Premature labor is the greatest cause of death for children under 5 years old worldwide. The etiology of preterm labor is often unknown. Some concepts that explain the causes of premature labor are basically always associated with the incidence of infections in the amniotic fluid, utero-placental ischemia, excessive uterine strains, endocrine disorders, and abnormal immune responses from the mother and fetus. Vitamin D plays an important role as an antiinflammatory and antimicrobial agent, so the purpose of this study is to examine the role of 25-hydroxyvitamin D (25(OH)D), which can prevent preterm labor. This is a literature review of related studies. Vitamin D functions in the regulation of calcium and phosphate in the blood. Some studies also explain that vitamin D has a function in regulating the immune system, participating in mitosis and cell differentiation, in the expression of nitric oxide synthesis (NOS), glutathione synthesis and neurotrophic factors. Low vitamin D levels have been shown to be significantly associated with an increased risk of preterm birth in several countries such as India and China. Vitamin D has a significant role in the mechanism of preterm labor.
Rolul 25 hidroxivitaminei D (25(OH)D) în travaliul prematur
The role of 25-hydroxyvitamin D (25(OH)D) in preterm labor
First published: 18 aprilie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/ObsGin.67.1.2019.2296
Abstract
Rezumat
Travaliul prematur este cea mai importantă cauză de deces în cazul copiilor sub 5 ani, la nivel mondial. Etiologia travaliului prematur este adesea necunoscută. Unele concepte care încearcă să explice cauzele travaliului prematur sunt de obicei întotdeauna asociate cu incidenţa infecţiilor lichidului amniotic, ischemia utero-placentală, tulpini uterine excesive, tulburări endocrine şi răspunsuri imunitare anormale ale mamei şi fătului. Vitamina D are un rol important antiinflamator şi antimicrobial, astfel încât scopul acestui studiu este de a examina rolul 25 hidroxivitaminei D (25(OH)D), care ar putea împiedica travaliul prematur. Articolul este un review al studiilor din literatură referitoare la acest subiect. Vitamina D reglează nivelul calciuliu şi fosfatului din sânge. Unele studii explică, de asemenea, că vitamina D are un rol în reglarea sistemului imunitar, participând la mitoză şi în diferenţierea celulară, în expresia sintezei oxidului nitric (SON), în sinteza glutationului şi a factorilor neurotrofici. Niveluri scăzute ale vitaminei D au fost asociate în mod semnificativ cu un risc crescut de naştere prematură în câteva ţări, precum China şi India. Vitamina D joacă un rol important în mecanismul travaliului prematur.
Introduction
Preterm labor is a labor that occurs before reaching 37 weeks of gestation. The incidence of preterm labor in 2010 around the world was about 7.5% (2 million births), and then increased in 2015 to 8.6% (2.2 million births), the incidence rate varying between 5% and 25% in different countries. In many developing countries, the incidence of preterm labor is much higher(1). Preterm labor accounts for 60-80% of the causes of neonatal mortality and for about 75% of cases of neonatal morbidity(2). The mechanism of preterm labor is generally divided into four mechanisms: infection and inflammation, premature activation of the hypothalamic pituitary fetal axis, mechanical stretching, and decidual bleeding(1,2). Data shows that 1,25(OH)2D helps the implantation process and maintains a normal pregnancy, and contributes to fetal growth by transporting calcium, controlling the secretion of various placental hormones and limiting proinflammatory cytokines(3). The general population and pregnant women have adequate vitamin D status, with serum 25-hydroxyvitamin D concentrations greater than 50 nmol/L (or 20 ng/mL)(4). The standard requirement for vitamin D during pregnancy is 400 IU/day in accordance with the estimated average requirement (EAR) and 600 IU/day in accordance with recommended dietary allowance (RDA).
Vitamin D
Vitamin D is also known as calciferol. Vitamin D is a group of fat soluble steroids that are responsible for increasing the absorption of calcium, magnesium and phosphate in the intestine, and has several other biological effects. Vitamin D1 is a mixture of ergocalciferol with lumisterol with a ratio of 1:1, vitamin D2/ergocalciferol is made from ergosterol, vitamin D3/cholecalciferol is made from dehydrocholesterol in the skin, and vitamin D4/22-dihydroergocalciferol and vitamin D5/sitocalciferol are made from 7-dehydrositosterol. In humans, the most important compounds are vitamins D2 and D3. The main source of natural vitamin D is the synthesis of cholecalciferol in the skin (derived from cholesterol through chemical reactions) which depends on sun exposure (especially ultraviolet B [UVB] radiation). Cholecalciferol is converted in liver into 25-hydroxycholecalciferol (calcifediol) and ergocalciferol is converted into 25-hydroxyergocalciferol. Both of these vitamin D metabolites – called 25-hydroxyvitamin D or 25(OH)D – are measured in serum to determine the vitamin D status of a person(5).
