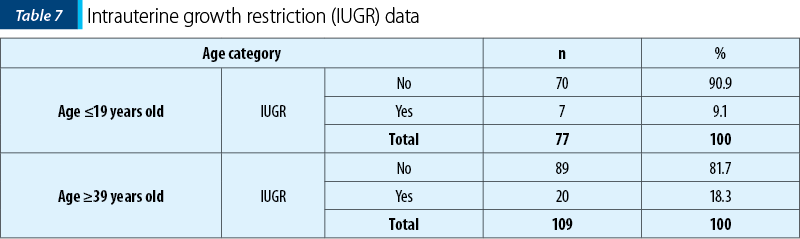
Intrauterine growth restriction is a condition that can be encountered during pregnancy; it might have several triggers and can be a major cause of fetal and neonatal morbidity and mortality. It can be seen that 18.3% of the patients within the over 39 years old group and 9.1% of the patients within maximum 18 years old group had a intrauterine growth restriction.
The presence of intrauterine growth restriction may predispose the newborn to several acute conditions, such as perinatal asphyxia, hypothermia, hypoglycemia and polycythemia. In the long run, these newborns may have complications in the form of growth retardation or neurodevelopmental difficulties(15).
The Apgar score is an important rapid test to assess the health of the newborn in the first 1-5 minutes after birth, in order to prevent infant mortality at birth(16).
As it can be seen, the Apgar scores obtained at birth vary between 7 and 10 (for the age group up to 19 years) and between 3 and 10 (for the age category 39 years and over) – Table 8.
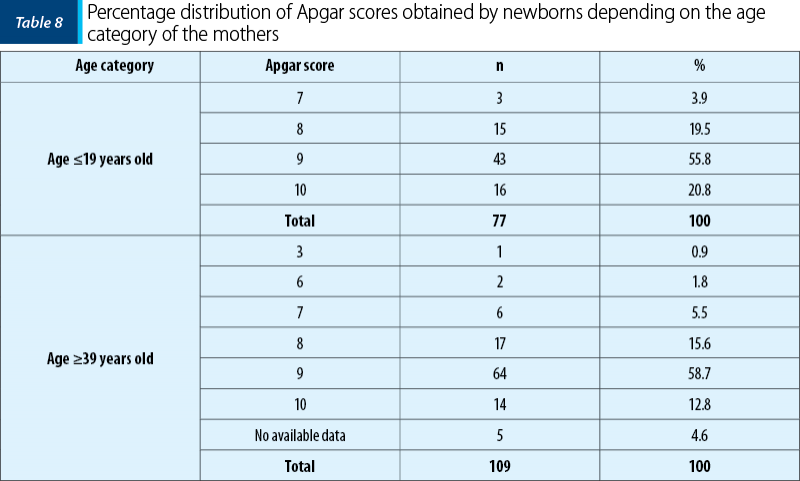
Data analysis on Apgar scores obtained by newborns from mothers up to 19 years old shows that 3.9% of newborns scored Apgar 7, 19.5% scored Apgar 8 and 76.6% of newborns received an Apgar score of 9 and 10.
The situation is slightly different for patients over the age of 39, where it can be seen that only 12.8% of the newborns obtained an Apgar score of 10, while 0.9% obtained an Apgar score of 3, 1.8% obtained an Apgar score of 6, 5.5% obtained an Apgar score of 7, 15.6% obtained an Apgar score of 8, and 58.7% obtained an Apgar score of 9, as it can be seen in Table 8.
1.2.3. Comparative analysis of data regarding associated pathologies, by age categories
The age category comparative analysis of the data regarding the associated pathologies revealed that the prevalence of diabetes was significantly higher among pregnant women in the second age group (39 years and over) – Table 9.
