Brain cancer during pregnancy is an unusual event, with a poor resolution due to its signs and symptoms that can be confused with those of pregnancy. Complications like infections and hemorrhages can occur due to multiple tumoral surgeries and these may represent another risk factor and can increase the morbidity and mortality. We present two cases of brain cancer during pregnancy which occurred in six months, between June 2021 and December 2021, in the Department of Obstetrics and Gynecology of the University Emergency Hospital, Bucharest. One of the most important facts we noticed in our cases was that both patients were very young (25 years old) and pregnant when the diagnosis was established. The histopathological exam revealed different results, as one of them was glioblastoma and the second one was anaplastic oligodendroglioma. The last one needed multiple interventions due to complications. In both cases, the newborns had a favorable evolution and the patients began radiotherapy after delivery.
Managementul neoplaziei cerebrale în timpul sarcinii
Management of cerebral neoplasia during pregnancy
First published: 31 mai 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.36.2.2022.6556
Abstract
Rezumat
Cancerul cerebral în timpul sarcinii este o patologie rară, cu un prognostic rezervat, din cauza semnelor şi simptomelor care pot fi confundate cu cele din sarcină. Complicaţiile precum infecţiile şi hemoragiile pot apărea ca urmare a multiplelor intervenţii chirurgicale şi pot reprezenta un factor de risc adiţional care duce la creşterea morbidităţii şi mortalităţii. Prezentăm două cazuri de cancer cerebral în timpul sarcinii, apărute în cursul a şase luni, între iunie şi decembrie 2021, în cadrul Departamentului de obstetrică şi ginecologie al Spitalului Universitar de Urgenţă din Bucureşti. O caracteristică importantă observată în cazurile studiate de noi este vârsta tânără, ambele pacientele având 25 de ani şi fiind gravide la momentul diagnosticului. Formele anatomopatologice au fost diferite, unul fiind diagnosticat ca glioblastom, iar cel de-al doilea, ca oligodendrogliom anaplazic. Cel din urmă caz a necesitat multiple intervenţii ca urmare a complicaţiilor apărute. În ambele cazuri, nou-născuţii au avut o evoluţie favorabilă, iar pacientele au început radioterapia după terminarea sarcinii.
Introduction
Neoplasia represents an important health problem, with a high mortality rate all over the world, but it is rarely diagnosed during pregnancy, with an incidence between 0.07% and 0.1% of all cancers(1). The finality of the case depends on several factors, such as age, health status of the mother, gestational age, social and demographic factors, and the stage of the disease when diagnosed(2,3). The treatment plan should not be significantly different from the one in the general population, but the pregnancy condition can delay or contraindicate some medical procedures or treatments due to the side effects that can affect the fetus(4).
Regarding the brain malignant tumors, they have an incidence of 7 per 100,000 person-years in Europe, and a rate of mortality of 5.4 per 100,000 person-years(5,6). Multiple risk factors for cerebral neoplasia, especially environmental ones, have been studied, but the only one which is recognized by the International Agency for Research on Cancer is the ionizing radiation, classified as carcinogen(5).
As in nonpregnant age-matched women, during pregnancy cerebral cancer is the rarest malignancy(7-9). It is well known that cerebral neoplasia may be very different in what concerns the anatomopathological subtype, therefore the prognostic and the treatment may be various. Certain types of cerebral tumors have been reported, which leads to the conclusion that they are more often encountered during pregnancy, such as: meningioma, astrocytoma, schwannoma, pituitary adenoma and breast cancer metastasis(7,10,11).
Glioblastoma is considered to be one of the most common brain tumors, but it is the deadliest primary cerebral malignancy(7,12). There had been some cases of glioma reported in pregnant women, but it has not been established whether pregnancy influences the oncogenicity of the tumor or not(7,13).
Anaplastic oligodendroglioma, a rare malignant cerebral tumor, represents 0.5% of all brain neoplasias. During pregnancy, it is extremely rare(14).
No matter what subtype of cerebral neoplasia we are referring to, the symptomatology seems to be common and includes: headache, visual changes, hemiparesis or seizures(10). Due to these symptoms during pregnancy, a brain tumor can be easily omitted. It is especially important to make the differential diagnosis with preeclampsia, eclampsia or epilepsy. In the moment we exclude other pathologies, a non-contrast MRI should be performed because it represents the best modality for brain tumor imaging during pregnancy and it is accepted by the American College of Obstetricians and Gynecologists and by the American College of Radiology(7,11,15).