Vitamin D receptor (VDR) exists in almost all tissues and cells in the human body, so that 1,25(OH)2D will have many other biological roles in the tissue or cell, one of them being to stimulate the production of cathelicidin macrophages which play a role in the immune system fight against infections. Cathelicidin is an antimicrobial peptide that is primarily stored in lysosomes of macrophages and polymorphonuclear leukocytes (PMNs). Vitamin D deficiency is closely correlated with an increased incidence of infections. Cathelicidin was originally found in neutrophils, but can also be found in many other cells, including epithelial cells and macrophages after being activated by bacteria, viruses, fungi or hormones(5).
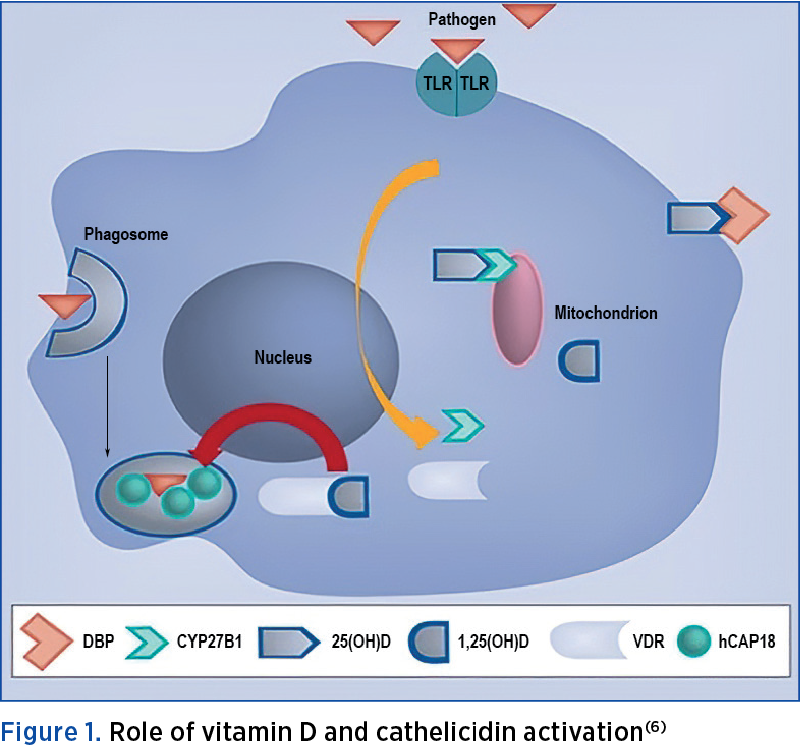
In Figure 1, it is explained that when pathogens are detected by each Toll-like receptor (TLR), VDR induction and CYP27B1 gene expression will appear. This results in a transformation process by 1--hydroxylation at 25(OH)D, whose source is derived from the blood (in complexes with vitamin D binding protein) and then the VDR will bind 1,25(OH)2D. The cathelicidin gene will be activated and will produce protein (hCAP18/LL-37) to be used against the pathogen that has been ingested by phagosomes in macrophages(6).
Physiology and metabolism of vitamin D in pregnant women
The aims of vitamin D homeostasis during the pregnancy process are to meet two important needs, which are to ensure normal delivery without complications, and optimal uterine conditions for the fetus to stay alive. The existing data shows that 1,25(OH)2D helps the implantation process and maintains a normal pregnancy, and contributes to fetal growth by transporting calcium, controlling the secretion of various placental hormones and limiting proinflammatory cytokines(3).
The typical adaptations of vitamin D homeostasis during pregnancy are increased maternal calcitriol, 25(OH)D availability for optimal maternal (OH)D status and elevated maternal vitamin D binding protein (VDBP) levels. These changes are clearly detected at the level of circulating systemic and placenta, suggesting that the placenta is a prime location for vitamin D metabolism in pregnancy(7).
The therapy with 1,25(OH)2D and 25(OH)D in human trophoblast cells has significantly altered the innate immune response. Natural killer (NK) cells in decidua given 1,25 (OH)2D (3) or 25-hydroxyvitamin D (3) (25OHD (3)) precursors for 28 hours show decreased synthesis of various cytokines, such as colony stimulating factor 2 (CSF2) granulocytes-macrophages, tumor necrosis factor (TNF) and interleukin 6 (IL-6), but increased mRNA expression for cathelicidin antimicrobial peptides(8).
