Traumatismele abdominale la copii – experienţa unui singur centru pe o perioadă de un an
Abdominal trauma in children – one-year single-center experience
Abstract
Trauma is the leading cause of childhood morbidity and mortality. With newer technologies, clinical guidelines and minimally invasive interventions, the management of trauma is different today than just a few years ago. There are multiple imaging and treatment protocols for clinicians to follow, but we need to highlight that every pediatric patient is unique, owing to the mechanism of injury or their characteristics. The objective of this study was to investigate patients presented to our emergency department during one calendar year, with blunt abdominal traumas, by reviewing their characteristics, the degree of intraabdominal solid organs injuries (according to biological and imaging findings), and the association with the nonoperative or operative management. The total number of patients included in the study groups was 102, with an average age of 8.3 ± 3.2 years old (6 months to 17 years old). The most common cause of trauma was physical assault (24.5%) followed by falling from height (23.5%). Regarding the treatment, 90 of the patients received conservative methods and 12 of them required surgery due to hemodynamic instability. The mean hospital length of stay was 9.3 days; 17 patients were hospitalized in the intensive care unit, and the remaining patients were hospitalized in the surgery department. The evaluation and management of pediatric abdominal trauma have changed significantly in the last decades, conservative treatment becoming a universal standard management implemented worldwide in stable children with favorable clinical outcomes.Keywords
abdominal traumachildrenRezumat
Trauma este principala cauză a morbidităţii şi mortalităţii la copii. Datorită tehnologiei moderne, ghidurilor clinice şi intervenţiilor minim invazive, managementul traumei este diferit actualmente faţă de acum câţiva ani. Există mai multe protocoale imagistice şi de tratament pe care medicii trebuie să le urmeze, dar trebuie să subliniem că fiecare pacient pediatric este unic, din cauza mecanismului leziunii sau a caracteristicilor acestora. Obiectivul acestui studiu a fost acela de a analiza pacienţii care s-au prezentat în cadrul unităţii de primiri urgenţe pe parcursul unui an calendaristic cu traumatisme abdominale contondente şi am analizat caracteristicile acestora, gradul leziunii organelor solide intraabdominale (conform rezultatelor biologice şi imagistice) şi asocierea cu managementul conservator (nonoperatoriu) sau chirurgical. Numărul total de pacienţi incluşi în lotul de studiu a fost de 102, cu o vârstă medie de 8,3 ± 3,2 ani (6 luni până la 17 ani). Cea mai frecventă cauză a traumei a fost agresiunea fizică (24,5%), urmată de căderea de la înălţime (23,5%). Referitor la tratamentul pacienţilor incluşi, 90 dintre aceştia au fost trataţi conservator, nonoperatoriu, şi doar 12 au necesitat intervenţii chirurgicale din diferite cauze care au dus la instabilitate hemodinamică. Durata medie de spitalizare a fost de 9,3 zile. 17 pacienţi au fost internaţi în secţia de terapie intensivă, restul necesitând supraveghere pe secţia de chirurgie. Evaluarea şi managementul traumatismelor abdominale pediatrice s-au schimbat semnificativ în ultimele decenii, tratamentul conservator devenind managementul standard universal implementat la nivel mondial, cu rezultate clinice favorabile în cazul copiilor stabili.Cuvinte Cheie
traumatism abdominalcopiiIntroduction
Trauma is the leading cause of childhood morbidity and mortality. Abdominal injuries represent the third most common type of trauma in children, after head and chest injuries, and the most common cause of death due to unrecognized lesions. Blunt trauma accounts for more than 80% of abdominal trauma at a young age and represents about 11-26% of total laparotomies. There are certain mechanisms of injury in the pediatric population, the main causes being traffic accidents, trauma caused by falling from a height altitude and physical attacks(1-4).
