Acute appendicitis is one of the most common causes for acute abdomen in pediatric populations and appendectomy is the most common surgical procedure performed in pediatric emergency surgery. Also, although there are almost 40 years since the first laparoscopic appendectomy was performed, there is no general consensus regarding the benefits of this procedure, and open appendectomy is still the conventional technique in some pediatric surgery departments. The aim of this study is to retrospectively compare the laparoscopic appendectomy with the open approach, in terms of length of surgery, length of stay and frequency of complications.
Apendicectomia laparoscopică versus cea deschisă în tratamentul apendicitei acute la copii
Laparoscopic versus open appendectomy in the management of acute appendicitis in children
First published: 16 decembrie 2020
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Pedi.60.4.2020.4070
Abstract
Rezumat
Apendicita acută este una dintre cele mai frecvente cauze de abdomen acut la populaţia pediatrică, iar apendicectomia este cea mai frecventă procedură chirurgicală efectuată în chirurgia pediatrică de urgenţă. Deşi sunt aproape 40 de ani de la prima apendicectomie laparoscopică, nu există un consens general cu privire la beneficiile acestei proceduri, iar apendicectomia deschisă este încă tehnica convenţională utilizată în unele secţii de chirurgie pediatrică. Scopul acestui studiu este de a compara retrospectiv apendicectomia laparoscopică şi abordarea deschisă, în ceea ce priveşte durata intervenţiei chirurgicale, durata spitalizării şi frecvenţa complicaţiilor.
Introduction
Appendectomy has been the standard of care for appendicitis since the late 1800s. First described in 1886 by Reginald Fitz, it continues to be the most common abdominal pathology, and appendectomy remains one of the most frequently performed surgical interventions in children. Open appendectomy has remained the optimum therapeutic intervention in the management of acute appendicitis for over a century, after it was first described by McBurney in 1894(1), due to its associated minimal and favourable morbidity and mortality rates. Following the exponential advances in science and technology and the development and improvement in laparoscopic surgeries, Semn, a German gynecologist, described and performed the first laparoscopic appendectomy in 1984(2).
Just over three decades later, there is still an ongoing debate over the benefits of each technique. With laparoscopic appendectomy gradually replacing open appendectomy and becoming a standard therapeutic approach in developed countries, this study aims to evaluate the statistical difference between laparoscopic and open appendectomy, and to highlight the significant differences – if any – between both approaches, in the management of different stages of acute appendicitis, while assuming no preference for either.
Materials and method
Between 2012 and 2018, a total of 932 children who underwent appendectomy, performed by different surgeons at the “Sf. Maria” Emergency Clinical Hospital for Children, Iaşi, Romania, were charted and retrospectively reviewed.
The inclusion criteria were patients ≤18 years old, with the main diagnosis of acute appendicitis, using the International Classification of Diseases (ICD-10) codes for appendicitis. The gender of the patients was not especially considered as a selection criterion. The patients who underwent appendectomy presented with common symptoms of acute appendicitis, including right lower quadrant pain, fever, anorexia, nausea and vomiting. The biological findings, such as leukocytosis and elevated C-reactive protein, were considered during the diagnosis of the selected patients.
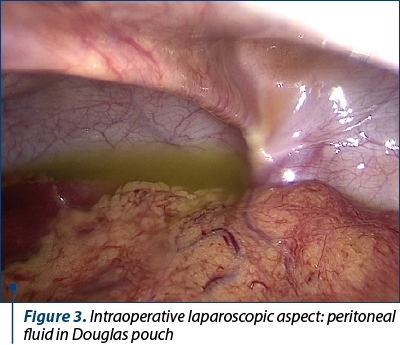
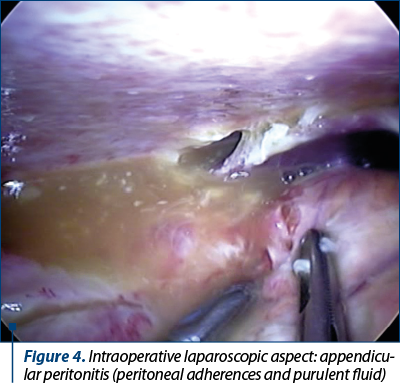
The patients who met these criteria were divided into two groups: those who underwent open appendectomy (OA), and those who had laparoscopic appendectomy (LA). These groups (OA and LA) were further subdivided into three subgroups: simple acute appendicitis, acute appendicitis with general peritonitis, and acute appendicitis with peritoneal abscess (Figure 1). These subdivisions were supported by the data obtained from the patients’ medical reports, including the ICD-10 codes and the pathological reports.