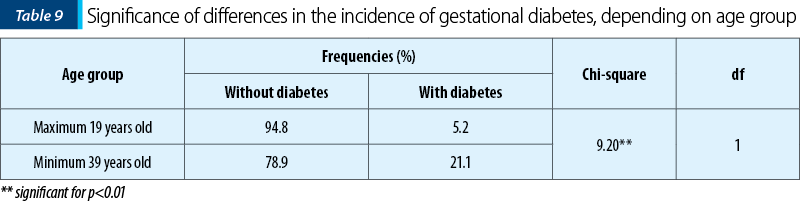
Gestational diabetes is an increase in the normal blood glucose level encountered in the second or third trimester of pregnancy. The presence of glycemic values that exceed the normal level in the first trimester of pregnancy is considered type 1 or type 2 diabetes. Implementing healthcare management protocols tailored to this health problem can help patients to prevent this condition by adopting a healthy lifestyle in which exercise, diet and rest are the main aspects that need to be taken into account.
Other complications associated with the evolution of pregnancy within the study group were found, such as anemia, urinary tract infections with various germs (Klebsiella, Streptococcus, Candida albicans, E. coli, Ureaplasma, MRSA, Trichomonas vaginalis), varicose veins, disease hemorrhoids, placenta praevia, thrombocytopenia, hypothyroidism, polyhydramnios, hepatic cytolysis, pelvic presentation, uterine fibroids, positive VDRL, HELLP syndrome, cholestasis, minor thalassemia, macrosome fetus, endometriosis and secondary uterine inertia.
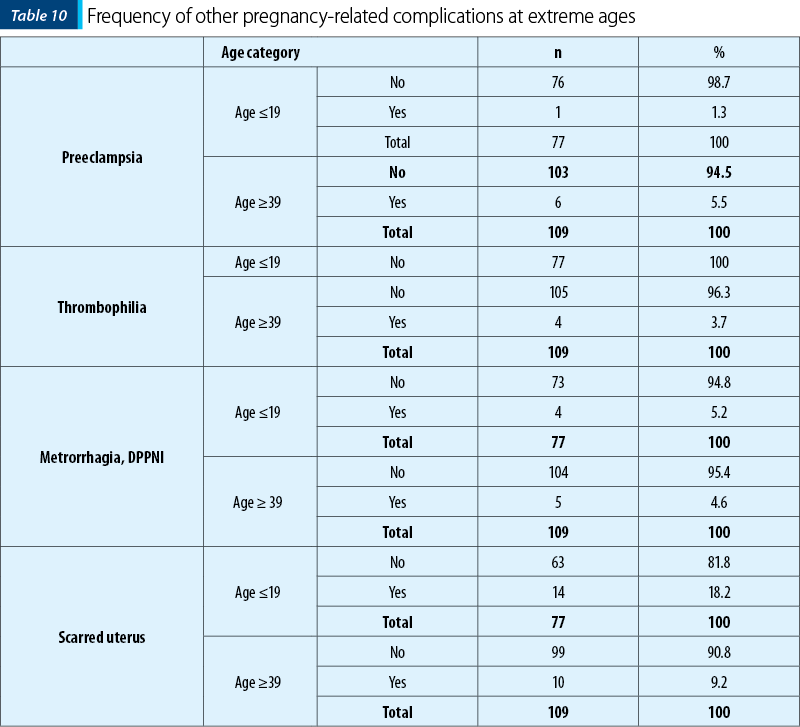
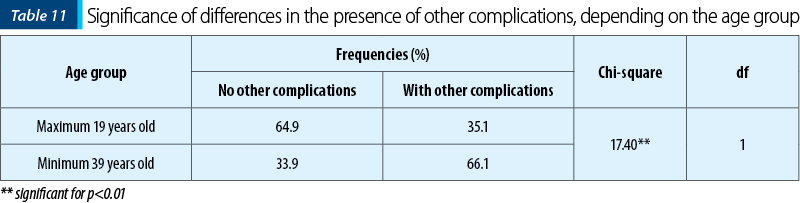
It can be noticed that, regarding the frequency of other diseases, the differences are not significant, the scarred uterus having a higher frequency in pregnant women in the up to 19 years old group. Also, situations in which there are no other complications associated with pregnancy are much more common among pregnant women up to 19 years old (64.9%), compared to those under 39 years old (33.9%).