Children have an increased risk of suffering injuries of intraabdominal organs after a blunt abdominal trauma due to their anatomical and physiological characteristics. Compared to the adult population, children have a higher elasticity of the body, the intraabdominal organs are proportionally larger and relatively close to each other, they have a smaller adipose panniculus, an abdominal wall with less muscle layer, and an incompletely ossified chest cage that provides limited protection of the liver, spleen and kidneys (most commonly injured organs)(5-8).
The field of trauma is expanding and pediatric trauma is no exception. With newer technologies, clinical guidelines, minimally invasive and percutaneous interventions, the world of trauma care is dramatically different today than just a few years ago. There are multiple imaging and treatment protocols for clinicians to follow, but we need to highlight that every pediatric patient is unique, owing to the mechanism of injury or their characteristics. The ability to manage injuries relies on the surgeon’s comfort with pediatric protocols and experience with nonoperative management (NOM)(9).
In the emergency department (ED), after the evaluation of trauma patients, one should make a detailed physical exam that sometimes remains a challenge due to a poor description of symptoms and mostly the absence of physical examination findings that cannot exclude any kind of intraabdominal injury. The most commonly used imaging tools in children with blunt abdominal injuries are ultrasonography (US) and computed tomography (CT) – the gold standard in the diagnosis and therapeutical planning and also in the follow-up for cases with NOM(10).
Mostly, in pediatric surgery practice, blunt abdominal traumas are managed nonoperatively and defined as the choice, made after a primary and secondary revision, of not performing surgery immediately after imagistic and blood tests results. A surgeon must be available in case of a patient who becomes unstable, despite maximal resuscitation efforts, and requires surgical intervention. Surgery is traditionally preformed via laparotomy, but more common nowadays via laparoscopy(11-13).
The objective of this study was to investigate patients presented to our emergency department during one calendar year, with blunt abdominal traumas, by reviewing their characteristics, the degree of intraabdominal solid organs injuries (according to biological and imaging findings), and the association with the NOM or the operative management (OM).
Materials and method
A retrospective, observational study was performed to investigate the management of pediatric blunt abdominal trauma in the “Sf. Maria” Emergency Clinical Hospital for Children, Iaşi, Romania, in patients registered in our emergency service in 2014. Children under 18 years of age were considered cases of pediatric trauma.
The medical records of the patients admitted to the pediatric surgery service with potential abdominal injuries were analyzed. We included in this study patients and trauma characteristics such as age, gender, demographics, localization of trauma, type of trauma (i.e., blunt or penetrating), mechanism, and period of trauma. The physical examination was rigorously performed. The imagistic results were obtained by performing US and/or CT of the abdomen. Abdominal CT was performed on multiple trauma patients with pathologic findings on physical and US. Diagnostic workup, treatment (number and percentage of conservative treatment and need or indication of immediate surgery, intraoperative findings), and outcomes were retrieved from the database.
The patients were separated into two groups and categorized by the type of treatment they initially received. The first group of patients was treated by NOM and those who received OM were included in the second group. The operative reports were reviewed for details regarding the type and extension of the trauma, additional to the information previously obtained from clinical and imaging exams and from lab findings. The outcome measurements of this study included postoperative abdominal complications, length of hospital stay (LOS), length of intensive care unit (ICU) stay, reintervention for abdominal complications, and mortality.
In the quantitative variables, measures of central tendency and dispersion were calculated – (n) and relative frequencies (%) were calculated for qualitative variables, along with percentage for all data. The process and storage of data are following privacy and ethics regulations under the institutional medical ethics committee.