The management of cerebral tumors consists in the resection of the entire tumor, if it’s possible, or most of it, followed by radiotherapy and, as a second step, chemotherapy(14). Even though neurosurgery during pregnancy presents more risks, it is accepted and it can have positive results. Radio- and chemotherapy can be complicated by the risk of safe maintenance of pregnancy, this is why the patients should be informed about the risks and the benefits(7). A psychologist should advise and counsel both parents about the neonatal and mother’s prognosis.
Cases report
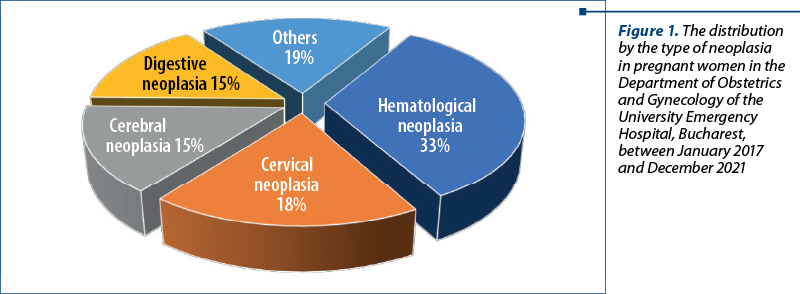
We present two cases of brain cancer during pregnancy which occurred in six months, between June 2021 and December 2021, in the Department of Obstetrics and Gynecology of the University Emergency Hospital, Bucharest. We have to mention that in the last five years there have been 19 patients with neoplasia who gave birth in our department (0.15% of all births in our unit). Also, cerebral cancer represented the third type of cancer in pregnant women; the first two ones were hematological and cervical cancer (Figure 1). In the category “Others”, we included breast neoplasia, bone neoplasia and choriocarcinoma.
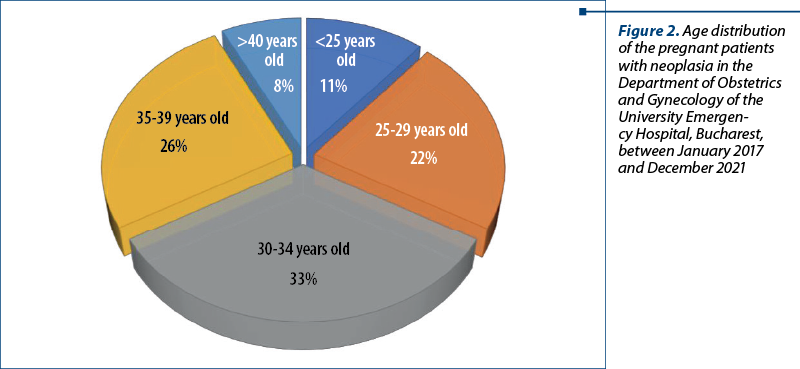
For this analyzed period, we also evaluated the frequency of cancer according to age distribution and we concluded that in the group of 30-34 years old we had the most cases of neoplasia during pregnancy (Figure 2).
Case 1
We present the case of a 25-year-old patient who was admitted in the Department of Obstetrics and Gynecology of the University Emergency Hospital, Bucharest, transferred from the Department of Obstetrics and Gynecology of the Slatina Emergency County Hospital, for a massive cerebral tumor and with pregnancy in 36-37 weeks. She was gravida 1, para 1. She had a Body Mass Index (BMI) of 22.4, non-smoker and non-hypertensive. She underwent all antenatal consultations and did not have any infections or other pathologies associated to pregnancy. The patient had no significant personal pathological history. Neither did her family had any medical record.
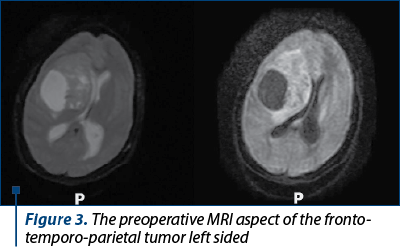
Her symptomatology started two weeks before the diagnosis and was represented by intense headaches, diplopia and left facial paralysis. In the Slatina Emergency County Hospital it was performed a cerebral MRI that established the diagnosis of massive cerebral tumor with left frontotemporal location. At the time she was transferred to our hospital, the patient was stable and underwent multidisciplinary consultations – obstetrical, neurological and neurosurgical. The patient was evaluated clinically and paraclinically, including blood samples, urinary samples, cervical and vaginal samples. We repeated the cerebral MRI which confirmed the previous diagnosis (Figure 3).
