Some clinico-therapeutic evaluations and considerations on laryngeal cancer – work carried out in the ENT Clinic of the Craiova County Emergency Clinical Hospital
Evaluări şi consideraţii clincoterapeutice asupra neoplasmului laringian – lucrare efectuată în Clinica ORL a Spitalului Clinic Judeţean de Urgenţă Craiova
Abstract
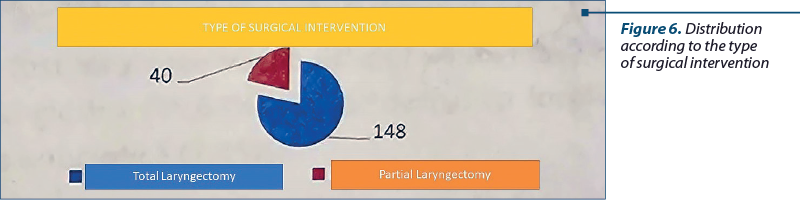
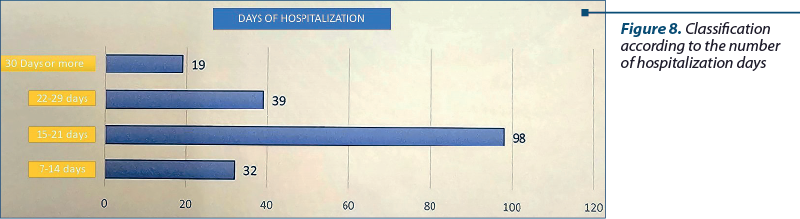
Aim of the paper. Highlighting laryngeal neoplasia through clinical manifestations and therapeutic possibilities. Objective of the study. Achieving topographic localization of larynx with oncologically limited surgical indication. Materials and method. This clinico-therapeutic study was conducted over a period of five years, in the ENT Clinic of the Craiova County Emergency Clinical Hospital. Results. A total of 188 patients were identified between 2015 and 2019, categorized by gender, age, symptoms, place of origin, histopathological examination, staging and types of laryngectomies. Discussion. It was observed that all male patients were smokers, with moderately differentiated squamous carcinoma being the predominant histological type. The dominant symptoms included dysphonia, dysphagia and dyspnea, which also dictated the type of surgical intervention: total laryngectomy in 148 cases and reconstructive partial laryngectomies in 40 cases. The hospitalization period ranged from 15 to 25 days, on average. The postoperative treatment was supplemented with radiation and chemotherapy. Conclusions. Patients should seek medical attention more promptly. Dysphonia and dysphagia were the dominant symptoms. Clinical examination, fiberoscopy and suspended laryngoscopy are useful for assessing the topographic localization of the neoplasm. Surgical intervention is the clinical act for neoplasia removal, complemented by cervical irradiation.Keywords
larynxneoplasmlaryngectomyRezumat
Scopul lucrării. Evidenţierea neoplasmului de laringe prin manifestări clinice şi posibilităţi terapeutice. Obiectivele lucrării. Realizarea localizării topografice laringiene cu indicaţia chirurgicală de exereză în limita oncologică. Materiale şi metodă. Acesta este un studiu clinicoterapeutic, efectuat pe o perioadă de cinci ani, în Clinica ORL a Spitalului Clinic Judeţean de Urgenţă Craiova. Rezultate. Au fost depistaţi 188 de pacienţi în perioada 2015-2019, repartizaţi în funcţie de sex, vârstă, simptomatologie, mediu de provenienţă, examen histopatologic, stadializare şi tipuri de laringectomie. Discuţie. Am constatat că toţi pacienţii de sex masculin au fost fumători, tipul histologic predominant fiind reprezentat de carcinomul scuamos moderat diferenţiat. Simptomatologia dominantă a fost reprezentată de disfonie, disfagie şi dispnee, care a dictat şi tipul intervenţiei chirurgicale, laringectomie totală în 148 de cazuri şi laringectomii parţiale reconstructive în 40 de cazuri. Durata spitalizării a variat, în medie, între 15 şi 25 de zile. Postoperatoriu, tratamentul a fost completat cu iradiere şi chimioterapie. Concluzii. Adresabilitatea bolnavilor către medic ar trebui să fie mai rapidă. Disfonia şi disfagia au fost simptomele dominante. Examinarea clinică, fibroscopică şi laringoscopia suspendată sunt utile pentru aprecierea localizării topografice a neoplasmului. Intervenţia chirurgicală reprezintă actul clinic pentru îndepărtarea neoplaziei, fiind completată de iradierea cervicală.Cuvinte Cheie
laringeneoplasmlaringectomieIntroduction
Detecting laryngeal cancer is relatively straightforward, with one of the signs of laryngeal cancer being hoarseness. Whenever hoarseness persists for more than 4-6 weeks, it should be considered suspicious for the development of laryngeal cancer, both by the patient and the physician. Consequently, the patient should proactively seek the attention of the family doctor and then a specialist for a laryngeal examination. In cases of early suspicion of laryngeal cancer, the risk factors or contributing causes such as smoking and alcohol consumption, as well as precancerous conditions of the larynx, such as hyperkeratosis, calluses or vocal strain, should be considered(1,2).
The rich lymphatic network of the supraglottic region explains the exuberant development of epitheliomas, while the paucity of lymphatics in the subglottic region leads to a slower, infiltrative appearance(2,3). The particular structure of the vocal cords, with extremely reduced lymphatic vessels, explains the clinical situations when the extension is very slow, more exophytic than infiltrative(1,3). Histologically, the majority of tumors are squamous cell carcinomas, with connective tissue cancers of the larynx being extremely rare(2,4).
The positive diagnosis of laryngeal cancer is established based on subjective complaints, corroborated with laryngoscopic examination, exocervical examination, histopathological examination of laryngeal tumor fragments, and radiological examination. The absence of laryngeal crepitus or the presence of a mass is a clinical diagnostic element of neoplasia(5,6).
Glottic cancer manifests as dysphonia, supraglottic cancer as dysphagia, and subglottic cancer as dyspnea, depending on the extent of localization, which can involve one or multiple laryngeal levels. Once diagnosed, laryngeal cancer is treated with surgery, radiation and chemotherapy(2,6).
Unlike other cancer locations, the unique anatomy of the larynx allows for limited surgical procedures (partial laryngectomies) that remove the cancer while preserving important laryngeal functions in cases of early-stage laryngeal tumors(6,7).
In cases of advanced-stage laryngeal cancer, a patient’s life can be saved by the complete surgical removal of the vocal organ (total laryngectomy), a mutilating procedure that eliminates the voice but ensures the patient’s survival. Both mutilating and partial surgeries are followed by consolidation treatment, including complementary radiation therapy, and in cases of lymph node metastases, oncological treatment is added(8-10).
In terms of frequency, compared to other neoplastic locations, in the field of otolaryngology, the larynx represents the most common neoplasia(11-13).
Materials and method
We included a group of 188 patients hospitalized in the ENT Clinic of the Craiova County Emergency Clinical Hospital over a period of five years (from 1 January 2015 to 31 December 2019), diagnosed with laryngeal neoplasms, aged between 41 and 90 years old. For data collection, analysis and interpretation, we used the following parameters: medical history, ENT clinical examination, paraclinical examinations, imaging studies (cervical ultrasound, chest X-ray, cervicothoracic computed tomography), endoscopic examination (suspended laryngoscopy), and tumor biopsy with histopathological examination.
Results
We analyzed the 188 cases of laryngeal neoplasms over the five-year study period and we observed the following annual distribution: in 2015 – 36 patients (19.15%); in 2016 – 33 patients (17.55%); in 2017 – 35 patients (18.62%); in 2018 – 44 patients (23.40%); in 2019 – 40 patients (21.28%).
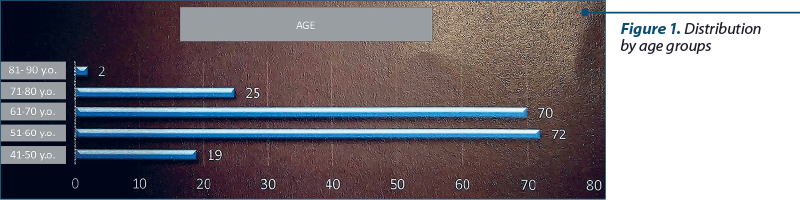
Regarding the age groups of patients with laryngeal neoplasms, we found that in the 41-50 years old age group, there were 19 cases (10.10%), in the 51-60 years old age group we had 72 cases (38.30%), followed by the 61-70 years old age group (70 cases; 37.23%), the 71-80 years old age group (25 cases; 13.29%), and the 81-90 years old age group (two cases; 1.06%).
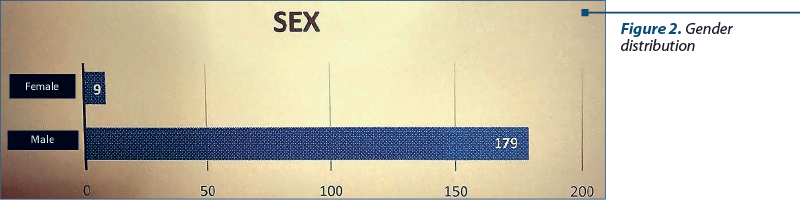
Analyzing patients based on gender, we encountered 179 cases of males (95.21%) and nine cases (4.79%) of females with laryngeal neoplasms, over the course of five years.
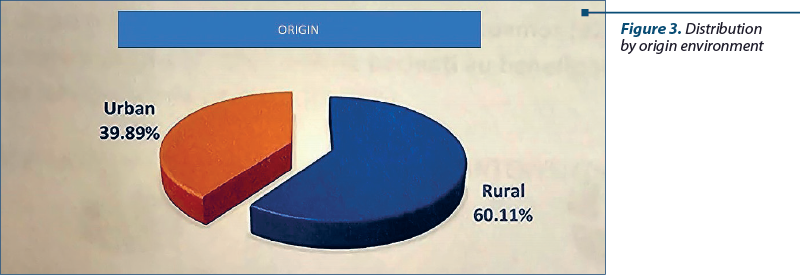
Regarding the patient’s places of origin, those with laryngeal neoplasms had different distribution: 75 patients (39.89%) originated from urban areas, while 113 came from rural areas (60.11%).
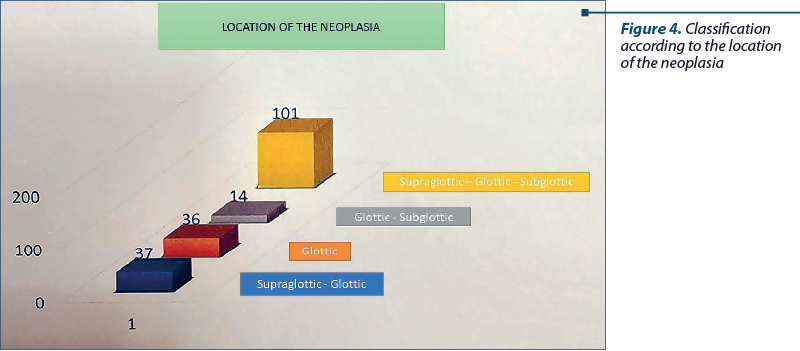
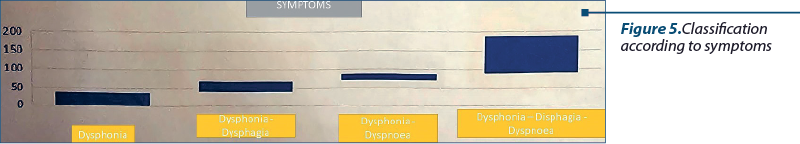
From the patient history obtained, we noted that the triad of dysphonia, dysphagia and dyspnea was encountered in 101 patients (53.72% of cases), which was confirmed during the laryngoscopic examination by the localization of the tumor in the vestibulo-glottic-subglottic region.
Simple dysphonia was observed in 36 patients, where laryngoscopy identified tumor changes on the right vocal cord in 21 cases, on the left vocal cord in 14 cases, and on both vocal cords in a single case.
Patients complaining of dysphagia were found in three cases, and laryngoscopic examination revealed an epiglottic tumor in a single case and ventricular bands in two cases, concomitant with bilateral jugulocarotid adenopathy for which both laryngeal and adenopathy surgical interventions were performed.
Exocervical examination was essential through palpation of the larynx, which showed the absence of laryngeal crepitus in the vestibulo-glottic localization and the presence of laryngeal plastron in 20 cases.
Unilateral jugulocarotid adenopathies were present in 50 cases, while bilateral adenopathies were present in 126 cases. No adenopathies were found in patients with glottic localization (cordal) – 12 cases.
All patients with vocal functional changes, dysphagia and macroscopic endolaryngeal changes were admitted to the ENT Clinic in Craiova. After prior cardiopulmonary, hepatic, renal and blood preparation, laryngoscopic, fiberoptic and suspended laryngoscopy examinations were performed, along with tumor biopsies. The tumor fragments collected were sent for microscopic histopathological examination, confirming the macroscopic suspicion of neoplasia.
The histological type found in biopsied patients revealed moderately differentiated squamous cell carcinoma in 170 cases, in situ carcinoma in 14 cases, verrucous carcinoma in one case, rhabdoid carcinoma in one case, synovial sarcoma in one case, and carcinosarcoma in one case.
The surgical interventions performed on the patients included cordectomy in 30 cases, bicordocomissural laryngectomy in one case, frontolateral laryngectomy in five cases, anterior frontal laryngectomy in one case, and supraglottic horizontal laryngectomy in three cases.
Total laryngectomy was performed on 148 patients, involving two or more laryngeal levels. Jugulocarotid lymphadenectomy was performed in the same surgical session as partial or total laryngectomy.
The microscopic examination of the jugulocarotid adenopathy revealed metastases in 31 cases, while no metastatic changes were found in 157 cases. The microscopic examination of the excised larynx showed cartilaginous invasion in 71 cases (patients with a plastron), muscular invasion in 56 cases, perineural invasion in 36 cases, and vascular invasion in 14 cases.
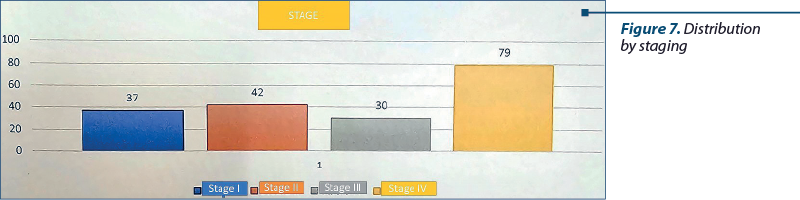
The patients were also analyzed based on staging. Consequently, stage I was encountered in 37 cases, including all patients with cordal localization, stage II was encountered in 42 patients, stage III was encountered in 30 patients, and stage IV was encountered in 79 patients.
Postoperative care. Patients who underwent total laryngectomy, supraglottic horizontal laryngectomy and cordectomy received surgical intervention under general anesthesia. Postoperatively, they were provided with a nasoesophageal liquid feeding tube for 12-14 days and a suprasternal tracheal cannula. Sterile postoperative cervical dressings were applied daily, and the tracheal cannula was cleaned multiple times a day.
Simultaneously, antibiotics were administered systemically for 10 days, until the suture threads were removed. Antisecretory treatment was given to reduce salivary secretion, and hyperproteic intravenous treatment was provided for 12 days. At seven days postoperatively, the sutures at the cervical flap were removed, and at 10 days, the tracheal fixation sutures were removed. At 12 days postoperatively, a methylene blue test was performed to check for fistula by administering diluted methylene blue in drinking water, and the feeding tube was removed.
For patients who underwent supraglottic horizontal laryngectomy, the feeding tube was removed around 20 days, considering the arytenoid edema, which hindered glottis closure and led to a false pathway for liquid aspiration into the trachea.
The tracheal cannula was permanent for patients with total laryngectomy and temporary (48 hours) for those with cordectomy, while for supraglottic horizontal laryngectomy, it was maintained for five days.
Two weeks after discharge, all patients were included in the oncology service for radiation therapy. Chemotherapy was administered only to those with lymph node metastases.
Discussion
In the five years of studying patients with laryngeal neoplasms, we observed that the annual distribution remained relatively constant, with the highest number recorded in 2018 (23.40%), followed by 2019, with a percentage of 21.28%.
Laryngeal neoplasms were predominantly found in the 51-60 years old age group (38.30%), followed by the 61-70 years old age group (37.23%). The youngest patients were in the 41-50 years old age group (10.40%), while the oldest were in the 81-90 years old age group (1.06%).
The risk factors for laryngeal neoplasia were primarily associated with smoking and alcohol consumption. Men accounted for 95.21% of cases, with a predominantly rural origin of 60.11%.
The symptomatology was dominated by dysphonia, especially when the tumor was located in the vocal cord or in conjunction with neighboring levels such as supraglottic or subglottic. It is recommended for patients to seek medical attention after persistent dysphonia for 4-6 weeks. Dysphagia was often accompanied by adenopathy, as the supraglottic region is rich in lymphoid tissue and can invade the piriform sinus(14,15).
Early presentation to the doctor is beneficial for patients because it allows for partial surgical interventions while preserving unaffected laryngeal levels. Ninety-five percent of laryngeal carcinomas are treatable. The choice between radiotherapy and surgery depends on the tumor’s location and stage(14,16). For glottic cancers T1N0 and some T2N0 tumors, exclusive radiotherapy can yield similar results to surgery. There were no patients who underwent exclusive radiation therapy in this study(17,18). Cordectomy was indicated for mobile vocal cord carcinoma T1N0 or T2N0. Vertical or horizontal partial laryngectomies were performed to preserve vocal and respiratory functions. Total laryngectomy was indicated when the tumor involved two or three laryngeal levels or extended beyond the larynx, affecting neighboring organs such as the tongue, hypopharynx, thyroid gland or trachea(19,20).
After total laryngectomy, breathing is only possible through a tracheostomy, while swallowing becomes normal after the surgical wound heals. The voice is lost, but it can be partially regained through esophagophony (esophageal voice) or the use of an electronic voice device(20,21).
The principle of the esophageal voice is based on the belching of air in the esophagus, either by swallowing or by pressing the tongue and then belching, which causes the remaining structures of the pharynx to come into operation that produce a sound which can be modulated by the articulation mechanism of speech. Erigmophonation is superior to any type of laryngophone or phonator button(2,21).
Staging in the five years of the study was dominated by stages III and IV. Operated and discharged patients received monthly follow-ups in the first year, which then extended to medical checkups every two, three or four months, or when new symptoms appeared(21,22).
Patients were instructed to daily clean their tracheal cannulas, avoid cold exposure and protect their tracheal stomas from impurities.
Clinical and surgical recovery of laryngectomized patients provides psychological comfort and well-being, with proper nutrition playing a crucial role in maintaining good health(2,6,12,22).
Through its major functions, namely phonation, respiration and nutrition, the larynx is a vital organ that has interested and continues to interest ENT doctors worldwide in performing less mutilating surgeries, while ensuring the eradication of cancerous lesions within oncological safety limits(1,3,7,11,16,19).
As evidence of early interest in laryngeal cancer surgery, in 2023 we mark 150 years since the first laryngeal operation, performed by Theodor Billroth in 1873.
Conclusions
1. The high frequency of laryngeal cancer at the Otolaryngology Clinic in Craiova suggests a long-standing interest in laryngeal surgical interventions, dating back to 1956.
2. Early detection of laryngeal cancer allows for partial laryngectomies to be performed.
3. Late presentation in stages III and IV leads to mutilating surgeries, with the permanent use of a tracheal cannula.
4. Spontaneous functional phonation recovery has increased patients’ confidence, leading them to adopt a healthy lifestyle and maintain a proper nutrition.
5. Continuous monitoring of laryngectomized patients is essential for the success of laryngeal cancer surgery.
Acknowledgement. This work was supported by the grant POCU/993/6/13/153178, “Perfomanţă în cercetare” (“Research performance”), co-financed by the European Social Fund within the Sectorial Operational Program Human Capital 2014-2020.
Conflict of interest: none declared
Financial support: none declared
This work is permanently accessible online free of charge and published under the CC-BY.
Bibliografie
- Bogdan CI. Foniatrie Clinică. Ed. Viaţa Medicală Românească, Bucureşti, 2001.
- Brook I. Ghidul pacientului laringectomizat. Ed. Printech, 2019.
- Obreja S, Ioniţă E, Mitroi MR, Ioniţă I. Îndreptar Terapeutic ORL. Ed. Sitech, Craiova, 2010.
- Anghelide R, Sbenghe-Ţeţu L. Aspecte de patologie oto-rino-laringologică. Ed. Medicală, Bucureşti, 1986.
- Sarafoleanu C, Popescu I, Ciuce C. Tratat de chirurgie – Otorinolaringologie şi chirurgie cervico-facială, Vol. I. Ed. Academiei Române, Bucureşti, 2012
- Woodson GE. Laryngeal and pharyngeal function. In: Cummings CW, Flint PW, Harker LA, et al (Eds.). Cummings Otolaryngology – Head and Neck Surgery, 4th Ed., Mosby, 2005;85:1963-74.
- Weisman RA, Moe KS, Orloff LA. Neoplasms of the Larynx and Laryngopharynx. In: Snow JB, Ballanger JJ (Eds). Ballenger’s Otorhinolaryngology. Head and Neck Surgery. Hamilton: BC Decker Inc, 2003; p. 1255-1297.
- Kleinsasser 0, Glau H. Microcarcinoma and microinvasive carcinoma. Clinical Oncology. 1982;(1):479-487.
- Friedman S, Tellez S. Ljubljana classification of epithelial hyperplastic laryngeal lesions. Histopathology. 1999;35:(6):579-589.
- Fleskens S, Slootweg P. Grading systems in head and neck dysplasia: their prognostic value, weaknesses and utility. Head & Neck Oncology. 2009;1:11.
- Remacle M. Inflammatory diseases and lasers. In: Anniko M, Sprekeslsen MB, Bonkowsky V, et al. (Eds.). Otorhinolaryngology, Head and Neck Surgery. European Manual of Medicine. Berlin, Springer, 2010; p. 475-481.
- Sarafoleanu D. Tumorile maligne ale laringelui. In: Sarafoleanu C (Ed.). Esenţialul în laringologie. Bucureşti, Ed. Academiei Române, 2007;(14):321-351
- Sarafoleanu C. Stările precanceroase ale laringelui. În: Sarafoleanu C (Ed.). Esenţialul în laringologie. Bucureşti, Ed. Academiei Române, 2007;(12):287- 298.
- Dahlstrom KR, Adler-Storthz K, Etzel CJ, et al. Human papilloma-virus type 16 infection and squamous cell carcinoma of the head and neck in never-smokers: a matched pair analysis. Clinical Cancer Research. 2003;9:2620-6.
- Severin E. Patologia genetică a laringelui. În: Sarafoleanu C (Ed.). Esenţialul în laringologie, Ed. Academiei Române 2007;3:77-112.
- Gale N, Pilch BZ, Sidransky D, Westra W, Califano J. Tumours of the hypopharynx, larynx and trachea (epithelial precursor lesions). In: Barnes L, Eveson JW, Reichart P, Sidransky D (Eds.). World Health Organization Classification of Tumours. Pathology & Genetics. Head and neck tumours. International Agency for Research on Cancer (IARC), Lyon: IARC Press, 2005;140-143.
- Barnes L, Tse LLY, Hunt JL, et al. Tumours of the hypopharynx, larynx and trachea: Introduction. In: Barnes L, Eveson JW, Reichart P, Sidransky D (Eds.). World Health Organization Classification of Tumours. Pathology & Genetics. Head and neck tumours. IARC Press, Lyon, IARC Press, 2005;107-117.
- Adams GL, Maisel RH. Malignant tumors of the larynx and hypopharynx. In: Cummings CW, Flint PW, Harker LA, et al. (Eds). Cummings Otolaryngology Head and Neck Surgery, 4th Ed. Mosby, 2005;(99):2222- 83.
- Rafferty MA, Fenton JE, Jones AS. The history, aetiology and epidemiology of laryngeal carcinoma. Clinical Otolaryngology. 2001;26(6):442-446.
- Sarafoleanu C. Tumorile benigne ale laringelui. În: Sarafoleanu C (Ed.). Esenţialul în laringologie. Bucureşti: Ed. Academiei Române. 2007;(13):299-319.
- Barnes L, Ferlito A, Altarilla G. Basaloid squamous cell carcinoma of the head and neck clinicopathological features and differential diagnosis. Ann Otol-Rhinol Laringol. 1966;105(1):75-82.
- Kleinssaser O, Gluck H. Microcarcinoma and microinvasive carcinoma. Clin Oncol. 1982;1:479-487.





