Spontaneous heterotopic pregnancy with ampullar location of the ectopic pregnancy – case report and literature review
Sarcină heterotopică spontană cu localizare ampulară a sarcinii ectopice – prezentare de caz şi review al literaturii
Abstract
Heterotopic pregnancy (HP) is defined as the coexistence of an ectopic and an intrauterine pregnancy. It is a biovular twin pregnancy characterized by a difference in migration between the two embryos. Although the overall prevalence is increasing due to the wide use of techniques for ovulation induction and assisted reproduction techniques, spontaneous HP remains a very rare condition. In most spontaneous heterotopic pregnancies, the suspicion index is low, and the ectopic one is implanted in the ampullary segment of the tubes (80% of cases). We present herein a case with this rare condition: spontaneously conceived HP with an ampullar tube location of the ectopic pregnancy. We also reviewed the published literature, describing this specific variety of high-risk pregnancies, to raise the clinicians’ awareness. Most patients present with acute abdominal pain, and heterotopic pregnancy is diagnosed following the tubal rupture. The surgical management is usually required, even in yet uncomplicated HP. The preferred approach is minimally invasive surgery. In most cases, the goal of medical intervention is to remove the ectopic pregnancy and to ensure the uneventful evolution of the eutopic one. The unit’s facilities, the practitioner skills and the given case features are paramount. The case we describe is of a 32-year-old multigravida. She presented with acute, intense abdominal pain, in the context of secondary amenorrhea for seven weeks. The transvaginal ultrasound scan revealed a large amount of free fluid in the cul-de-sac, a live intrauterine pregnancy, and a left tubal ectopic live pregnancy. As in most spontaneous heterotopic pregnancies, our patient had no known risk factors for ectopic/heterotopic pregnancy. Emergency laparotomy and left salpingectomy were performed. Subsequently, the medical termination of the intrauterine pregnancy was performed at the couple’s request.Keywords
spontaneous heterotopic pregnancyultrasoundsalpingectomyabortionsurgeryRezumat
Sarcina heterotopică (SH) se defineşte ca fiind coexistenţa unei sarcini intrauterine şi a unei sarcini ectopice. Este o sarcină gemelară bizigotă, în care migrarea celor doi embrioni se produce diferit. Deşi prevalenţa SH este în creştere, prin utilizarea pe scară largă a inducţiei medicamentoase de ovulaţie şi a reproducerii umane asistate, sarcina heterotopică spontană a rămas foarte rar întâlnită. În majoritatea SH spontane, clinicienii suspectează greu diagnosticul, iar sarcina ectopică este tubară (implantată la nivelul ampulei în 80% din cazuri). Prezentăm un astfel de caz rar: sarcină heterotopică obţinută natural, cu localizarea ampulară a sarcinii ectopice. Am realizat o revizie a literaturii publicate în această varietate de sarcini cu risc înalt, cu intenţia de a spori atenţia medicilor asupra acestui diagnostic. Majoritatea pacientelor se prezintă cu dureri abdominale acute, iar diagnosticul este precizat după ruptura tubară. Tratamentul chirurgical este necesar în cea mai mare parte a cazurilor, chiar şi în sarcinile heterotopice necomplicate. Se preferă abordul minim invaziv. Scopul principal este de a îndepărta sarcina ectopică şi de a o proteja pe cea eutopică. Facilităţile unităţii respective, experienţa medicului şi caracteristicile cazului sunt foarte importante. Cazul întâlnit de noi este al unei paciente multipare în vârstă de 32 de ani. Pacienta prezenta dureri abdominale intense şi amenoree secundară (de şapte săptămâni). Examinarea ecografică transvaginală a relevat un volum mare de revărsat liber în fundul de sac Douglas, o sarcină intrauterină în evoluţie şi o sarcină ectopică tubară stângă în evoluţie. Ca în multe cazuri de sarcină heterotopică spontană, pacienta nu prezenta niciunul dintre factorii de risc cunoscuţi pentru sarcina ectopică/heterotopică. S-au practicat laparotomie de urgenţă şi salpingectomie stângă. Cuplul a solicitat şi întreruperea sarcinii intrauterine, care s-a practicat medicamentos.Cuvinte Cheie
sarcină heterotopică spontanăexaminare ecograficăsalpingectomieavortintervenţie chirurgicalăIntroduction
The coexistence of ectopic and eutopic pregnancy has different clinical forms, the ectopic pregnancy having various locations: tubal, interstitial, cervical, abdominal or ovarian. According to published literature, the most common ectopic implantation site is the Fallopian tube, in its ampullary segment.
The main risk factors for heterotopic pregnancy (HP) are the use of assisted reproduction techniques (ART), pelvic inflammatory disease, history of tubal surgery, intrauterine device implantation, and previous ectopic tubal pregnancy(1). However, spontaneous HP (SHP) often occurs in the absence of any known predisposing risk factors. SHP is a rare clinical condition, having a historically reported incidence of 0.003% in all pregnancies(2).
The symptoms of heterotopic pregnancy are nonspecific: abdominal pain, vaginal bleeding and/or amenorrhea. The diagnosis usually requires transvaginal ultrasound (TVUS). The use of serum levels dynamic of the b subunit of human chorionic gonadotropin (b-HCG) is hampered by the secretion of the simultaneous intrauterine pregnancy (IUP)(3).