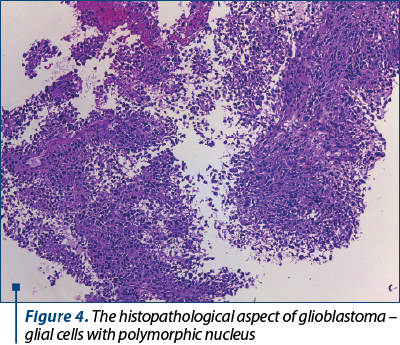
The next day, a multidisciplinary team formed by obstetricians, neurosurgeries and anesthetists’ physicians decided to perform a caesarean section, being extracted a male newborn (weigh 2.860 grams, Apgar score of 8 at 1 minute) and, at the same time, it was conducted the neurosurgery intervention. The cerebral tumor that was extirpated was sent to extemporaneous examination and the result was glioblastoma (Figure 4).
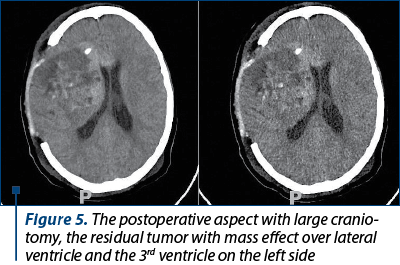
During the hospitalization, the mother benefited from psychological evaluation. The post-surgery evolution was favorable both for the mother and the newborn, and they were released after 10 days. The neurological symptomatology was ameliorated, with diplopia and left facial paralysis submitted. The postoperative control performed by MRI imaging was improved (Figure 5). After 30 days of the surgery, the patient started radiotherapy and polychemotherapy. Nowadays, the patient is under follow-up care.
Case 2
We present the case of a 25-year-old patient who showed up at the Emergency Room of the Bucharest University Emergency Hospital and accused intense headaches, muscle force loss for right limbs and recent installed language disorder. She was gravida 2, para 2, and she had 22-23 weeks of pregnancy. She had a Body Mass Index (BMI) of 21.1, non-smoker and non-hypertensive. She underwent all antenatal consultations until this gestational age and she did not have any infections or other pathologies associated to pregnancy. The patient did not have significant personal pathological history and neither did the family had any medical record. The first newborn was delivered by caesarean section due to fetal dystocia.
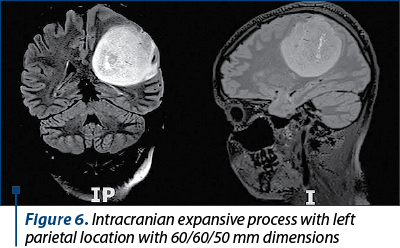
She underwent multidisciplinary examinations, including obstetrical and neurological which revealed left hemicrania, right hemiparesis and elements of motor aphasia. A cerebral MRI was also performed, being established the diagnosis of massive cerebral tumor with left parietal location (Figure 6). She was admitted in the Neurological Department of the University Emergency Hospital, Bucharest. The patient was evaluated clinically and paraclinically, including blood samples, urinary samples, cervical and vaginal samples.
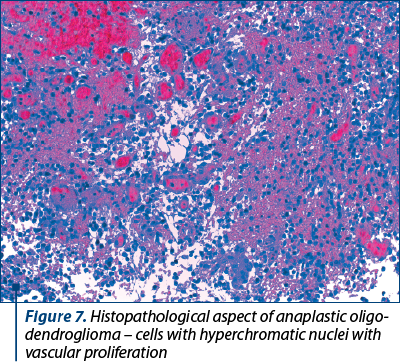
After three days of hospitalization, the neurosurgery team decided to perform the intervention with the extirpation of the infiltrative tumor. The histopathological result was anaplastic oligodendroglioma (Figure 7).
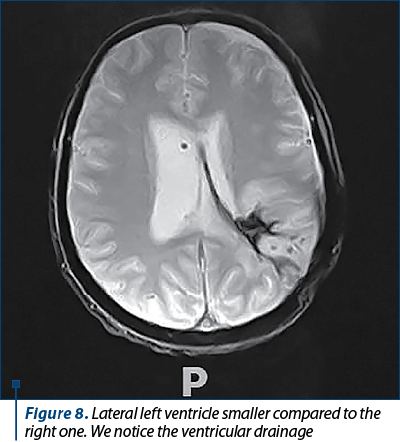
In the next 45 days, the patient needed seven more surgeries due to postoperative complications. The first three surgeries were done for uncal herniation syndrome and hemorrhagic complications. After these interventions, the patient was stable. The other four surgeries were performed for left parietal abscess and acute hydrocephaly which needed right external ventricular drain. The patient needed multiple antibiotic treatments, corticosteroids and anti-inflammatories medication. At the last intervention, it was removed the external ventricular drain and was set a right ventriculoperitoneal shunt (Figure 8).