Results
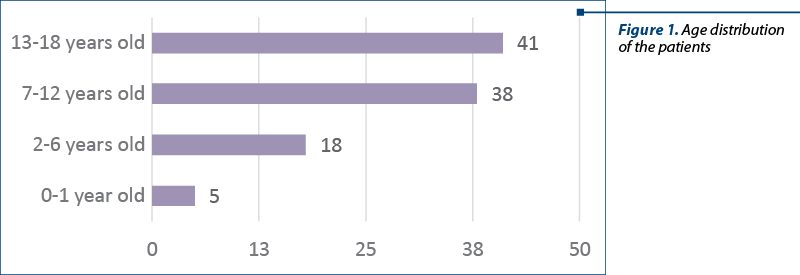
Demographics. The total number of patients included in the study groups was 102. There were 42 females (41%) and 60 males (59%), with an average age of 8.3±3.2 years old (from 6 months old to 17 years old). The distribution of cases by group age was analyzed according to the age range: 50 abdominal traumas were encountered in the range 0-10 years old, and 52 cases in the age range 11-18 years old. Thus, the predominance of abdominal traumas is observed in the age range 11-18 years old, with a percentage of 51%, and in the case of the age range 0-10 years old, a percentage of 49% was recorded. Considering the distribution of patients according to the development groups, it can be observed that: five cases were registered in the interval 0-1 year old (infants), 18 cases were registered in preschool children (2-6 years old); in the case of school-age children (7-12 years old) there were 38 cases, and 41 children (13-18 years old) were registered in adolescents (Figure 1). We found a higher preponderance of abdominal injuries among people from rural areas (n=73; 72%) compared to those from urban areas (n=29; 28%).
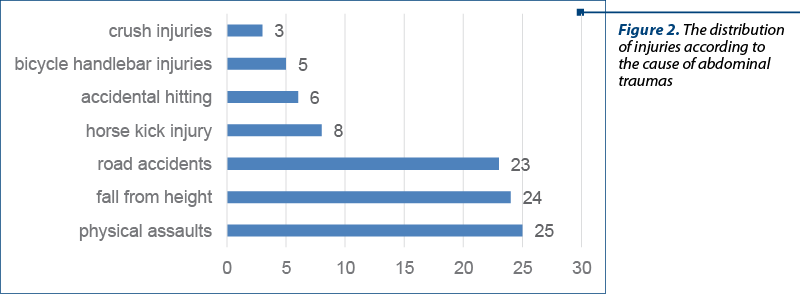
Trauma characteristics. The distribution of injuries according to the cause of abdominal traumas was registered as follows: 25 physical assaults; 24 children who fell from height altitude; 13 road accidents as pedestrians, six as passengers and four bicycle accidents; eight injuries from horse kick injury; six due to accidental hitting; five caused by hitting the handlebars of the bicycle; three children presented crush injuries. The most common cause of trauma was physical assault (24.5%), the second was falling from a height (23.5%), and the third trauma mechanisms in this series were accidents (22.5%) as car accidents, vehicle occupants or bicycle. Some of the patients had more than one lesion, 8% of patients had fractures in addition to abdominal trauma, 56% had chest trauma and 36% of patients had a head injury. In our series, there was no penetrating trauma reported. Analyzing the distribution of cases and taking into account the seasons, we can see the increased incidence of abdominal trauma in summer (36 cases; 35%), in autumn 33 cases were reported (32%), in the spring there were 21 cases (21%), and in winter there were 12 abdominal injuries (12%). Regarding the distribution of the cases according to the months of the year, it was found that most injuries were in June (n=16), followed by July (n=14), and the lower frequency was identified in December, with only one case registered. According to the days of the week, it can be noticed that most abdominal traumas were registered on Friday (n=20; 19%), followed by Wednesday (n=19; 18%) and Tuesday (n=12; 12%); on Thursday, there were nine abdominal injuries (9%). Analyzing the data related to the time when trauma occurred, we can notice the net predominance of trauma during the week, with a percentage of 73%, while during the weekends there were 28 abdominal traumas (27%).
Imaging results. The radiological examination was the most frequently used in the diagnosis of abdominal trauma. The radiological investigation methods were based on clinical criteria, the risks of the chosen method being irradiation. Referring to the imaging investigations that were performed, 94 of the patients benefited from US (fluid being identified in 80% of cases), representing 92%. Twenty-seven of those patients needed CT, representing 26.5%, and 64 of the patients had an X-ray, representing 62.7%. There were 29% of patients diagnosed with a liver trauma, 37% had a renal one, 11% had a splenic trauma, and 11% had a pancreatic trauma. Small bowel injury was diagnosed in 4% of patients, gallbladder in 4% of patients, and stomach injury in 4%.