The duration of each type of surgery (OA and LA), the duration of hospital stay after the respective surgical interventions and the postoperative complications for each subgroup were obtained and analyzed, with their mean and standard deviation, before finally determining their significance through the p value, using the Student’s t-test against a p (alpha) value of 0.05.
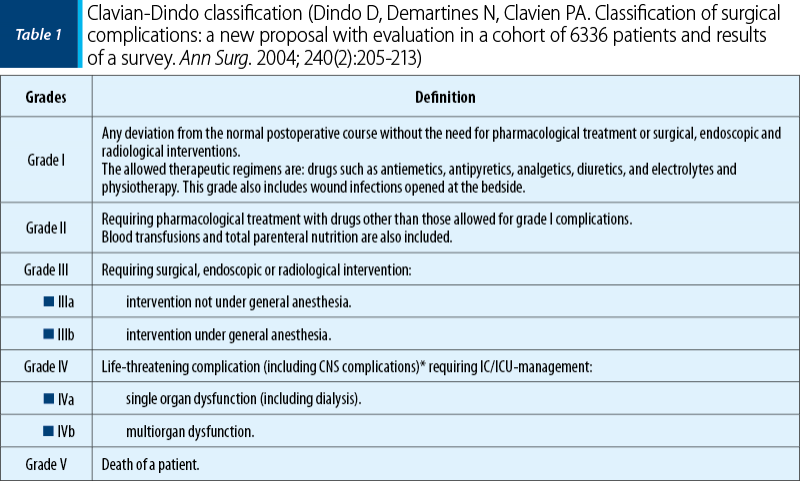
The postoperative complications were also grouped according to the Clavien-Dindo classification into seven grades (Table 1).
Results
A total of 932 patients were selected for this study, based on all inclusion criteria: 76% of them had open appendectomy, and 24% underwent laparoscopic appendectomy, with an average age of 12.2±3.6 years old and 12.7±3.7 years old, respectively.
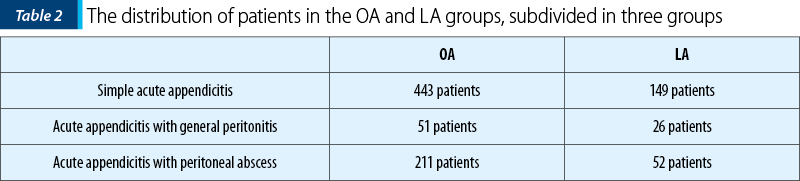
Out of these patients, 705 were in the open appendectomy (OA) group, and 227 patients in the laparoscopic appendectomy (LA) group. Each group was subdivided into three groups, presented in Table 2.
The age and gender of the patients had no statistical significance amongst each corresponding OA or LA group.
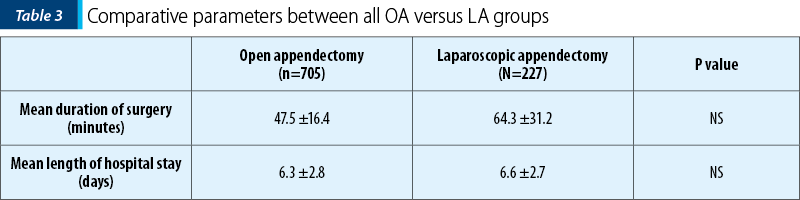
An overview of OA and LA, irrespective of the stage of acute appendicitis, shows a longer duration of surgery associated with LA compared to OA, but without a significant difference between both approaches (p>0.05).