Regarding the obstetrical status, the pregnancy evolved, but there were noticed the decrease of amniotic fluid and an intrauterine growth restriction, maybe due to multiple interventions, anesthesia and drugs.
The patient benefited from psychological counseling during the entire period of hospitalization. After more than two months from the moment the patient had been admitted in our hospital, she was presented to the Oncological Border of the University Emergency Hospital, Bucharest, and, because the patient’s neurological status was favorable, the team indicated caesarean delivery and the starting of the oncological treatment, with radio- and chemotherapy, as soon as possible.
The next day, the patient was transferred to the Department of Obstetrics and Gynecology of the University Emergency Hospital, Bucharest, and caesarean section was performed, being extracted a female newborn (weight 1.520 grams, with an Apgar score of 6 at 1 minute). The newborn was admitted in the neonatal intensive care and her evolution was favorable. The mother was released 10 days after she gave birth and she started the radiotherapeutic treatment. Nowadays she is under follow-up care. The newborn needed prolonged intensive care and she was released after 30 days.
In both cases, the patients signed the consents for medical and surgery treatments and for using their data in medical research purpose.
Discussion
A review analyzed 122 cases of glioma during pregnancy. The data were extracted from 65 reports published between 1999 and 2020(16). There were some interesting conclusions, such as: the median age when diagnosed with malignant tumor was 30 years old and it was established almost equal in every trimester of pregnancy. The main symptomatology was represented by signs of intracranial hypertension, seizures or focal neurologic deficits. Regarding the histopathological result, the most frequent tumors were: glioblastoma, anaplastic astrocytoma, and anaplastic oligodendroglioma(16). Also, signs and symptoms of any type of neoplasia may mimic those of pregnancy, such as fatigue, anemia, nausea or breast changes(17,18).
A study that took place between 2009 and 2019 in a university hospital in California analyzed nine patients who were diagnosed with neoplasia during pregnancy(10). In this study, the median age when the pregnant women had been diagnosed with malign tumor was 29 years old. The main symptomatology was represented by headache, neurovisual disorders, paresthesia or seizures(10).
In our cases, the patients were both 25 years old when they were diagnosed with brain cancer, younger than these from breadth studies. Regarding symptomatology, our patients presented the typical neurological signs and symptoms that are seen in brain tumors, even in non-pregnant patients. This symptomatology is very important to be noticed as soon as possible, because it may have a negative impact if the diagnosis is delayed. The diagnosis in both cases was established in the third trimester and the MRI remains the best method for brain tumors imaging in these patients. As we have seen, there is a variety of anatomopathological forms of brain tumors even in pregnant women. In our cases, the histopathological results were glioblastoma and anaplastic oligodendroglioma.
According to the risk factors, as we showed before, only the ionizing radiation is classified as carcinogen, while others – like N-nitroso compounds, pesticides, outdoor air pollution or radiofrequency electromagnetic waves – were just studied, but not established as being carcinogens(5). None of our patients was exposed to ionizing radiation, as far as we were informed.
Although there are a lot of anatomopathological types of brain tumors, the oncological treatment consists in surgery with tumor extirpation completed by radio- and chemotherapy. In the review which analyzed 122 cerebral neoplasias during pregnancy, there were 20 pregnant women who received after surgery radiotherapy, chemotherapy or a combination of them. An interesting result is than none of the patients who was exposed to radio- or chemotherapy during pregnancy had experienced intrauterine fetal death(16). These outcomes should be further analyzed.
Conclusions
Neoplasia during pregnancy is a rare event, and brain cancer is even less often encountered. However, we should be very aware of this pathology every time we have signs and symptoms that cannot be associated with pregnancy. It is safer to perform an MRI imaging during pregnancy than delaying the diagnosis. Cerebral neoplasia during pregnancy requires psychological counseling, multidisciplinary team and personalized treatment. For these reasons, neonatal prognosis is favorable most of the times. The mother’s outcome depends on the histopathological result, but the basic treatment is represented by surgery followed by radio- and chemotherapy.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Dur-e-Shahwar SI, Islam ZS, Sheikh L. Impact of pregnancy on cancer survival: Experience at a tertiary care hospital. Pak J Med Sci. 2021;37(2):335.
-
Blumenthal DT, Parreño MGH, Batten J, Chamberlain MC. Management of malignant gliomas during pregnancy: a case series. Cancer. 2008;113(12):3349-54.