Lab results. Pathological values in biochemical tests were observed in a certain percentage of patients, as follows: Hb determined in all patients, with pathological values recorded in only 26% of patients; in 23% of patients there were changes in Hct values. Abnormal amylase values were recorded in 11% of patients, and abnormal urine amylase values were observed in 4% of patients; abnormal AST values were identified in only 16% of patients and abnormal ALT values were identified in 14% of patients; ESR and fibrinogen values were abnormal in 2% of patients; hematuria was observed in 2% of patients and urea showed pathological values in 1% of patients.
Diagnostic workup and management. Regarding the treatment, it can be seen that 90 of the patients received conservative treatment, with a percentage of 88%, and 12 patients required surgery (12%). Other treatments, such as plaster, splints, suture and dressing, were applied to the NOM group. Ninety-four of the patients did not need a transfusion (92%), and eight patients benefited from blood transfusions, with a percentage of 8%. Among the eight patients, there were: four patients who required surgery for associated fractures; one patient diagnosed with splenic rupture, who required transfusion of 200 ml of blood and 200 ml of frozen plasma; one patient diagnosed with pancreatic rupture (caudal fragment) who required transfusion of 250 ml of blood; one patient diagnosed with hemopneumothorax, abdominal trauma, following a horse’s kick, who required transfusion of 250 ml of blood and 200 ml of frozen plasma, and another patient diagnosed with hemoperitoneum, traumatic pneumothorax, secondary to a fall from a height of about 8 m, who required the transfusion of 150 ml of blood.
Analyzing the data according to the number of hospitalization days, 51 patients had a hospitalization under five days (50%), 40 children had a hospitalization between 5 and 10 days (39%), and 11 of the patients had a hospitalization that exceeded 10 days, with a percentage of 11%. The mean hospital length of stay was 9.3 days. Examining the data according to the need for hospitalizations in the intensive care unit, we observed that 17 patients were hospitalized in ICU (17%), and the remaining 85 patients were hospitalized in the surgery department, with a percentage of 83%. Regarding the need for days of hospitalization in the ICU per patient, it can be noticed that eight patients (47%) had hospitalizations under four days, four patients (24%) needed hospitalizations between four and six days, and five patients (29%), over seven days.
Surgical treatment (OM). The operative management was needed in 12 patients. We mention:
-
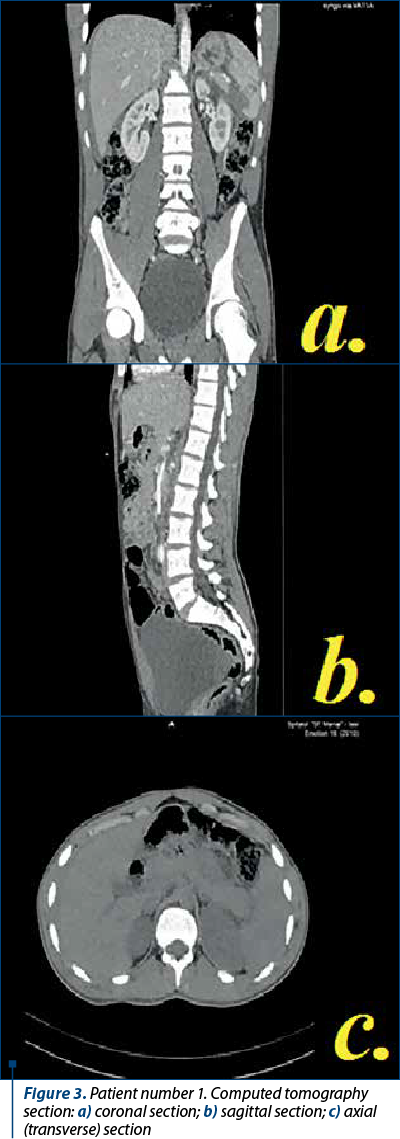
Patient number 1, diagnosed with splenic rupture, following a physical assault. CT scan results: splenic fracture grade III and hemoperitoneum (Figure 3). Because there were signs of hemodynamic instability, he required laparotomy, splenorrhaphy, hemostasis, abdominal lavage, and drainage with one tube.
-
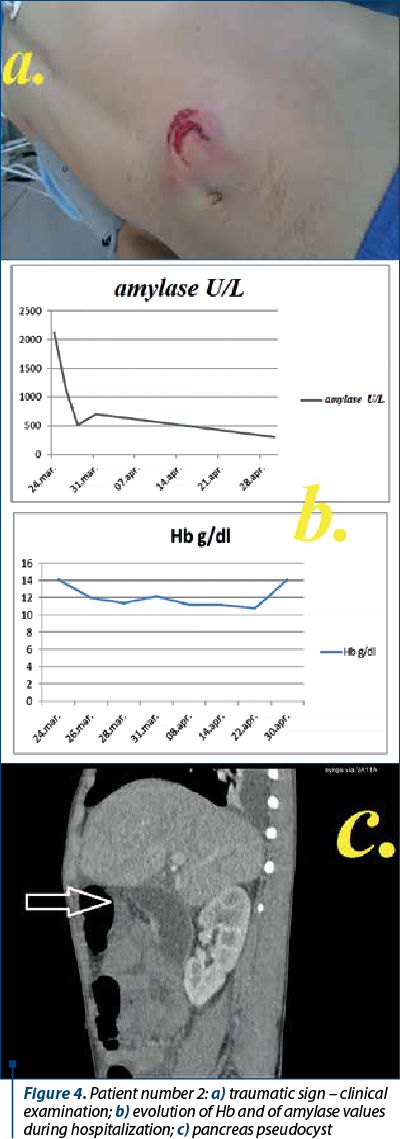
Patient number 2, diagnosed with pancreatic rupture (caudal segment), following a bicycle handlebar impact. Initially treated conservatively, the patient developed five weeks later a pseudocyst (8.16/11.6/14 cm). For the treatment of the pseudocyst, surgery was performed: a laparotomy was done, cystogastrostomy, abdominal lavage and drainage with one tube (Figure 4).
-
Patient number 3, diagnosed with an abdominal trauma, following a horse’s hoof kick in which the CT examination revealed the presence of a right hydropneumothorax, associating signs of hemodynamic instability. An emergency procedure was needed: pleural drainage in VIII intercostal right space.
-
Patient number 4, diagnosed with an abdominal trauma, following a horse’s hoof kick, initially treated conservatively, with dynamic ultrasound monitoring showing an increase peritoneal fluid and exacerbation of abdominal pain syndrome. An exploratory laparoscopy was performed and the presence of blood in the peritoneal cavity was confirmed (300 ml of old blood was evacuated), without any other lesions of the parenchymal organs. Peritoneal lavage was performed and a continuity solution was identified, involving the parietal peritoneum, the transverse aponeurosis and partially the parietal muscular body, at the level of the right flank. A postoperative abdominal drainage tube was placed.
-
Patient number 5, diagnosed with hemopneumothorax following a fall from a height of approximately 8 m, for which surgery was performed in emergency because he showed signs of hemodynamic instability. A drainage tube was placed in VII intercostal left space, with blood removal.
-
Patient number 6, diagnosed with an abdominal trauma, following a direct impact to the handlebars of the bicycle. He required surgery because he showed signs of peritonitis and free gas was revealed by X-ray. A laparotomy was performed and an intestinal perforation was identified. Resection of the perforation edge, suture of jejunal loop perforation, peritoneal lavage and drainage with two tubes were performed.
-
Patients number 7-12 required surgeries for the treatment of associated injuries – wounds, fractures.