Data such as the duration of each type of surgery (OA and LA), the duration of hospital stay after the respective surgical interventions, and the postoperative complications for each subgroup – simple acute appendicitis, acute appendicitis with general peritonitis, and acute appendicitis with peritoneal abscess – were analyzed (Table 3).
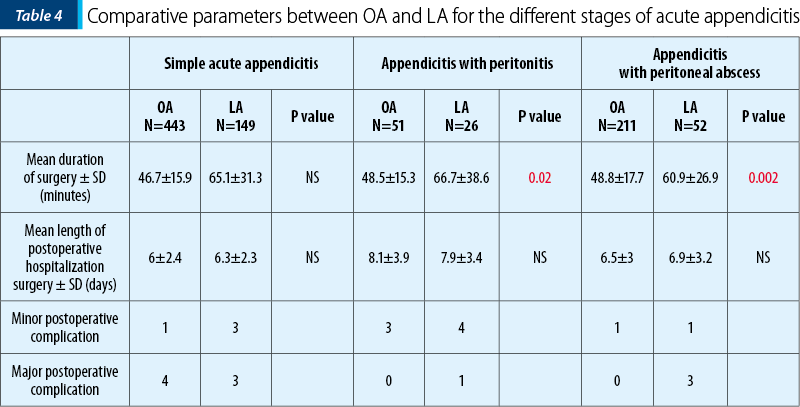
A look at the mean duration for the LA group shows a longer surgical duration compared to the mean surgery duration for the OA in all subgroups of patients. Although there is a variation in the mathematical numbers, the standard deviation suggests a closer relationship than the one suggested by just the simple mathematical numbers. Moreover, no statistical significance was observed between both OA and LA groups, within the subgroup of patients treated for simple acute appendicitis, with a p value >0.05 denoted as NS (not significant). The statistical significance was noted within the subgroup of patients who had acute appendicitis with peritonitis and appendicitis with peritoneal abscess, with a p value <0.05 (=0.02) – Table 3.
The average length of stay at the hospital marked by the time interval between recovery room and discharge was recorded mathematically to be longer but only obscurely for patients in the LA group compared to the patients in the OA group. A two-tailed t-test demonstrated no statistical difference between the OA and LA for each subgroup of patients.
Regarding the postoperative complications, for simple acute appendicitis, one grade I complication associated with open appendectomy (fever) and four grade II complications – readmission within 30 days for reevaluation for symptoms already ruled out – were recorded. The complications after laparoscopic surgery included three grade I complications (ileus) and three grade III complications – bowel adhesion and obstruction.
For patients who had acute appendicitis with peritonitis, managed with open appendectomy, three grade I complications (vomiting and two surgical wound infections) were recorded. Laparoscopic appendectomy was associated with four grade I complications (prolonged ileus) and one grade III complication (bowel adhesion and bowel obstruction).
Regarding patients who had acute appendicitis with peritoneal abscess, one grade I complication (postprocedural wound infection) was described. Also, one case of diarrhea (minor complication) associated with laparoscopic appendectomy and three grade III complications (bowel adhesion and obstruction) were reported.
Discussion
A number of studies and articles have been published, citing several comparative merits of laparoscopic appendectomy over open appendectomy in the management of both complicated and uncomplicated appendicitis in children, including minimal postoperative pain in comparison to open appendectomy, shorter postoperative hospital stay, favourable aesthetics and shorter recovery time. Most of the published studies that have focused on different parameters – especially the duration of surgery, the recovery time and postoperative complications, the duration of antibiotics administration, including readmission – have diverse results and conclusions, which have aided the long debate between open and laparoscopic appendectomy(14,15). Such variations were not lacking in this study as well, with some results corresponding and others differing from other published studies.