In most cases, clinicians and emergency department doctors include in the differential diagnosis, after confirming the IUP: ovarian/adnexal torsion, appendicitis, urinary tract infections and/or spontaneous incomplete or missed abortion, gestational trophoblastic disease/ choriocarcinoma. In the absence of straightforward ultrasound (US) images, the diagnosis of the simultaneous ectopic pregnancy (EP) is intraoperative in most cases. The transvaginal ultrasound scan is paramount in clarifying the positive diagnosis.
The therapeutic approach is impressively standardized in fact, as we will show below. In most cases, it consists in the removing of the extrauterine pregnancy and trying to preserve the IUP. Laparoscopic removal is considered the most appropriate approach, having fewer postoperative complications. In cases presenting with hemorrhagic shock, emergency laparotomy may be required as a lifesaving intervention. Direct injection of potassium chloride and methotrexate (by transvaginal or transabdominal approach) is historically mentioned in previous publications. Systemic MTX cannot be used in patients who opt to continue the IUP.
Case description
A healthy 32-year-old multigravida (gravida 11, term 3, preterm 0, abortion 8, living 3), with no medical history, presented to our obstetrics and gynecology emergency room with severe low abdominal pain and seven weeks of amenorrhea. She was Caucasian, she had many on-request surgical terminations of pregnancy, never had an intrauterine device inserted, had no pelvic inflammatory disease episodes, no history of previous abdominal surgery, and she never smoked. The patient denied any kind of drug administration.
On examination, the patient was vitally stable, with a blood pressure reading of 100/65 mmHg, a heart rate of 118 beats per minute, and a normal temperature. Laboratory testing at admission showed a serum hemoglobin concentration of 8.5 g/dL, biochemical tests with normal results, and an elevated serum b-HCG (5853 mIU/mL).
The TVUS revealed a live intrauterine pregnancy, with an embryo measuring 19.4 mm (corresponding to 8 weeks and 3 days) and a left tubal ectopic pregnancy with a live embryo measuring 17.2 mm (corresponding to 8 weeks and 1 day) – Figure 1.
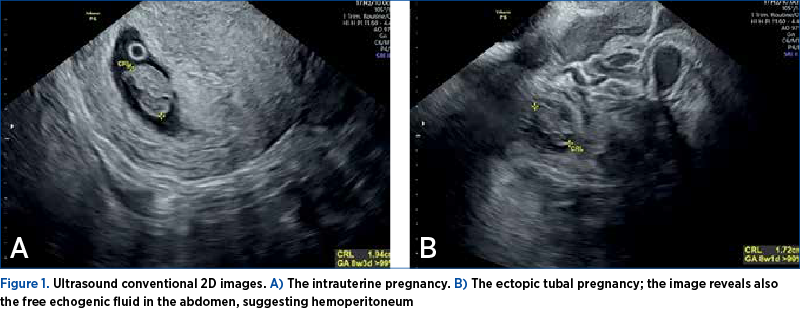
A single typical gestational corpus luteum (located in the left ovary) and an image consistent with a functional hemorrhagic cyst (approximately 4 cm diameter, in the right ovary) were seen. Also, TVUS revealed a large amount of free fluid in the cul-de-sac, anteriorly to the uterus, and in the Morrison’s space. The patient had complete family planning at the presentation, and the twin SHP was unplanned and unsupported. After counseling, the couple agreed to an emergency laparotomy and the removal of the ectopic tubal pregnancy. They also required the intraoperative ligation of the remaining tube and the termination of the IUP.
We managed this case during the global health crisis generated by COVID-19. Due to technical limitations in the context of the rapid development of signs of hypovolemic shock, an emergency abdominal salpingectomy was performed. Roughly 1500 ml of free blood was present in the abdomen at the opening. During surgery, the right ovarian cyst described by the ultrasound exam was removed. Electric ablation of the corpus luteum was performed also (Figure 2).
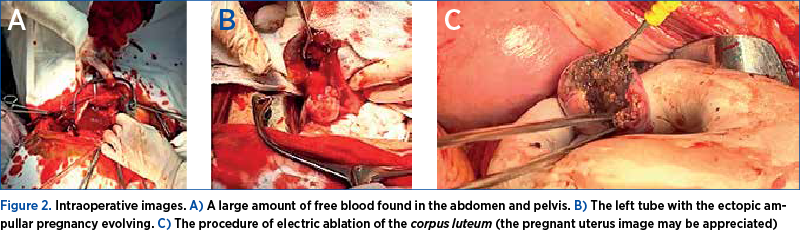
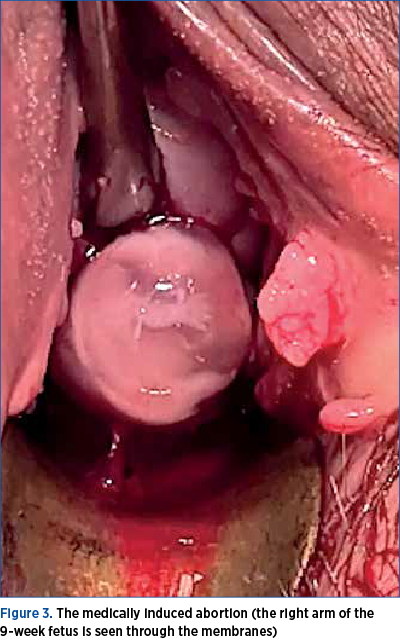
Postoperatively, the hemoglobin level dropped to 7.02 g/dL. The patient had an uneventful postoperative evolution after two blood unit transfusions. A combined treatment (mifepristone 200 mg and misoprostol – 4 x 0.2 mg) was administered on the second day, to terminate the IUP. Two days later, the medically induced termination of the IUP occurred (Figure 3).
The histopathological exam confirmed the diagnosis of ectopic pregnancy in the specimen removed – left tube.
Literature review
We searched on The National Center for Biotechnology Information – the international database PubMed Central, restricting our selection to available full-text publications, and English or French language only manuscripts. The search engine was limited to the words “spontaneous heterotopic pregnancy” [All Fields]. Two authors (M.D. and A.F.C.S.) individually screened the abstracts and manuscripts resulted, for relevance and completeness.
We found 124 eligible manuscripts. We subsequently decided to limit our search to the last seven years, considering the huge development of technology in the medical ultrasound, the wider availability of machines equipped with transvaginal probes (especially in emergency units), and the ever-increased awareness of the medical staff. We ended up with 96 manuscripts. The authors scrutinized each publication and omitted the ones describing other varieties of SHP apart from the ones located on the ampullar region of the tubes (e.g., scar, abdominal, ovarian, interstitial etc.). They excluded one publication describing six cases of spontaneously conceived heterotopic triplets(4) (all six cases being reported before 2015). The authors excluded also a large case series reporting on the risk of miscarriage following surgical treatment of heterotopic extrauterine pregnancies(5). Although seven SHPs were included in this retrospective report carried out in three London early pregnancy units (EPUs) and covering 20 years(5), critical important data considered in our literature review were missing, due to the completely different target of the study.
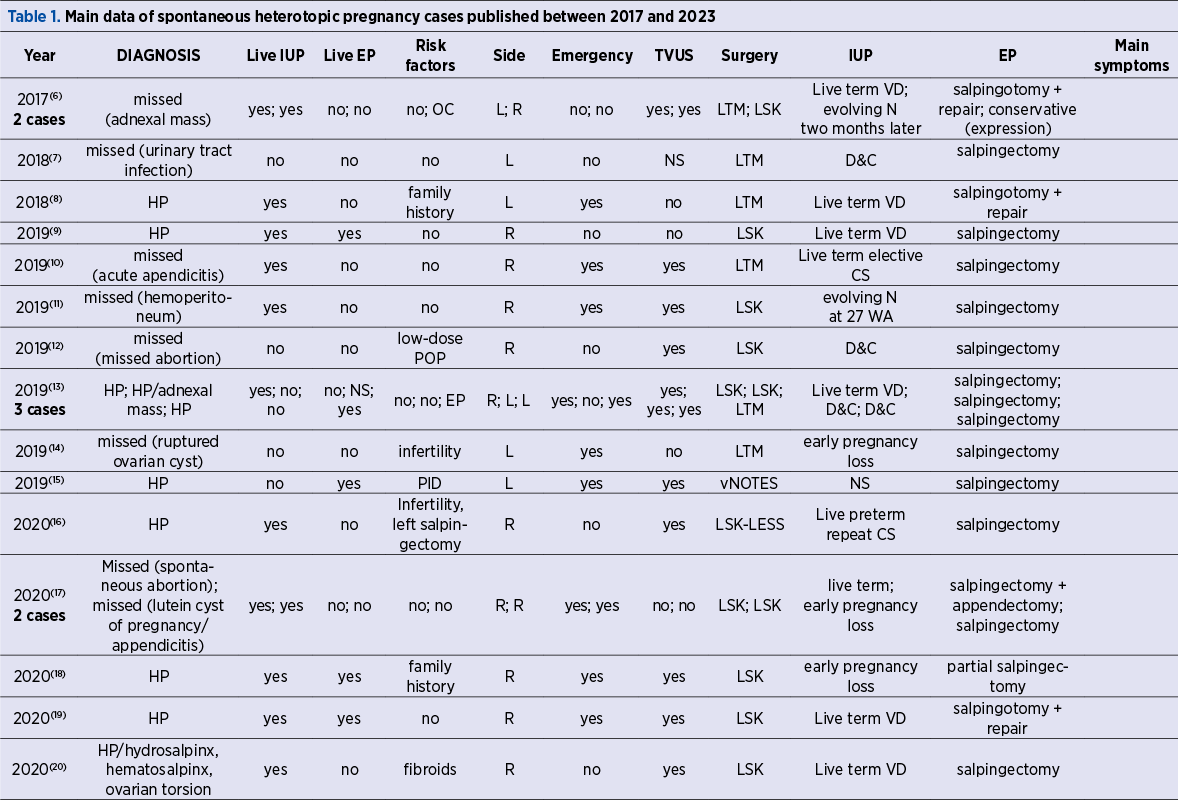
The final review included 36 records, including our case, describing a total of 41 cases.
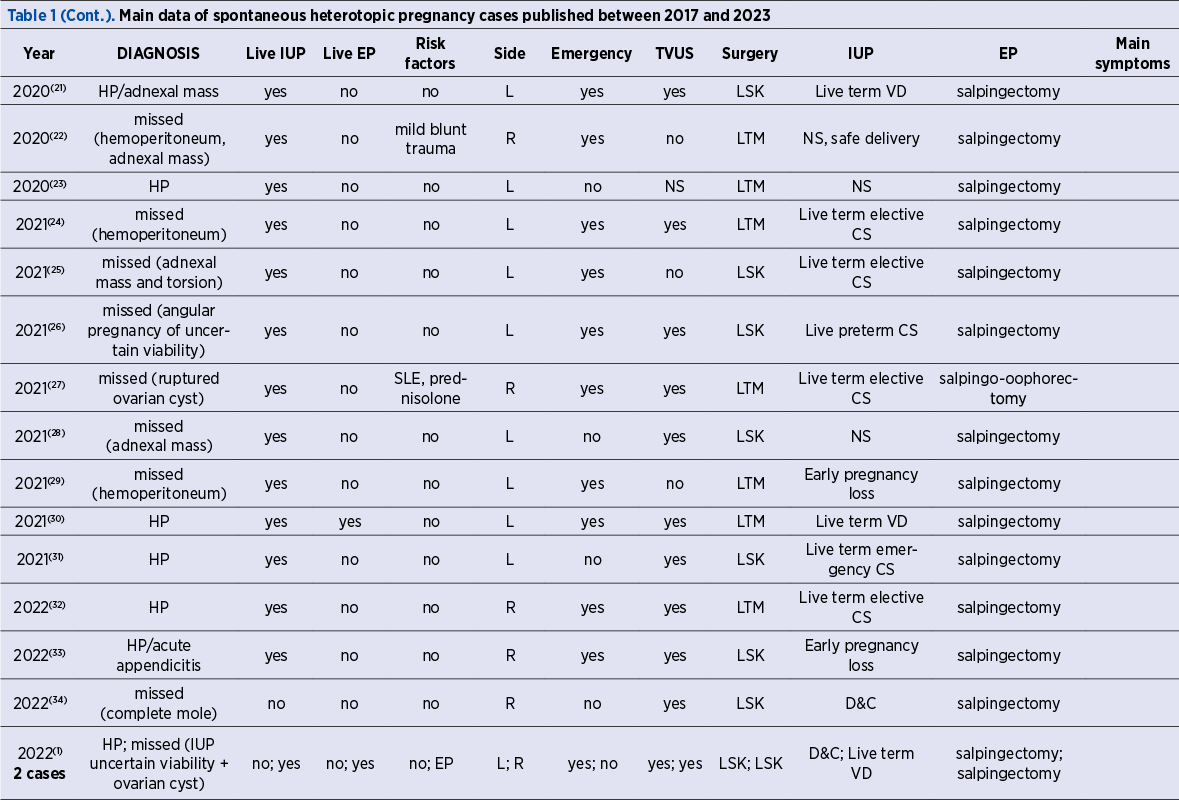
Data from the articles selected for inclusion in this narrative review were extracted independently and then homogenized by the two authors. The data are summarized in Table 1 (also presented completely in the additional material). The table contains the following features for interpretation: author, date of publication, number of cases reported, mother’s demographics (age, gestation and parity range, risk factors), the main symptom at presentation, the main suspected diagnosis at presentation, the gestational age at the diagnosis, the side (right or left) of the affected tube, the type of the ultrasound scan used, the surgical approach, and the outcome of each of the two pregnancies.

A live pregnancy was defined by the presence of an embryo/fetus with visible cardiac activity on US scan. The normally sited IUP (the eutopic pregnancy) and the ectopic ampullar pregnancy were defined using the ESHRE terminology and classification(40).
Pregnancies that were less than 6 weeks of gestation were considered potentially live if the morphological appearances on US scan was as expected for the gestational age. The term “miscarriage” included the early embryonic demise (intact gestational sac of at least 25 mm in size without an embryo or with an embryo measuring at least 7 mm, with no evidence of cardiac activity)(40), pregnancies with an abnormal course at follow-up, and complete/incomplete miscarriages as reported by the authors.
Since 2019, a rather steady number of cases (between five and nine) were reported yearly. The total number of SHP cases published in the last seven years (40) is relatively small, which reflects the rarity of this condition. The vast majority were case reports or very small case series (two manuscripts described two cases, and one – a case series of three).
The maternal demographic characteristics (patients in selected records) are shown in Table 2.
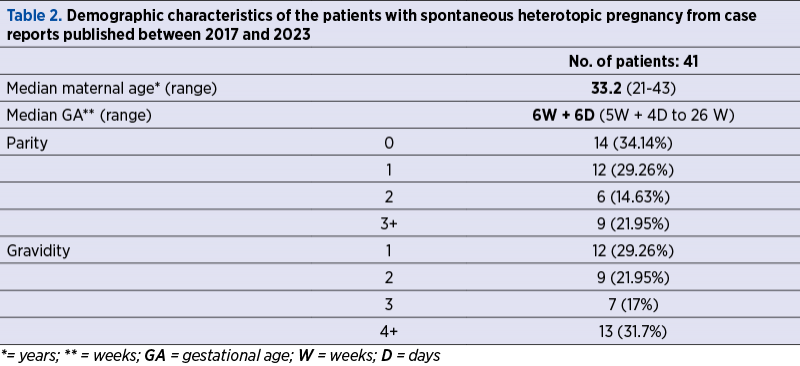
The median maternal age was 33.2 years old (the extreme ages being 21 and 43 years old). The median gestational age at diagnosis was low – 6 weeks and 6 days (the extreme gestational ages being 5 weeks and 26, respectively). At the diagnosis, the IUP was live in most cases (35/41 – 85.36%). On the contrary, a live embryo/fetus in the EP was not confirmed in 32 of the 41 cases (78%), and not specified in one manuscript.