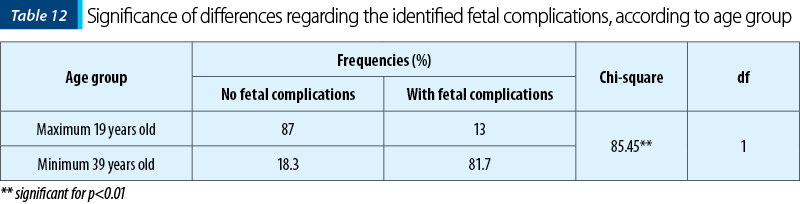
Data analysis indicates the presence of fetal complications that are significantly more common among newborns of mothers older than 39 years old compared to those occurring among mothers younger than 19 years old. The most common fetal complications reported in this study were: toxic erythema, neonatal jaundice, congenital hydrocele, allergic erythema, congenital crooked leg, fetal isoimmunization, hemangioma, hip dislocation, macrosome fetus, congenital lower limb deformities, transient metabolic disorders, fetal asphyxia.
Discussion
In this cohort study, the comparative analysis of the two groups evaluated the maternal results and the complications associated with the patients who constituted the two groups studied.
The findings of this study show that patients in the age group of ≥39 years old have a higher frequency of miscarriages and intrauterine growth restrictions, the latter being most likely associated with a higher frequency of premature births in the age group.
According to the results of this research, patients in the age group of ≥39 years old have a significantly higher presence of pregnancy-related medical conditions, and the newborns have various pathologies at birth, such as macrosomia, fetal asphyxia and prematurity. The results of our study are also confirmed in other similar studies performed on the perinatal and obstetric outcomes of patients older than 40 years of age(17-19).
Another study, developed by Ozalp and colleagues in 2003, also indicates poor obstetric results due to increased risk of chromosomal aneuploidies and the development of hypertension and gestational diabetes, conditions that lead to major pregnancy complications(20).
Our study highlights, retrospectively, the increased maternal and fetal risks in pregnancy among extreme age groups. Pregnancy counseling is essential for these age groups, so that a woman can make an informed decision about when to give birth.
Thus, we can conclude that the hypothesis of our study is confirmed in this research. Although pregnancy at extreme ages can be associated with significant maternal and fetal risks, old age cannot be considered a risk factor during pregnancy, childbirth and the postnatal period. Pregnancy complications among old maternal age pregnancies are not entirely due to age, but additional factors, such as chronic maternal disorders, lifestyle, parity and social environment, may adversely affect the proper course of the pregnancy(21).
Conclusions for clinical practice
The results of our research suggest the need for distinct approaches of healthcare for the two categories. Thus, in case of patients younger than 19 years old, most of them being at their first pregnancy/birth but with fewer pathological implications, healthcare planning offered by midwives and nurses should include a more pronounced educational component (given the lack of experience), while for patients included in the other group (≥39 years old), the healthcare plan should focus more on the prevention and treatment of pathological aspects associated with pregnancy, especially on the prevention of the most common pathologies, such as gestational diabetes, preeclampsia and pregnancy-induced hypertension, but also on the early detection of these diseases.
With regard to prevention actions in the adolescent age group, health education programs play a key role in preventing unwanted pregnancies. As recommended in the report “Pregnancy in adolescents in Romania”(12), the institutional collaboration of the main organizations in the field of health promotion and the multidisciplinary approach are essential in the projects development in order to promote public campaigns to prevent unwanted pregnancies and family planning, all addressed to sexually active adolescents.
Thanks. The authors would like to thank all those who supported the study: Ms. Ilona Voicu for her support in statistical data processing, Antonia Stroe for her English translation, and the assistants who supported the data collection and centralization process.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Cleary-Goldman J, et al. Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005;105(5):983–90.
-
Casteleiro A, Paz-Zulueta M, Parás-Bravo P, Ruiz-Azcona L, Santibañez M. Association between advanced maternal age and maternal and neonatal morbidity: A cross-sectional study on a Spanish population. PLoS One. 2019;14(11):e0225074.
-
Leader J, et al. The effect of very advanced maternal age on maternal and neonatal outcomes: a systematic review. J Obstet Gynaecol Canada. 2018;40(9):1208–18.
-
Londero AP, Rossetti E, Pittini C, Cagnacci A, Driul L. Maternal age and the risk of adverse pregnancy outcomes: A retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):261.
-
Arya S, Mulla ZD, Plavsic SK. Outcomes of women delivering at very advanced maternal age. J Women Health. 2018;27(11):1378–84.
-
Schummers L, et al. Absolute risks of obstetric outcomes risks by maternal age at first birth: A population-based cohort. Epidemiology. 2018;29(3):379–87.
-
Usta IM, Zoorob D, Abu-Musa A, Naassan G, Nassar AH. Obstetric outcome of teenage pregnancies compared with adult pregnancies. Acta Obstet Gynecol Scand. 2008;87(2):178–83.
-
Soula O, Carles G, Largeaud M, El Guindi W, Montoya Y. Pregnancy and delivery among adolescents under 15: a study of 181 cases in French Guiana. J Gynecol Obstet Biol Reprod (Paris). 2006;35(1):53–61.
-
Goonewardene IMR, Deeyagaha Waduge RPK. Adverse effects of teenage pregnancy. Ceylon Med J. 2005;50(3):116-20.
-
Pereira AB, Silva FMAM, Pereira DCA, et al. Depression and anxiety in pregnant adolescents. Women Health. 2019;8(2):154–7.
-
INS. Evenimente demografice în anul 2019. Available at: https://insse.ro/cms/sites/default/files/field/publicatii/evenimente_demografice_in_anul_2019.pdf
-
Nanu MI, Stativa E, Vălceanu D, Oţelea MR. Sarcina la adolescente în România. Available at: https://www.programsamas.ro/sarcina-la-adolescente-in-romania-raport/
-
MS. OUG 144/28. 2008 Oct.
-
Hinkle SN, et al. Differences in risk factors for incident and recurrent small-for- gestational-age birthweight: A hospital-based cohort study. BJOG An Int J Obstet Gynaecol. 2014;121(9):1080–9.
-
Sharma D, Shastri S, Sharma P. Intrauterine growth restriction: antenatal and postnatal aspects. Clin Med Insights Pediatr. 2016;10:67-83.
-
Karen Gill RN. Apgar Score: what you should know. Available at: https://www.healthline.com/health/apgar-score#normal-apgar-score.
-
Zapata-Masias Y, Marqueta B, Gómez Roig MD, Gonzalez-Bosquet E. Obstetric and perinatal outcomes in women ≥ 40 years of age: Associations with fetal growth disorders. Early Hum Dev. 2016;100:17–20.
-
Tebeu PM, Major AL, Ludicke F, Obama MT, Kouam L. Outcome of delivery at extreme ages of reproductive life. Rev Med Liège. 2004;59(7-8):455-9.
-
Simchen MJ, Yinon Y, Moran O, Schiff E, Sivan E. Pregnancy outcome after age 50. Obstet Gynecol. 2006;108(5):1084-8.
-
Ozalp S, Tanir HM, Sener T, Yazan S, Keskin AE. Health risks for early (≤19) and late (≥35) childbearing. Arch Gynecol Obstet. 2003;268(3):172–4.
-
Schildberger B, Linzner D, Hehenberger L, Leitner H, Pfeifer C. Influence of maternal age on selected obstetric parameters. Geburtshilfe Frauenheilkd. 2019;79(11):1208–15.