In an effort to compare the aforementioned parameters in both open appendectomy and laparoscopic appendectomy, we first disregarded the stage of appendicitis and just focused on the type of management employed. In this scenario, 227 patients of the 932 patients in the study had laparoscopic appendectomy and 705 had open appendectomy. The wide variation between the quantities of both samples didn’t go unnoticed, providing this study with an increased margin of error, with the sample size for open appendectomy about three times than that of laparoscopic appendectomy.
Most of the studies recorded a longer duration of surgery with laparoscopic approach than with open appendectomy(2,3-5,9), whereas few studies reported similar or even shorter operating time with laparoscopic approach(6-8). In our study, the duration of laparoscopic appendectomy was considerably longer than the duration of open appendectomy (63.4±31.2 versus 47.5±16.4 minutes). This observation corresponds to the numerous studies previously published, although its significance is challenging. This difference, clearly uncontestable, still leaves an open debate as to why it exists. This fact may be explained by the learning curve in a technique that was only started in 2013 at the “Sf. Maria” Emergency Clinical Hospital for Children, the cohort studied including the initial years of minimal invasive approach.
In an attempt to find whether the duration of surgery is influenced by the stage of appendicitis, we compared the group who had simple appendicitis and underwent either OA or LA versus complicated appendicitis (with peritonitis or peritoneal abscess). Even though the duration of surgery was longer in LA (65.1±31.3 minutes) than in OA (46.7±15.9 minutes), this difference in surgery duration was insignificant in simple acute appendicitis (p>0.05), but highly significant in the management of complicated acute appendicitis (with peritonitis/abscess) – p<0.05.
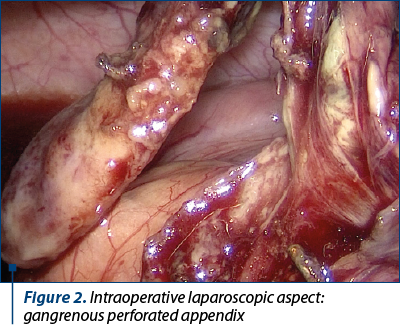
The visualization is better in laparoscopy, as you have magnification, therefore offering a broader examination of the abdominal cavity and inspection of all organs, such as identifying a hernia or ovarian cyst in the examination of the female internal genitalia. LA also offers a better operating field and access in case of an abnormally located appendix like a subhepatic one, in which McBurney incision is difficult.
Another important factor with a direct influence on patient’s management is the length of hospital stay. When we compared the duration of hospital stay after surgery, we found no difference of significance between laparoscopic appendectomy and open appendectomy (6.6±2.7 versus 6.3±2.8, respectively). Some studies have recorded different results regarding this parameter, favouring either OA or LA, while others, like this study, have recorded a square result. On the other hand, many studies have shown that the length of hospital stay for the patients who underwent laparoscopic appendectomy was significantly shorter(3,4,6). Those differences can be attributed to the experience and skills of the surgeons, as well as the different discharge policies in different medical facilities.
The complications after surgery, whether minor or major, are arguably the most important factor in the debate between open and laparoscopic appendectomy. With a high prevalence of acute appendicitis, a safe management is of utmost importance, hence the need for an approach with minimal complications.
In this study we have grouped these complications according to Clavian classification. We have found some minor type complications, such as postoperative fever, vomiting or stool changes (± ileus), postoperative wound infection, and major complications, including bowel adhesion and obstruction, and readmission. We found that the minor complications were more frequent in the LA group than in the OA group, but there was no difference regarding the major complications. Other studies have shown a lower complication rate in patients who underwent laparoscopic appendectomy(12). In a retrospective study by Tsai Ching-Chung et al., in Taiwan(13), they recorded fewer minor and major postoperative complications in laparoscopic appendectomy than in open appendectomy, from a study sample of 177 children.
Conclusions
These study results point out the differences between laparoscopic appendectomy and open appendectomy, but this difference does not suggest a favoured maneuver.