Discussion
The evaluation and management of pediatric abdominal trauma have changed significantly in the last decades. In our study, 88% of patients with intraabdominal injuries were treated with conservative methods and 12% of them required surgery. It was reported that the liver is the second most commonly injured organ, following the spleen in blunt traumas. Wisner et al. investigated a total of 605 children with solid organ injuries and found spleen injury in 49% of these children, liver injury in 47%, and renal injury in 24% of these patients(5). Our study found that the most commonly injured organ was the kidney, in 37% of patients, followed by the liver in 29% of cases, and pancreatic or spleen trauma in 11% of patients. When compared with other studies, the results are different, as in our series renal trauma was the most common. In our study, 88% of patients with intraabdominal solid organ injuries were treated with conservative methods and 12% of them needed surgery. These rates are compatible with those from literature(14).
Basaran et al. investigated the characteristics and the degree of intraabdominal solid organ injuries in a study where 1066 pediatric patients were included, with 92.8% blunt injuries, from which liver injury was detected in 47% of patients, spleen injury in 36% and renal injury in 17% of patients. Grade II injury was the most common and 96.5% of patients were provided conservative treatment, while only 3.5% of patients were treated surgically(15).
In our study, posttraumatic pancreatic rupture was treated conservatively, because at the initial examination the patient was stable, the dynamic evolution of amylase values was favorable, the initial increase being followed by a decrease (indicating a minor pancreatic lesion), and the imaging examinations did not detect the presence of free fluid in the peritoneal cavity. The evolution under conservative treatment was favorable. After five weeks of conservative supportive treatment and protective therapy with antibiotics in the ICU department, a CT revealed a pseudocyst. For the treatment of the pancreatic pseudocyst (with dimensions exceeding 6 cm) surgery was performed, consisting in a transgastric drainage of the cyst, with a favorable outcome. The incidence of pancreatic lesions in children with nonpenetrating abdominal trauma varies between 3% and 12%. A report from San Diego revealed 18 cases of major pancreatic injury over a 14-year period. Of these 18 patients, seven were diagnosed with pancreatic pseudocyst, and in 11 patients a distal pancreatectomy was performed. Two of the seven pseudocysts were treated conservatively and five were treated by cystogastrostomy. Thus, distal pancreatic lesions must be treated by distal pancreatectomy, proximal lesions require conservative treatment, and pseudocysts may be treated conservatively or require cystogastrostomy. Endoscopic retrograde cholangiopancreatography (ERCP) with a stent placement management has been shown to be also effective. It has been found that CT examination is suggestive, but the diagnosis cannot always be made based on this examination(16). The mortality associated with pancreatic trauma varies between 8% and 10% in children and is usually due to associated lesions, especially vascular ones with hemorrhages or neurological lesions and multiple organ failure(17).
In our study, we had a 15-year-old male patient who was hospitalized in our surgery department for supervision, following a bicycle accident. At admission, the patient had a good general condition, stable and at local exam he presented multiple superficial wounds in the left lumbar and hypochondrium, spontaneous pain and at palpation in the left hemiabdomen, and also microscopic hematuria. The imaging test in ER (chest X-ray and ultrasonography) showed no changes. At approximately 48 hours after the admission, his general status showed signs of impairment, with a progressive increase in pain in the left hypochondrium and the suspicion of splenic rupture was raised, a reason for which abdominal CT was performed. The study revealed posttraumatic splenic lacerations, grade III AAST, posterior arch fracture – left C9 rib, left pleural fluid in small amounts, bilateral posterobasal lung lesion. The patient’s general good condition and the laboratory results permitted the management by conservative treatment. The outcome was favorable.
The conservative treatment in isolated spleen and liver ruptures in stable children is a universal standard management implemented for about three decades worldwide, with favorable outcomes. It involves bed rest, supportive treatment and blood transfusion, if needed.
The course of a spleen rupture can be variable. Apart from the obvious cases with operative indication, there are smaller spleen ruptures which may evolve over time with small signs of internal bleeding or which, after surveillance for several days, are suddenly manifested with signs of a delayed severe hemorrhage. This possibility of evolution must be taken into account and it is necessary to recommend a minimum safety interval of time until the resumption of daily activities. If the supportive treatment fails and surgery is performed, the purpose of the intervention is to control bleeding and preserve the splenic tissue. Laparotomy is performed and, depending on the degree of the lesions, splenic suturing can be applied, using hemostatic agents, partial splenectomy or total splenectomy.
In case of splenic lesions, conservative treatment is preferred more frequently recently compared to surgery. The conservative treatment will apply to cases where the estimated blood loss is less than 500 ml or one-third of the child’s blood volume, the lesions associated are minimal, without interesting the hilum, and with normal hemostasis(18).
In research performed by Bairdain et al., on patients diagnosed with splenic lesions, admitted to the Boston Hospital between 1994 and 2014, it was concluded that no patient diagnosed with splenic lesions had died or had a splenectomy in the last 20 years. The length of hospitalization decreased over time, despite the increase in the severity of splenic lesions(19).
In the literature, the surgical treatment percentages are reported at 8-31% and the conservative treatment percentages are reported at 70-92%(14,20,21). More commonly in recent studies, the surgery ratio is low. In the study of Henderson et al., the prevalence of surgery was reported at 8.7%(14). In the study of Rogers et al., 10% of patients with a high-grade injury (grade IV) were surgically treated and 80% of them were conservatively managed(22). In our study, 90 children with different traumas (88%) were observed and the conservative treatment was applied, and only in 12 children (12%) a surgical approach was applied.
In conclusion, solid organ injuries due to pediatric abdominal blunt trauma are generally severe injuries, with high morbidity and mortality. Nowadays, more than 90% of pediatric solid organ injuries are successfully treated with conservative methods.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
-
Gaines BA. Intra-abdominal Solid Organ Injury in Children: Diagnosis and Treatment. The Journal of Trauma. 2009;67:S135-S139.
-
Holmes JF, Mao A, Awasthi S, McGahan JP, Wisner DH, Kuppermann N. Validation of a prediction rule for the identification of children with intra-abdominal injuries after blunt torso trauma. Ann Emer Med. 2009 Oct;54(4):528e533.
-
Gaines BA, Rutkoski JD. The role of laparoscopy in pediatric trauma. Semin Pediatr Surg. 2010;19:300e303.
-
NationalVital Statistics System, NationalCenter forHealth Statistics (CDC). 10 Leading causes of death by age group, Unites States – 2014. Available at: http://www.cdc.gov/injury/wisqars/pdf/leading_causes_of_death_by_age_group_2014-a.pdf.
-
Notrica DM. Pediatric blunt solid organ injury: beyond the APSA guidelines. Curr Surg Rep. 2015;3:1-6.
-
Wegner S, Colletti JE, Van Wie D. Pediatric Blunt Abdominal Trauma. Pediatr Clin N Am. 2006;243-56.
-
Wisner DH, Kuppermann N, Cooper A, Menaker J, Ehrlich P, Kooistra J, et al. Management of children with solid organ injuries after blunt torso trauma.
-
J Trauma Acute Care Surg. 2015;79(2):206-14.
-
Pariset J, Feldman, K, Pari C. The Pace of Signs and Symptoms of Blunt Abdominal Trauma to Children. Clinical Pediatrics. 2010;49(1):24-8.
-
Drexel S, Azarow K, Jafri MA. Abdominal Trauma Evaluation for the Pediatric Surgeon. Surg Clin N Am. 2017;97(1):59-74.
-
Houda II WE. Pediatric Trauma. In: Tintinalli JE, Stapczynski JS, Cline DM, Ma OJ, Cydulka RK, Meckler GD (eds): Emergency Medicine A Comprehensive Study Guide. 7th ed. New York: The Mac Graw Hill Companies, 2010.
-
Morales C, Correa J, Villegas M. Efficacy and safety of non-operative management of blunt liver trauma. Eur J Trauma Emerg Surg. 2011;37(6):591-6.
-
Cherkasov M, Sitnikov V, Sarkisyan B, