Tipuri actuale de naştere şi impactul lor asupra mamei şi fătului
Types of childbirth nowadays and their impact on both mother and newborn
Abstract
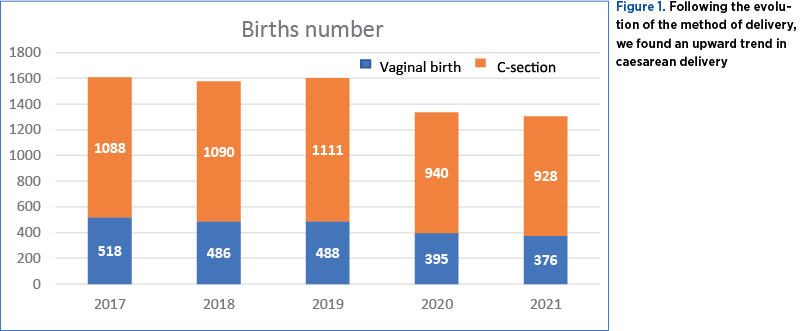
Following the evolution of the method of delivery, we found, according to an observational study carried out in our clinic between 2017 and 2021, an upward trend of caesarean deliveries. As a result, in 2021, the number of caesarean surgeries was three times higher compared to the number of vaginal births. This upward trend is particularly observed among developing countries, where the percentage of caesarean deliveries tends to exceed 50-60% of all births. Even in countries with a well-established health system, such as those from North America, North-West Europe, Australia and North Asia, where although vaginal birth remains the first option in terms of the method of birth, the trend also tends to be upward for birth by caesarean section, but the difference is a much smaller percentage, of approximately 30% of the total number of births. The increase in the number of caesarean sections has led, in recent years, to the implementation of antenatal corticoprophylaxis at gestational ages close to term, over 37 weeks, to improve neonatal adaptation and implicitly reduce costs related to newborn care. In this article, we present the statistical data obtained over five years regarding the mode of delivery in the clinic of the “Elias” University Emergency Hospital, Bucharest, and we discuss the risks involved, the utility of corticoprophylaxis, and the impact of caesarean section on the newborn.Keywords
caesarean sectioncorticoprophylaxispregnancyvaginal birthnewbornRezumat
În urma evoluţiei modalităţii de naştere, am constatat, potrivit unui studiu observaţional efectuat în clinica noastră în perioada 2017-2021, o tendinţă ascendentă a naşterii prin cezariană. Ca urmare, în anul 2021 numărul operaţiilor cezariane a fost de trei ori mai mare faţă de numărul de naşteri vaginale. Această tendinţă ascendentă se observă în special în ţările în curs de dezvoltare, unde procentajul naşterilor prin operaţie cezariană tinde să depăşească 50-60% din totalul naşterilor. Chiar şi în ţările cu un sistem de sănătate bine implementat, cum ar fi cele din America de Nord, Europa de Nord-Vest, Australia şi Asia de Nord, unde, deşi naşterea vaginală rămâne prima opţiune în ceea ce priveşte modalitatea de naştere, tendinţa tinde să fie, de asemenea, ascendentă pentru naşterea prin cezariană, însă diferenţa constă într-un procentaj mult mai mic, de aproximativ 30% din numărul total al naşterilor. Creşterea numărului de operaţii cezariane a determinat în ultimii ani apariţia conceptului de corticoprofilaxie prenatală, administrată la vârste gestaţionale apropiate de termen, peste 37 de săptămâni, pentru a îmbunătăţi adaptarea neonatală şi, implicit, pentru a reduce costurile de îngrijire a nou-născutului în unităţile de terapie intensivă neonatală. În acest articol, prezentăm datele statistice obţinute în clinica Spitalului Universitar de Urgenţă „Elias”, Bucureşti, pe parcursul a cinci ani, cu privire la modalitatea de naştere şi discutăm despre riscurile pe care acestea le implică, despre utilitatea corticoprofilaxiei şi despre impactul operaţiei cezariane asupra nou-născutului.Cuvinte Cheie
operaţie cezarianăcorticoprofilaxiesarcinănaştere vaginalănou-născutIntroduction
Delivery through caesarean section represents the surgical intervention performed to extract the fetus, when natural birth cannot take place, the indications being most often represented by labor dystocia, signs of fetal distress, abnormal fetal presentations, multiple pregnancies, or when the pregnant woman associates a pathology that contraindicates natural birth. Caesarean section is performed by making a surgical incision at the level of the suprapubic abdominal wall (laparotomy) and the uterine wall (hysterotomy), and involves risks, both for the pregnant woman and for the fetus, so we should take into consideration the way this intervention will impact on the long-term the evolution of both the mother and the newborn. It is recommended to take into account the emotional aspects involving the lack of immediate contact of the newborn with the mother, the difficulty or the impossibility of performing the “skin to skin” technique, the late initiation of breastfeeding, and the immediate postnatal adaptation of the newborn. The lack of passage through the vagina does not allow the colonization of the neonatal intestinal microbiome with microorganisms from the local microbiota, subsequently predisposing these newborns to respiratory, skin and digestive allergies. It is also relevant to take into consideration the immediate and long-term complications for the woman through the much higher risk of infections, hemorrhages, anesthesia complications, limiting the number of future pregnancies and, implicitly, the birth rate and, last but not least, through the increased hospitalization costs, which often involve both the woman and the newborn(1).
From a historical point of view, the procedure of caesarean delivery changed both in the way it is performed and in its indications which have undergone dramatic transformations(1). There are accounts of performing caesarean sections since ancient times, and several cultures described performing operations for pregnant women who were “dying” or already deceased to save the fetus (Hindu, Egyptian, Ancient Greece, Roman Empire, China, and in certain European populations). Over time, the methods of performing surgical procedures, the emergence of anesthesia, the control of infections through the discovery of penicillin and the easier access to the medical system through the emergence of hospitals significantly reduced the mortality of pregnant women who, for various reasons, could not give birth naturally(1).
Delivery through caesarean section is an increasingly common surgical procedure worldwide, many of these interventions being performed in the absence of a medical indication. If at the beginning of the 1990s the rate of births by this method was 7% worldwide, according to the World Health Organization (WHO), this percentage has tripled, and the trend tends to be in a constant increase, being estimated to reach a percentage of approximately 29% until 2030(1-3).
Caesarean section was initially seen as a surgical technique meant to save the pregnant woman or the fetus from critical situations. Nowadays, the global prevalence of caesarean sections has increased considerably, the indications for performing these surgical procedures being represented only by major emergencies that endanger the fetus or pregnant woman(1,3). However, WHO raises the alarm about the fact that, in 2021, one out of five children was born by caesarean section, reaching a global rate of 21% from the total number of births(3).
The prevalence of caesarean section differs according to the geographical region. Thus, in less developed countries, such as those from Southern Africa, the prevalence of caesarean sections is low, between 5% and 8%. There are countries, such as those in Latin America and the Caribbean, where four out of ten newborns are born by caesarean section, therefore, of the total number of births, 43% are by caesarean section. In developed countries, the prevalence increased from 7% in the 1990s to 21% today, and continues to grow(3).
We can also discuss the other extreme that we meet in countries such as the Dominican Republic, Brazil, Cyprus, Egypt and Turkey, where the number of caesarean sections is higher than the number of vaginal births(3).
In the United States of America, caesarean deliveries have increased steadily since 1996, reaching the highest value in 2007, representing 32% of all births. The group of women included in the statistics included all women regardless of age, race, geographic area and gestational age(1). For the year 2007, the caesarean delivery rate varied by state from a low level in Utah (22.2%) to a high level in New Jersey (38.3%)(4).
The provisional data provided by the Centers for Disease Control and Prevention (CDC) from 2019, published in May 2020, showed that 31.7% of all births were by caesarean section, and the majority (25,6% of them) were represented by the NTSV population (pregnant primiparous women with potential low-risk births, which means that they have only one full-term fetus in cranial presentation)(1,5,6).
Most pregnant women (86.2%) who gave birth by caesarean section will also have a following birth by caesarean section, because the risk of vaginal birth after a previous caesarean section is very high for the pregnant woman and for fetuses, often leading to a dead fetus, for this reason many hospitals do not encourage these women to give birth vaginally in their units. The CDC reported, in the United States of America, for the year 2019, a low rate of vaginal births after a previous caesarean delivery, of approximately 13.8%(1,8).
The rate of caesarean deliveries in the group of low-risk pregnant women showed a slow upward trend, increasing in 2020 compared to 2019; also, the increase in caesarean deliveries among primiparous pregnant women follows the same increasing trend, representing a percentage of 21.9% in 2020(1,8).
The upward trend of caesarean sections lately brought into discussion the risks that caesarean section involves, both for the mother and for the newborn. The post-surgical complications, the slower mobilization of the women after birth, the impossibility of performing the “skin to skin” technique and the late initiation of breastfeeding are some of the aspects that must be considered when we indicate caesarean section(8).
Also, when the extraction of the fetus takes place in the absence of labor, the newborn may face problems in postnatal adaptation, which will also increase the number of days of hospitalization and, implicitly, the costs of care for these newborns. Regarding the subsequent evolution of newborns extracted by caesarean section, at the pediatric age, it was observed that the lack of passage through the vaginal canal is associated with delayed colonization of the intestinal microbiome, and they have a double risk of manifesting asthma, skin or digestive allergies(8-10).
The increase in the rate of births by caesarean section led to the emergence of the concept of elective caesarean section; thus, antenatal corticoprophylaxis after 37 0/7 weeks of gestation is being discussed more and more frequently to improve the prognosis of neonatal respiratory pathology in newborns at term or close to term(11).
It is well known that vaginal birth participates in fetal lung maturation, through several mechanisms. During physiological delivery and during labor, due to the stress of birth, the serum level of glucocorticoid hormones and catecholamines increases. This abundance of hormones is involved in numerous cellular mechanisms intended to prepare the fetus for extrauterine life, such as increasing the synthesis and expression of amiloride-sensitive Na+ channels (ENaC), aquaporin 5 and Cl- channels at the level of the pulmonary epithelium, through mRNA-type mechanisms, therefore the absorption of alveolar liquid is stimulated(12).
In the case of newborns born by caesarean section, these hormonal changes that have been correlated with favorable neonatal pulmonary adaptation do not appear, making these newborns vulnerable to manifest respiratory complications shortly after birth(13).
Another mechanism involved in pulmonary maturation, in case of vaginal birth, is the elimination of pulmonary fluid during labor through painful uterine contractions and during the passage through the pelvic and vaginal straits, through mechanical pressure forces, which we do not encounter in case of caesarean operations. Considering this aspect, we are discussing the importance of painful uterine contractions before caesarean section, discussing the concepts of “warm” caesarean section and “cold” section(14,15).
There are concerns about the administration of both betamethasone and dexamethasone, due to potential adverse effects on neurological development. However, the data are from animal studies or multi-treatment pregnancies. A follow-up of a study carried out at a high gestational age (over 37 0/7 weeks of gestation) showed subjective differences in the evaluation of children’s learning abilities, but the same study showed that there was no objective difference in neurocognitive development(14,15).
In another study, carried out in the Obstetrics-Gynecology and Neonatology Clinic of the “Elias” University Emergency Hospital, Bucharest, between 2017 and 2019, on 81 newborns from pregnancies with a gestational age between 37 0/7 and 38 0/7 weeks, who received dexamethasone less than seven days before birth, a significant reduction in the need for mechanical ventilation, the use of surfactant and a shortening of the number of days spent in neonatal intensive care units were observed(15).
Subjects and method
This is a retrospective observational study which was carried out over five years (2017, 2018, 2019, 2020 and 2021) in the clinic of the “Elias” University Emergency Hospital, Bucharest. It included 7420 pregnant women, of which 2263 gave birth by natural delivery and 5157 gave birth by caesarean section. All patients included in the study met the inclusion criteria (female patient, pregnant). The exclusion criteria were represented by the absence of pregnancy.
All studied value determinations were made using similar work techniques. The statistical data were systematized in tables and represented by graphs of various types. The Excel program of Microsoft Office was used for data processing and systematization. The graphic representations and the statistical analysis of the data were performed using the same program.
The statistical significance of the results is interpreted according to the value of the p coefficient: if the p value is higher than 0.05, then the results are not statistically significant; for p values between 0.05 and 0.001, the results are considered highly statistically significant, while p values less than 0.001 are considered very highly statistically significant.
Results
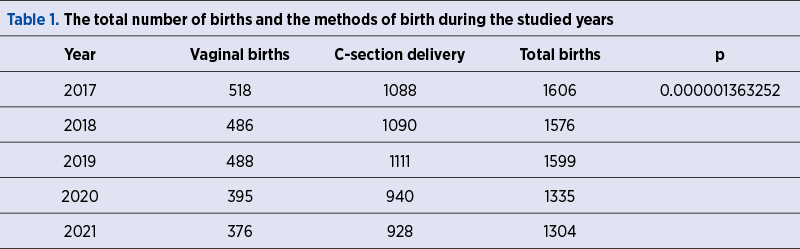
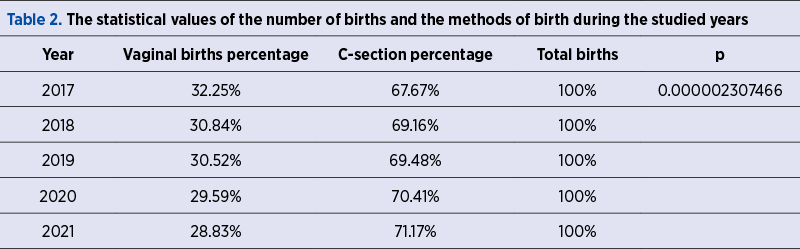
This study included 7420 pregnant women, of which 2263 gave birth by natural delivery and 5157 gave birth by caesarean section (C-section) – Table 1 and Table 2.
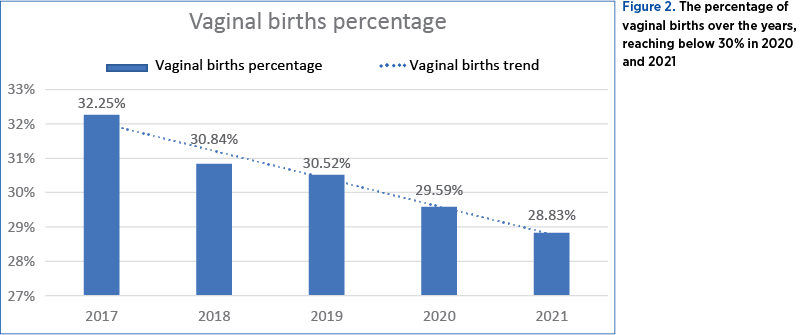
It is observed that, over the years, the rate of vaginal deliveries decreases; thus, in 2019, of the total number of births in our clinic, only 30.54% were through physiological birth, and in 2021 the percentage reached 28.83% (Figure 1 and Figure 2).
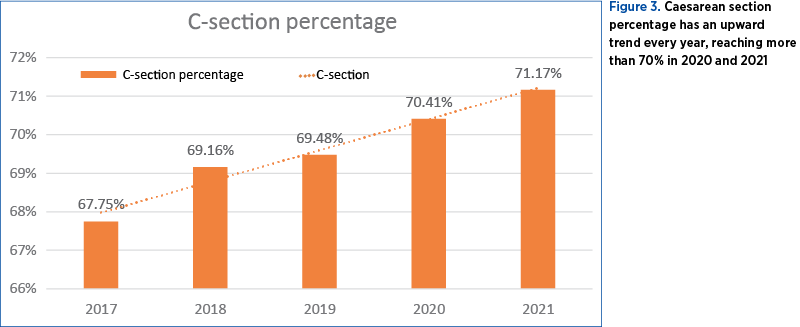
As far as Romania is concerned, there are no exact statistical data related to the prevalence of caesarean deliveries. In our clinic, we performed a statistical analysis over five years (2017, 2018, 2019, 2020, 2021), following the evolution of the mode of birth. Thus, during the five years studied, the trend is clear, the prevalence of caesarean sections being much higher compared to physiological birth, in 2021 the caesarean sections representing 70.17% (Figure 3).
Discussion
It is observed that, over the years, in our clinic, caesarean section has had an upward trend. The risks entailed by caesarean section can impact both the mother and the newborn.
The importance of the pregnant woman’s easy access to medical information regarding the benefits of natural birth (when there are no contraindications) can be discussed. It is well known that labor brings numerous benefits both to the newborn (neonatal adaptation with good prognosis) and to the mother (quick recovery, making the mother-newborn connection, quick initiation of natural nutrition, and lower hospitalization costs). In developing countries, the access to medical information is deficient, and this aspect could explain the increased incidence of caesarean delivery. In the case of our study, we noticed that the incidence of birth by caesarean section is increasing over the years, reaching that, in 2021, approximately 70% of births were by caesarean section.
Conclusions
The upward trend of caesarean sections lately brought into discussion the risks that caesarean section has, both for the mother and the newborn. This trend is observed in case of developing countries, while in developed countries, which have a well-implemented health system, and the pregnant woman has access to health information, spontaneous births are the first intention in terms of the method of birth.
In Romania, there are not enough statistical data regarding the mode of birth, and this article presents the trend regarding the mode of birth in a single university clinic, therefore it is necessary to have a complete database that centralizes the data, so that a more accurate report can be made.
The risks entailed by caesarean section can impact both the mother and the newborn through the immediate and long-term postoperative complications, through the immediate postnatal adaptation of the newborn, but also through the possible subsequent complications that may appear at the pediatric age and, last but not least, by limiting the number of pregnancies and the effects on the family and the birth rate.
The increase in the rate of births by caesarean section led to the emergence of the concept of elective caesarean section; thus, antenatal corticoprophylaxis is discussed after 37 0/7 weeks of gestation, in order to improve the prognosis of neonatal respiratory pathology in newborns at term or close to term.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29-38. doi:10.1097/AOG.0b013e31821e5f65.
-
El-Berry SA, Farag MA, Sharaf El-dine AA, Abdelaty RI, Abu El Fotouh FA. Prophylactic Antenatal Corticosteroid Administration before Elective Cesarean Delivery at or Near Term to Improve Perinatal Outcome. Benha Journal of Applied Sciences. 2020;5(Issue2)Part (1):109-115. doi: 10.21608/bjas.2020.135460.
-
World Health Organization. Caesarean section rates continue to rise, amid growing inequalities in access. 16 June 2021. Available at: https://www.who.int/news/item/16-06-2021.
-
Sotiriadis A, McGoldrick E, Makrydimas G, et al. Antenatal corticosteroids prior to planned caesarean at term for improving neonatal outcomes. Cochrane Database Syst Rev. 2021;12(12):CD006614. https://doi.org/10.1002/14651858.cd006614.pub4.
-
Norwitz ER. Cesarean birth on maternal request. UpToDate. Jun 20, 2022. Available at: https://www.uptodate.com/contents/cesarian-birth-on-maternal-reqest.
-
Chen H, Tan D. Cesarean Section or Natural Childbirth? Cesarean Birth May Damage Your Health. Front Psychol. 2019;10:351. doi:10.3389/fpsyg.2019.00351.
-
Osterman MJK, M.H.S., Hamilton BE, Martin JA, et al. Division of Vital Statistics. Births: Final Data for 2020. February 7, 2022. Available at: https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-17.pdf.
-
Groom K, Brown SP. Caesarean section controversy. BMJ. 2000 Apr 15;320(7241):1072. https://pubmed.ncbi.nlm.nih.gov/10764376.
-
Loo EXL, Sim JZT, Loy SL, et al. Associations between caesarean delivery and allergic outcomes: Results from the GUSTO study. Ann Allergy Asthma Immunol. 2017;118(5):636-638. doi:10.1016/j.anai.2017.02.021.
-
Verbanas P. The Hidden Reason Children Born by C-Section Are More Likely to Develop Asthma. November 11, 2020. https://www.rutgers.edu/news.
-
Elewa AM, Saad AS, Soliman AS, Al Saber SA. Does Corticosteroids Administration after 37 Weeks for Elective Lower Segment Cesarean Section Reduce Neonatal Respiratory Morbidity? A Randomized Controlled Trial. Benha Medical Journal. 2020; Vol. 37, Issue 3. https://bmfj.journals.ekb.eg/article_111732_9913488c33a616a2e28e94d101f3277c.pdf.
-
Süvari L, Janér C, Helve O, et al. Postnatal gene expression of airway epithelial sodium transporters associated with birth stress in humans. Pediatr Pulmonol. 2019;54(6):797-803. doi:10.1002/ppul.24288.
-
Sharfuddin S, Pradha A, Imam N. Prophylactic antenatal corticosteroid before elective cesarean delivery at or near term: a retrospective study. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2019 Mar;8(3):927-931. https://dx.doi.org/10.18203/2320-1770.ijrcog20190859.
-
Saccone G, Berghella V. Antenatal corticosteroides for maturity of term or near term fetuses: systematic review and meta-analysis of randomized controlled trials. BMJ. 2016;335:i5044. https://doi.org/10.1136/bmj.i5044.
-
Kamath-Rayne BD, Rozance PJ, Goldenberg RL, Jobe AH. Antenatal corticosteroids beyond 34 weeks gestation: What do we do now?. Am J Obstet Gynecol. 2016;215(4):423-430. doi:10.1016/j.ajog.2016.06.023.