Just over three decades later after the first LA, there is still an ongoing debate over the benefits of each technique. Supporters of the OA find it easy and fast to perform and they consider that this technique has a lower rate of abdominal abscess. On the other hand, in case of LA, the operative time can be reduced after training. It is less painful and it has less wound infections and postoperative ileus. Other complications have the same rate as with OA.
It is undeniable that the choice of surgical approach in the management of appendicitis, although reliant on numerous studies, is influenced by the personal preference, the surgical skills, the resource availability and the patients’ expectation.
This study particularly focused on the comparative significance of the duration of surgery and the postoperative hospital stay between open appendectomy and laparoscopic appendectomy in the management of simple acute appendicitis and complicated appendicitis – with generalized peritonitis and peritoneal abscess, in children, concluding that laparoscopic appendectomy is a feasible technique in the management of acute appendicitis just as much as open appendectomy.
Bibliografie
-
McBurney C. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg. 1894;20(1):38-43.
-
Semm K. Endoscopic appendectomy. Endoscopy. 1983;15(2):59-64.
-
Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177(3):250-6.
-
Azaro EM, Amaral PC, Ettinger JE, Souza EL, Fortes MF, Alcantarag RS, et al. Laparoscopic versus open appendicectomy: A comparative study. JSLS. 1999;3(4):279-83.
-
Bennett J, Boddy A, Rhodes M. Choice of approach for appendicectomy: a meta-analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech. 2007;17(4):245-55.
-
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1-12.
-
Hellberg A, Rudberg C, Kullman E, Enochsson L, Fenyö G, Graffner H, et al. Prospective randomized multicentre study of laparoscopic versus open appendicectomy. Br J Surg. 1999;86(1):48-53.
-
Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R. Laparoscopic versus open appendectomy. A prospective randomized double-blind study. Ann Surg. 2005;242(3):439-50.
-
Ikeda H, Ishimaru Y, Takayasu H, Okamura K, Kisaki Y, Fujino J. Laparoscopic versus open appendectomy in children with uncomplicated and complicated appendicitis. J Pediatr Surg. 2004;39(11):1680-5.
-
Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V, et al. Laparoscopic versus open appendectomy in children a meta-analysis. Ann Surg. 2006;243(1):17-27.
-
Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic appendectomy study group. Am J Surg. 1995;169(2):208-12.
-
Heikkinen TJ, Haukipuro K, Hulkko A. Cost-effective appendectomy. Open or laparoscopic? A prospective randomized study. Surg Endosc. 1998;12(10):1204-8.
-
Tsai CC, Lee SY, Huang FC. Laparoscopic versus open appendectomy in the management of all stages of acute appendicitis in children: a retrospective study. Pediatrics and Neonatology. 2012 Oct;53(5):289-94.
-
Ali R, Anwar MA, Akhtar J. Laparoscopic versus open appendectomy in children: a randomized controlled trial from a developing country. Journal of Pediatric Surgery. 2018 Feb;53(2):247-249.
-
Svensson JF, Patkova B, Almström M, Eaton S, Wester T. Outcome after introduction of laparoscopic appendectomy in children: A cohort study. Journal of Pediatric Surgery. 2016 Mar;51(3):449-53.
Articole din ediţiile anterioare
Cardiopatie dilatativă la un adolescent – prezentare de caz
Heart failure is a rare but serious diagnosis in pediatric patients.
Un caz rar de boală de stocaj a fibrinogenului hepatic la un copil – prezentare de caz
Boala hepatică de stocare a fibrinogenului este o afecţiune genetică rară, cu transmitere autozomal dominantă, caracterizată de acumularea de fi...
Bronșiectaziile non-fibrochistice
Bronșiectazia este definită clinic prin dilatația permanentă și ireversibilă a calibrului bronhiilor, asociată cu inflamația și infecția croni...
Transmiterea hepatitelor B și C de la mamă la copil - o problemă actuală
Hepatitele cronice la copil sunt încă în actualitate, prin evoluția particulară și dificultățile de tratament. Transmiterea verticală rămâne o mo...