Adequacy of vitamin D
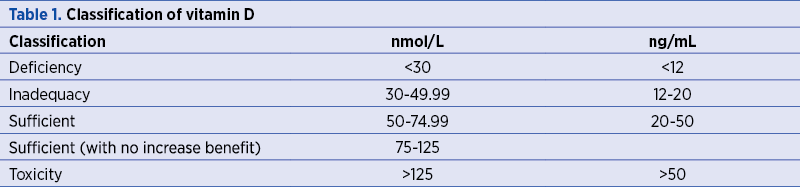
The Institute of Medicine from Washington defines the adequate vitamin D status as a serum 25-hydroxyvitamin D concentrations greater than 50 nmol/L (or 20 ng/mL) in both the general population and pregnant women, as presented in Table 1(4).
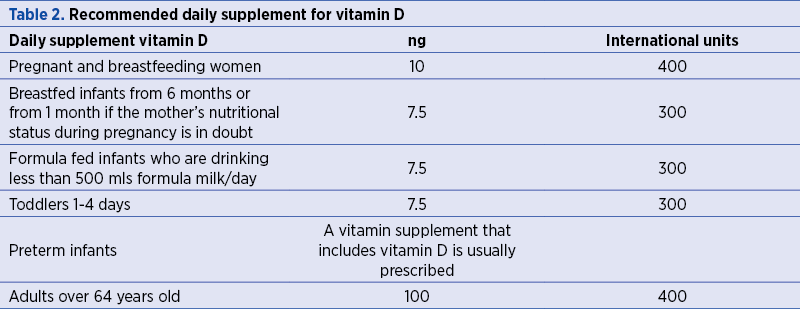
The standard requirement for vitamin D during pregnancy based on the guidelines of the Institute of Medicine (IOM) issued in 2010, as presented in Table 2, is 400 IU/day, in accordance with the estimated average requirement (EAR), and 600 IU/day in accordance with recommended dietary allowance (RDA). We also include the IOM 2010 recommendations for the classification of vitamin D deficiency(9).
Vitamin D deficiency can be caused by factors that inhibit its synthesis in the skin, by poor food consumption and other additional factors that affect its absorption or metabolism. Vitamin D insufficiency affects nearly 50% of the population worldwide. The etiology of increased rates of vitamin D deficiency may be multifactorial, but in part because of low vitamin D intake and limited exposure to sunlight(4,5). Vitamin D status is influenced by the factors that regulate its production in the skin, which affects its absorption or metabolism. Melanin acts as an ultraviolet (UV) filter, reducing the production of vitamin D to the skin, affecting populations with high melanin levels, such as Hispanic and black people(10).
In addition, the difference in latitude has also been shown to affect vitamin D concentrations. Individuals from countries with high and low latitudes tend to have lower vitamin D levels. The importance of UV light is further demonstrated by seasonal variation in vitamin D concentrations between summer and winter(11). Vitamin D levels tend to be higher during summer compared to winter periods. Vitamin D metabolism is also influenced by body mass index (BMI), where obese people tend to experience relative deficiency. Because of their lipid solubility properties, vitamin D tends to be stored in body fat depots, which lead to decreased bioavailability of vitamin D(11).
Vitamin D supplementation
25-hydroxyvitamin D is the main circulatory form of vitamin D, thus reflecting the level of intake of the skin and food. This molecule is also a precursor for 1,25-dihydroxyvitamin D, which is the most active vitamin D metabolite. 1,25-dihydroxyvitamin D cannot be used to measure vitamin D levels because its concentration can be affected by many factors(18). In general, vitamin D supplementation tables established by the UK health department can be used as a reference for adequate vitamin D intake(4).
Vitamin D as a predictor of preterm labor preterm
Over the past decade, studies have emerged which attempted to relate vitamin D deficiency in pregnancy with complications in maternal, fetal and neonatal disadvantages. Based on its epidemiology, as much as 50% of preterm deliveries can be attributed to infections(12). Vitamin D in the form of 1,25(OH)2D is known to reduce the bacterial infections by inducing cathelicidin in various tissues, including the maternal and fetal cells of the placenta. Other data from laboratory studies with randomized trials have shown a significant association between maternal vitamin D status measured by assessing maternal serum levels (25(OH)D) and the antibacterial responses of the placenta(6).
In addition to its role in the production of cathelicidin, vitamin D also stimulates the production of hydrogen peroxide secreted in human monocytes cells. The presence of oxidative enhancement activated by vitamin D can help cells to kill pathogenic organisms. Vitamin D activates the monocyte macrophage system to fight infections by pathogens such as Listeria and Group B Streptococcus, which are known to have a role in interrupting pregnancies, such as preterm birth(13).
Several clinical studies have found a significant correlation between vitamin D deficiency and preterm birth. Vitamin D deficiency during pregnancy increased the risk of preterm birth compared with mothers with adequate vitamin D intake (OR=1.29; 95% CI; 1.16-1.45)(14,15). The research on the population of pregnant women with inevitable abortion in Japan also showed that the majority of patients suffered from vitamin D deficiency(16). Furthermore, vitamin D concentrations are known to have a higher effect in influencing the process of partus. This is confirmed by the fact that vitamin D supplementation to maternal concentrations exceeding 40 ng/mL reduced the risk of preterm birth by 47%. However, not all studies showed significant results(17).
A 2017 meta-analysis tried to find out whether single vitamin D supplementation or 25 hydroxyvitamin D (25-OHD) could reduce the risk of preterm birth. This meta-analysis found six randomized controlled trials (RCTs) and 18 observational studies, and concluded that circulating maternal 25-OHD deficits may increase the risk of preterm birth, and vitamin D supplementation alone during pregnancy may reduce the risk of preterm birth (RR 0.57; 95% CI; 0.36-0.91), this also occuring in the spontaneous preterm birth subgroup (OR 1.45; 95% CI; 1.20-1.75)(18).
In one study, after supplementation of vitamin D in two cases of pregnancy, it was found that women with serum 25(OH)D of 40 ng/mL had a 59% lower risk of preterm delivery compared with women who had serum 25(OH)D levels of 20 ng/mL (p=0.02). In these clinical trials, the provision of vitamin D of 4000 IU/day was found to help safely reach a minimum level of 32 ng/mL at the beginning of the second trimester in various groups of pregnant women(24). Furthermore, it is known that in pregnant women, the conversion process of 25(OH)D to its active form, 1,25(OH)2D, takes place optimally at a vitamin D level of 40 ng/mL. The findings of this study support that the recommended vitamin D levels are 40-60 ng/ml to maintain the optimal health(19).
Another study found no significant correlation between preterm birth and vitamin D deficiency in cohort studies in single hospitals. Observations in a larger cohort indicate a minimal increase in risk between low vitamin D concentrations (20 ng/ml) and preterm birth. It is estimated that the differences in these findings relate to differences in the study population, so it is important to analyze the effects of race and geography on the results of the study(20).
The investigators concluded that the examination of maternal serum levels and maternal supplementation are a safe, cheap and affordable prevention tool, and can substantially reduce the occurrence of preterm labor and heavy burden associated with morbidity, mortality and economic costs that may result. They also underlined the importance of achieving the vitamin D levels recommended by IOM 2010, above 20 ng/ml, in order to prevent the preterm birth(9).
Conclusions
Thus, it’s obvious that vitamin D plays an important role in pregnancy. In normal pregnancy, vitamin D homeostasis is maintained using three mechanisms: increased calcitriol, increased maternal 25(OH)D availability for optimal maternal (OH)D status, and elevated maternal VDBP level(4,5).
Vitamin D is responsible for increasing the absorption of calcium, magnesium and phosphate in the intestine and has several other biological effects. VDR is present in almost all tissues and cells in the human body, and stimulates the production of cathelicidin macrophages which play a role in the immune system fight against infections. Cathelicidin is an antimicrobial peptide which is primarily stored in lysosomes of macrophages and PMNs. Cathelicidin was originally found in neutrophils, but can also be found in many other cells, including epithelial cells and macrophages after being activated by bacteria, viruses, fungi or hormones. The cathelicidin gene will be activated and will produce proteins (hCAP18/LL-37) to be used against the pathogen that has been ingested by phagosomes in macrophages(5).
The investigators concluded that the examination of maternal serum levels and maternal supplementation are a safe, cheap and affordable prevention tool, and can substantially reduce the occurrence of preterm labor and heavy burden associated with morbidity, mortality and economic costs that may result. They also stressed the importance of achieving the vitamin D levels recommended by IOM 2010, above 20 ng/ml, in order to prevent the preterm birth(9).
Acknowledgements
We would like to acknowledge E.D. Ginting for providing us full support for drafting this scientific review.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
2. Lockwood CJ. Testing for risk of preterm delivery. Clinics in Laboratory Medicine. 2003; 23(2):345-60.
3. Shin JS, Choi MY, Longtine MS, Nelson DM. Vitamin D effects on pregnancy and the placenta. Placenta. 2010; 31:1027-34.
4. Ross AC, Taylor CL, Yaktine AL, Valle HB (editors). Dietary Reference Intakes for Vitamin D and Calcium. Washington DC. National Academy Press. 2011.
5. Nair R, Maseeh A. Vitamin D: The “sunshine” vitamin. Journal of Pharmacology and Pharmacotherapeutics. 2012; 3(2):118.
6. Gombart AF. The vitamin D – antimicrobial peptide pathway and its role in protection against infection. Future Microbiol. 2009; 4:1151.
7. Karras SN, Wagner CL, Castracane VD. Understanding vitamin D metabolism in pregnancy: from physiology to pathophysiology and clinical outcomes. Metabolism. 2018; 86:112-23.
8. Liu N, Kaplan AT, Low J, Nguyen L, Liu GY, Equils O, et al. Vitamin D induces innate antibacterial responses in human trophoblasts via an intracrine pathway. Biol Reprod. 2009; 80(3):398-406.
9. McDonnell SL, Baggerly KA, Baggerly CA, Aliano JL, French CB, Baggerly LL, et al. Maternal 25(OH)D concentrations ≥40 ng/mL associated with 60% lower preterm birth risk among general obstetrical patients at an urban medical center. PlosOne. 2017; 12(7):e0180483.
10. Mostafa WZ, Hegazy RA. Vitamin D and the skin: focus on a complex relationship. A review. Journal of Advanced Research. 2015; 6(6):793–804.
11. Yeum KJ, Song BC, Joo NS. Impact of Geographic Location on Vitamin D Status and Bone Mineral Density. International Journal of Environmental Research and Public Health. 2016; 13(2):184.
12. Kennel KA, Drake MT, Hurley DL. Vitamin D Deficiency in Adults: When to Test and How to Treat. Mayo Clinic Proceedings. 2010; 85(8):752–58.
13. Singh J, Hariharan C, Bhaumik D. Role of vitamin D in reducing the risk of preterm labour. Int J Reprod Contracept Obstet Gynecol. 2015; 4(1):86-93.
14. Qin LL, Lu FG, Yang SH, Xu HL, Luo BA. Does Maternal Vitamin D Deficiency Increase the Risk of Preterm Birth? A Meta-Analysis of Observational Studies. Nutrients. 2016; 8(5):301.
15. Bodnar LM, Platt RW, Simhan HN. Early-Pregnancy Vitamin D Deficiency and Risk of Preterm Birth Subtypes. Obstetrics and Gynecology. 2015; 125(2):439–47.
16. Shibata M, Suzuki A, Sekiya T, Sekiguchi S, Asano S, Udagawa Y, Itoh M. High prevalence of hypovitaminosis D in pregnant Japanese women with threatened premature delivery. J Bone Miner Metab. 2011; 29(5):615-20.
17. Wagner C, Baggerly C, McDonnell S, Baggerly L, Hamilton S, Winkler J, Hollis B. Post-Hoc Comparison of Vitamin D Status at Three Time Points During Pregnancy Demonstrates Lower Risk of Preterm Birth with Higher Vitamin D Closer to Delivery. The Journal of Steroid Biochemistry and Molecular Biology. 2015; 148:256-60.
18. Zhou SS, Tao YH, Huang K, Zhu BB, Tao FB. Vitamin D and risk of preterm birth: Up to date meta-analysis of randomized controlled trials and observational studies. Journal of Obstetrics and Gynaecology Research. 2017; 43(2):247-56.
19. Hollis BW, Wagner CL. Vitamin D and pregnancy: Skeletal effects, nonskeletal effects, and birth outcomes. Calcif Tissue Int. 2013; 92:128–39.
20. Yang L, Pan S, Zhou Y, Wang X, Qin A, Huang Y, Sun S. The Correlation between Serum Vitamin D Deficiency and Preterm Birth. Med Sci Monit. 2016; 22:4401-05.
Articole din ediţiile anterioare
Screeningul ecografic în al treilea trimestru al sarcinii
Ultrasound screening for pregnancy abnormalities in the third trimester is a specialized investigation which should be considered a routine/standar...
Metforminul în managementul diabetului gestaţional
Diabetul gestaţional (DG) este o complicaţie comună a sarcinii, apărută în special în al doilea sau al treilea trimestru, cu o prevalenţă în contin...
Microangiopatii trombotice (PE/HELLP, PTT, aSHU). Diagnosticul diferenţial: date clinice şi de laborator
Cauzele microangiopatiei trombotice identificate în timpul sarcini sunt variate: specifice sarcinii şi nespecifice. Diferenţierea preeclampsiei de ...
Şocul anafilactic în sarcină: minireview
Şocul anafilactic este o reacţie severă, acută, generalizată, de hipersensibilitate, care apare rar în timpul sarcinii, dar care are efecte adverse...