The diagnosis was missed and/or delayed in 26 of 41 cases (63.41%). The traditional risk factors – history of EP, fibroids, infertility, previous IVF (in vitro fertilization) procedures, documented pelvic inflammatory disease – were present in seven cases only (17%), while completely absent in most cases (28/41 – 68.29%). Of note, some of the cases had less recognized associations: family history of multiple gestations, corticoid therapy for lupus erythematosus systemic, hormonal therapy (oral contraceptives, progestin-only pills), and mild blunt abdominal trauma.
Ten patients (24.4%) had completely misleading symptoms, either suggesting a complicated IUP, or suggesting other systems involvement (digestive, respiratory, and cardiovascular symptoms), highlighting the complexity of the diagnosis in selected cases.
The medical/expectant approach was absent in the reviewed literature, although in a recent retrospective report three tubal ectopic pregnancies were managed expectantly(5). In the recent literature, a conservative approach was possible in one case only(6). In the majority of cases, a unilateral total salpingectomy was performed (34/41 – 82.92%). In two cases, the operators performed salpingo-oophorectomy(27,36), and four cases allowed salpingotomy and repair(6,8,19) or partial salpingectomy(18).
The percentage of severe clinical presentation, managed under pressure, as vital surgical emergencies, was rather high (27/41 – 65.85%), much higher than the IVF-resulted HP group(41). In this subgroup of SHP, the diagnosis was based on the presence of acute abdominal symptoms, confirming the data reported previously(24). In the case series analyzed, the pain was a mainstay, being present in the vast majority of cases (38/41 – 92.68%).
According to the current trend toward minimally invasive surgery, most of the spontaneous heterotopic pregnancies reported were managed by laparoscopy (26/41 – 63.41%). Yet, in 15 cases (36.58%), laparotomy was performed, as in previous reports(25,37,43). In one case, vaginal natural orifice transluminal endoscopic surgery (vNOTES) was performed(15), and in another one, the LESS (laparoendoscopic single site surgery) technique was used(16).
Almost all reported cases had pathological confirmation.
Contrary to some previously reported results(39), we found that the left location was almost equally represented (21/41 – 51.21%) as the right side (20/41 – 48.78%).
Live term babies resulting from the post-surgery evolving IUPs had a significant rate – 24/41 (58.53%). In the described group, there were only five cases of early pregnancy loss following the surgical procedure. In three cases, the outcome of the IUP was not specified, and there were some on-request terminations of pregnancy also.
Discussion
Heterotopic pregnancy obtained spontaneously is exceptionally rare. Although at times (especially in complicated and higher gestational cases) HP is an easy and straightforward diagnosis, our literature research revealed that it remains a diagnostic challenge in many cases. As expected, in women without any risk factors, a delay in diagnosis and treatment was present. Maintaining a low threshold for the diagnosis of HP is the mainstay for clinicians, especially those working in emergency and trauma departments(1,36).
The symptoms are nonspecific. Heterotopic pregnancy is asymptomatic in 17.5%(44) to 32%(42) of cases following in vitro fertilization. In the SHP case series, this percentage was much lower (7.3%). The patient’s complaints – as the intense pain in the context of a live IUP – may guide the clinician toward the ectopic pregnancy diagnosis. Abdominal pain was the most common symptom in the case series we reviewed, being present in most of them (over 92% cases). Yet, in real life, this symptom may be attributed to a pathologic intrauterine pregnancy, not to complications of ectopic pregnancy. In our case, due to a conclusive ultrasound in the presence of a late-discovered pregnancy, the diagnosis was easily reached.
Contrary to what we expected in the era of high-resolution US imaging and Doppler techniques, the diagnosis was missed and/or delayed in an impressive number of cases (over 63%). Most probably, visualizing using ultrasound the (normal or abnormal) IUP may be a reason for false reassurance. Moreover, the presence of adnexal cystic masses, complicating many intrauterine pregnancies and heterotopic pregnancies, may obscure the diagnosis and confuse further practitioners(36,38).
No risk factors were present in our case, strengthening the assumption that there could be other mechanisms and pathways (other than tubal pathology) that may play a role in the extrauterine pregnancy implantation(20).
Approximately 70% of heterotopic pregnancies resulting after IVF are diagnosed early, between 6 and 8 gestational weeks. In our case series also, 65.85% of cases (27/41) were diagnosed before 9 weeks. In the case we described, the diagnosis was delayed until the tubal rupture, the patient having no booking in her current pregnancy and no previous presentation in the gynecology department since her last TOP. Also, in our case, the diagnosis was easy due to the presence of heart activity in both intrauterine and ectopic embryos. This is an important clue, rarely seen in practice. In our case, the location of the ectopic pregnancy was in the ampullary segment, the most frequent location(10,41).
Scanning in early pregnancy should include the identification and the ultrasound assessment of the adnexa. According to ISUOG Practice Guidelines(45), the ultrasound scan in early pregnancy should provide information not only regarding the viability of the pregnancy, the gestational age, the number of embryos/fetuses, chorionicity in multiple pregnancy, but it should include the assessment of the adnexa for abnormalities and masses also(45).
According to our literature review results, whether the IUP embryo survives or not, the diagnosis of heterotopic pregnancy might be missed (more than half cases in our SHP case series). If the diagnosis is missed or delayed, these conditions can become life-threatening(46). Prompt gynecologic surgery may be required (almost 66% of the reviewed cases).
In the subgroup of women with ampullar SHP we described, the eutopic pregnancy was described as “live” on the initial scan in 35/41 cases (85.36%). On the contrary, a live ectopic pregnancy was confirmed in eight cases only (19.51%).
In the 41 cases reviewed, only five suffered an early pregnancy loss (12.19%). In six cases, dilation and curettage were performed, and in three cases the couple requested the termination of the intrauterine pregnancy. In 24 cases (58.53%), the intrauterine pregnancy had a normal, uneventful course, resulting in live and well neonates (of which only two being preterm).
If the intrauterine pregnancy is not desired, the treatment applied aims to remove both pregnancies safely and effectively. In our case, the electric ablation of the luteal body was intended to suppress the progesterone secretion, which is critical for the IUP early evolution. Subsequently, the medical termination of pregnancy was performed.
As in other reported cases, low compliance to prenatal care and/or a late booking may lead to a higher risk for surgical emergencies and to a poorer maternal and IUP outcome.
An especially high-risk situation is when the couple requires medical or surgical termination of the known intrauterine pregnancy. In the absence of a complete diagnosis, the procedure leads to potentially fatal complications (rupture of the EP) and massive intraabdominal hemorrhage(5,37).
Conclusions
Spontaneous heterotopic pregnancy (SHP) remains an exceptionally rare occurrence. The presence of a normal IUP is often perceived as a reassuring sign by clinicians when assessing women presenting with clinical signs suspicious of ectopic pregnancy. This can lead to a delay in diagnosing the concomitant ectopic pregnancy with an increased risk of adverse maternal outcome.
Once the diagnosis is suspected or reached, the management of SHP with an ampullar location is rather standard. Although there are no formal standard protocols for the treatment, in real life the options are limited to unilateral total salpingectomy.
Our SHP case and the literature review results highlight the need for systematic ultrasound assessment of the pelvis during the first trimester of pregnancy, even though the intrauterine pregnancy is confirmed and looks as expected. The diagnosis can be delayed in the absence of an examination of both adnexa. The diagnosis of ectopic pregnancy remains challenging at times, and the SHP diagnosis is even more so.
In the absence of common risk factors (like ART), the diagnosis is often missed. In this matter, we do agree with the simple dictum “think ectopic”, as previously stated(43), in all cases presenting with intense pelvic pain and pregnancy and/or hemoperitoneum and pregnancy.
Even more so, patients having abdominal pain and/or vaginal bleeding in early pregnancy should be scrutinized for heterotopic pregnancy. This involves a careful assessment of both adnexa, even in naturally conceived pregnancies.
Heterotopic pregnancy can become a life-threatening condition. The case presented (a late diagnosed one) and the literature review results highlight the easiness of reaching the point of hemodynamic imbalance. The early diagnosis prevents complications such as rupture of the ectopic pregnancy, hemoperitoneum, and hemorrhagic shock.
In the SHP subgroup, if diagnosed and treated timely, heterotopic pregnancy has a favorable maternal and IUP outcome.
Our manuscript is intended as a reminder that exceptionally rare and life-threatening situations may occur in the absence of known risk factors. In cases with less clear ultrasound images, in the absence of straightforward interpretable images (such as in our reported case, characterized by a live embryo in the ectopic pregnancy), the medical staff may easily miss the real diagnosis. Delays in the surgical intervention may endanger both the well-being of the mother and the normal course of a desired intrauterine pregnancy.
The surgical intervention during pregnancy (either laparoscopy or laparotomy) does not seem to raise the prevalence of spontaneous miscarriages and preterm labor.
Acknowledgement. This work did not receive any funding. None of the authors has any conflict of interests to declare.
Corresponding author: Ştefania Tudorache, e-mail: stefania.tudorache@gmail.com
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.
Bibliografie
-
Elsayed S, Farah N, Anglim M. Heterotopic Pregnancy: Case Series and Review of Diagnosis and Management. Case Rep Obstet Gynecol. 2023;2023:2124191.
-
DeVoe RW, Pratt JH. Simultaneous intrauterine and extrauterine pregnancy. Am J Obstet Gynecol. 1948;56(6):1119-26.
-
Oancea M, Ciortea R, Diculescu D, Poienar AA, Grigore M, Lupean RA, Nicula R, Chira D, Strilciuc S, Mihu D. Spontaneous Heterotopic Pregnancy with Unaffected Intrauterine Pregnancy: Systematic Review of Clinical Outcomes. Medicina (Kaunas). 2020;56(12):665.
-
Bataille P, Reynard A, Ducarme G. Spontaneous heterotopic triplets - A review of literature. J Gynecol Obstet Hum Reprod. 2017;46(8):657-659.
-
Solangon SA, Otify M, Gaughran J, Holland T, Ross J, Jurkovic D. The risk of miscarriage following surgical treatment of heterotopic extrauterine pregnancies. Hum Reprod Open. 2022;2022(1):hoab046.
-
Guennoun A, Mamouni N, Errarhay S, Bouchikhi C, Banani A. La grossesse hétérotopique spontanée: à propos de deux cas: Spontaneous heterotopic pregnancy: about 2 cases. Pan Afr Med J. 2017;28:306 [French].
-
Aroke D, Ngek LT, Tindong M, Fomanka E, Achu C, Tanah AA, Kadia BM. Blighted ovum and tubal pregnancy: a rare form of heterotopic pregnancy: case report. BMC Res Notes. 2018;11(1):242.
-
Onoh RC, Ejikeme BN, Onwe AB, Asiegbu OU. Ruptured ectopic in heterotopic pregnancy: Management and spontaneous vertex delivery of a live baby at term. Niger J Clin Pract. 2018;21(5):672-677.
-
Nazlı Yenigul N, Asicioglu O, Ayhan I. Successful laparoscopic treatment of asymptomatic heterotopic pregnancy after spontaneous conception. J Obstet Gynaecol. 2019;39(4):571-572.
-
Guimarães AC, Reis LDO, Leite FC, Reis CFDD, Costa AP, Araujo WJB. Spontaneous Heterotopic Triplet Pregnancy with a Two Viable Intrauterine Embryos and an Ectopic One with Right Tubal Rupture. Rev Bras Ginecol Obstet. 2019;41(4):268-272.
-
Gallaher C, Tahmasebi F, Sayasneh A, Mehra G. Spontaneous Heterotopic Pregnancy Associated with Massive Intraperitoneal Haemorrhage and a Normal Heart Rate, Illustrating the Concept of Relative Bradycardia. Case Rep Obstet Gynecol. 2019;2019:2893149.
-
Thakur U, Atmuri K, Borozdina A. Acute pelvic pain following miscarriage heterotopic pregnancy must be excluded: case report. BMC Emerg Med. 2019;19(1):59.
-
Nabi U, Yousaf A, Ghaffar F, Sajid S, Ahmed MMH. Heterotopic Pregnancy - A Diagnostic Challenge. Six Case Reports and Literature Review. Cureus. 2019;11(11):e6080.
-
Fomukong NH, Ngouagna E, Edgar MML, Nkfusai CN, Bede F, Wirsiy FS, Cumber SN. A case report of ruptured ectopic pregnancy plus massive hemoperitoneum on a heterotrophic pregnancy in a resource-poor setting, Mbengwi, Cameroon. Pan Afr Med J. 2021;39:52.
-
Doğan K, Kaya C, Ilıman DE, Karaca İ, Cengiz H. A spontaneous heterotopic pregnancy presenting with acute abdomen treated with natural orifice transluminal endoscopic surgery procedure: Case report. Turk J Obstet Gynecol. 2019;16(4):271-273.
-
Xiao J, Fu K, Duan K, Wang J, Sunkara S, Guan X. Pregnancy-preserving Laparoendoscopic Single-site Surgery for Gynecologic Disease: A Case Series.
-
J Minim Invasive Gynecol. 2020;27(7):1588-1597.
-
Stanic Z, Roje D, Matić D, Persec Z, Dapic K, Vidaković MR, Fureš R, Hrgovic Z, Fureš D. Spontaneous Heterotopic Pregnancy as an Uncommon Clinical Problem. Z Geburtshilfe Neonatol. 2020;224(4):223-226.
-
Aziz M, Arronte J. A case of spontaneous heterotopic pregnancy in natural conception complicated with hemoperitoneum. Heliyon. 2020;6(2):e03373.
-
Černiauskaitė M, Vaigauskaitė B, Ramašauskaitė D, Šilkūnas M. Spontaneous Heterotopic Pregnancy: Case Report and Literature Review. Medicina (Kaunas). 2020;56(8):365.
-
Diakosavvas M, Blontzos N, Daskalakis G, Protopapas A, Kathopoulis N, Antsaklis P, Derdelis G, Angelou K, Fasoulakis Z, Loutradis D, Theodora M. Vaginal Delivery at Term in a Woman with a Spontaneous Heterotopic Pregnancy Treated with Laparoscopic Salpingectomy. Case Rep Obstet Gynecol. 2020;2020:8892273.
-
Soares C, Maçães A, Novais Veiga M, Osório M. Early diagnosis of spontaneous heterotopic pregnancy successfully treated with laparoscopic surgery. BMJ Case Rep. 2020;13(11):e239423.
-
Elhadidi A, Alhariri A, Hosny Garib M, Mansour A, Almutiri B. Ruptured Heterotopic Pregnancy: A Rare Encounter in Acute Surgical Care Settings. Cureus. 2020;12(11):e11782.
-
Murewanhema G, Madombi S, Hlathswayo L, Simango N. Concurrent ruptured spontaneous heterotopic pregnancy and ruptured appendix with delayed presentation in the first trimester: a case report. Pan Afr Med J. 2020;37:222.
-
Kajdy A, Muzyka-Placzyńska K, Filipecka-Tyczka D, Modzelewski J, Stańczyk M, Rabijewski M. A unique case of diagnosis of a heterotopic pregnancy at 26 weeks - case report and literature review. BMC Pregnancy Childbirth. 2021;21(1):61.
-
de Oliveira S, Yaron M, Dällenbach P. Spontaneously conceived 17-week heterotopic pregnancy: a challenging and unusual diagnosis. BMJ Case Rep. 2021;14(3):e215489.
-
Kluckman ML, Schwope RB, Provagna AJ, Yauger BJ, Ramirez CI. The double corpus luteum: A novel sonographic sign of heterotopic pregnancy. J Clin Ultrasound. 2021;49(6):617-621.
-
Ntounis T, Fasoulakis Z, Koutras A, Diakosavvas M, Bourazan A, Pagkalos A, Samara AA, Kontomanolis EN. Heterotopic tubal pregnancy with a naturally conceived live twin intrauterine pregnancy in a patient with systemic lupus erythematosus: A case report. Case Rep Womens Health. 2021;32:e00348.
-
Abdelmonem AH, Sayed G, Abugazia AE, Kohla S, Youssef R. Heterotopic pregnancy after a spontaneous conception a case report with a review of clinical, laboratory and imaging findings. Clin Case Rep. 2021;9(8):e04649.
-
Dipanda AN, Fouogue JT, Mve VK, Kenfack B, Kemfang JDN. Pitfalls in Diagnosing Heterotopic Pregnancy in Sub-Saharan Africa: A Case Report at the Yaounde University Teaching Hospital (Cameroon). Case Rep Obstet Gynecol. 2021;2021:7970646.
-
Ouafidi B, Kiram H, Benaguida H, Lamrissi A, Fichtali K, Bouhya S. Diagnosis and management of a spontaneous heterotopic pregnancy: Rare case report. Int J Surg Case Rep. 2021;84:106184.
-
Cucinella G, Gullo G, Etrusco A, Dolce E, Culmone S, Buzzaccarini G. Early diagnosis and surgical management of heterotopic pregnancy allows us to save the intrauterine pregnancy. Prz Menopauzalny. 2021;20(4):222-225.
-
Maduako KT, Onoh V. Term delivery of a heterotopic pregnancy coexisting with ruptured tubal ectopic pregnancy: A case report. Afr J Reprod Health. 2022;26(4):110-113.
-
Nguyen KP, Hudspeth M, Milestone H. Spontaneous Heterotopic Pregnancy: Diagnosis and Management. Case Rep Obstet Gynecol. 2022;2022:2994808.
-
Dubbewar A, Srivastava A, Hiremath RN, Ghodke S, Chourey N, Sreenivas A. A rare case of spontaneous heterotopic pregnancy with intrauterine gestational trophoblastic neoplasia and tubal ectopic pregnancy at a remote secondary care hospital. J Family Med Prim Care. 2022;11(7):3996-3998.
-
McKeown C, Kalu C, DeTavernier MC. Heterotopic pregnancy following spontaneous conception. Ir Med J. 2023;116(9):863.
-
Teka H, Yemane A, Gebremeskel M, Kinfe BA, Kiros S, Kidanu M. Heterotopic Pregnancy with Ipsilateral Adnexal Cyst Causing a Diagnostic Dilemma: A Case Report. Int Med Case Rep J. 2023;16:27-34.
-
Yu S, Lv W, Li W. Missed Spontaneous Heterotopic Pregnancy: A Case Report of a Ruptured Tubal Pregnancy after Induced Abortion. J Coll Physicians Surg Pak. 2023;33(7):829-830.
-
Kathopoulis N, Diakosavvas M, Kypriotis K, Chatzipapas I, Domali E, Protopapas A. Laparoscopic management of a second trimester ruptured spontaneous heterotopic tubal pregnancy mimicking ovarian tumour, a case report. Facts Views Vis Obgyn. 2023;15(2):157-160.
-
Dao D, Abdel-Raheem M, Lazim TR. A Spontaneous Heterotopic Pregnancy Presenting as Acute Appendicitis. Cureus. 2023;15(8):e42803.
-
ESHRE Working Group on Ectopic Pregnancy; Kirk E, Ankum P, Jakab A, Le Clef N, Ludwin A, Small R, Tellum T, Töyli M, Van den Bosch T, Jurkovic D. Terminology for describing normally sited and ectopic pregnancies on ultrasound: ESHRE recommendations for good practice. Hum Reprod Open. 2020;2020(4):hoaa055. Barrenetxea G, Barinaga-Rementeria L, Lopez de Larruzea A, Agirregoikoa JA, Mandiola M, Carbonero K. Heterotopic pregnancy: two cases and a comparative review. Fertil Steril. 2007;87(2):417.e9-15.
-
Yu Y, Xu W, Xie Z, Huang Q, Li S. Management and outcome of 25 heterotopic pregnancies in Zhejiang, China. Eur J Obstet Gynecol Reprod Biol. 2014;180:157-61.
-
Talbot K, Simpson R, Price N, et al. Heterotopic pregnancy. J Obstet Gynaecol. 2011;31:7–12.
-
Zhang Y, Chen X, Lin Y, Lian C, Xiong X. Study on diagnosis and management strategies on heterotopic pregnancy: a retrospective study. J Obstet Gynaecol. 2023;43(1):2152660.
-
Salomon LJ, Alfirevic Z, Bilardo CM, et al. ISUOG practice guidelines: performance of first-trimester fetal ultrasound scan [published correction appears in Ultrasound Obstet Gynecol. 2013 Feb;41(2):240]. Ultrasound Obstet Gynecol. 2013;41(1):102-113.
-
Zhu S, Fan Y, Lan L, Deng T, Zhang Q. Heterotopic Pregnancy Secondary to in vitro Fertilization-Embryo Transfer: Risk Factors and Pregnancy Outcomes. Front Med (Lausanne). 2022;9:864560.