-
Stupp R, Hegi ME, Van Den Bent MJ, Mason WP, Weller M, Mirimanoff RO, Cairncross JG, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups and the National Cancer Institute of Canada Clinical Trials Group. Changing paradigms – an update on the multidisciplinary management of malignant glioma. Oncologist. 2006;11(2):165-80.
-
Basta P, Bak A, Roszkowski K. Cancer treatment in pregnant women. Contemp Oncol (Pozn). 2015;19(5):354-60.
-
Vienne-Jumeau A, Tafani C, Ricard D. Environmental risk factors of primary brain tumors: A review. Rev Neurol (Paris). 2019;175(10):664-78.
-
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JWW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374-403.
-
Gatson NTN. Managing central nervous system tumors during pregnancy. Continuum (Minneap Minn). 2022;28(1):122-46.
-
Haas JF, Jänisch W, Staneczek W. Newly diagnosed primary intracranial neoplasms in pregnant women: a population-based assessment. J Neurol Neurosurg Psychiatry. 1996;49(8):874-80.
-
Simon RH. Brain tumors in pregnancy. Seminars in Neurology. 1988;8(3):214-21.
-
Rodrigues AJ, Waldrop AR, Suharwardy S, Druzin ML, Iv M, Ansari JR, et al. Management of brain tumors presenting in pregnancy: A case series and systematic review. Am J Obstet Gynecol. 2021;3(1):100256.
-
Gatson NTN, Boccia ML, Taylor KR, Mack JK, Fonkem E. Hormone-dependent tumors and sexuality in the neuro-oncology of women (NOW): women’s brain tumors, gaps in sexuality considerations, and a need for evidence-based guidelines. Curr Oncol Rep. 2021;23(11):127.
-
Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2013–2017. Neuro Oncol. 2020; 22(Suppl 1):iv1-iv96.
-
Somma T, Baiano C, Santi L, Sabatino G, Della Pepa GM, La Rocca G, et al. Diffuse low grade glioma and pregnancy: Practical considerations and clinical tips. Clin Neurol Neurosurg. 2020;198:106110.
-
Shin DW, Lee S, Song SW, Cho YH, Hong SH, Kim JH, Kim HS, Park JE, Nam SJ, Kim YH. Survival outcome and prognostic factors in anaplastic oligodendroglioma: A single-institution study of 95 cases. Sci Rep. 2020;10(1):20162.
-
ACOG Committee on Obstetric Practice. Committee Opinion No. 723: Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2017;130(4):e210-e216.
-
Van der Vegt AN, de Vries R, Osinga J, Grun N, Postma TJ, de Haan PF, et al. P14.51 Can patients with a suspected high-grade glioma receive tumor treatment during pregnancy safely? Neuro Oncol. 2021;23(Suppl 2):ii47-ii47.
-
Silverstein J, Post AL, Chien AJ, Olin R, Tsai KK, Ngo Z, Van Loon K. Multidisciplinary management of cancer during pregnancy. JCO Oncology Practice. 2020;16(9): 545-57.
-
Secară D, Uzunov AV, Baroş A, Andreescu AV, Edu A, Mehedinţu C, Carp-Velişcu A, Cîrstoiu MM. Challenges of the management of cancer in pregnant women during the COVID-19 pandemic. Rom J Med Pract. 2021;16(Suppl 6):69-74.
Articole din ediţiile anterioare
Testul de sarcină
Deşi sarcina poate fi detectată la scurt timp după concepţie, poate nu bănuiţi că sunteţi gravidă sau vă puneţi întrebări numai după absenţa menstr...
Utilizarea testelor prenatale neinvazive în evaluarea riscului de aneuploidii fetale în sarcina gemelară cu un embrion oprit în evoluţie în trimestrul I
Testele neinvazive prenatale sunt teste care analizează ADN-ul fetal din sângele matern şi stabilesc riscul de aneuploidii fetale, analizând cromoz...
Constatări ultrasonografice ale hipotiroidismului în timpul sarcinii
Hipotiroidismul este cea mai frecventă patologie endocrină care apare în timpul sarcinii. La nivel global, cel mai des întâlnită cauză pentru hip...
O singură inimă nu e de ajuns – gemeni conjuncţi: diagnosticul prenatal şi evaluarea malformaţiilor asociate. Prezentare de caz
Incidenţa sarcinilor multiple a crescut de-a lungul timpului datorită îmbunătăţirii tehnicilor de reproducere asistată şi reprezintă de obice...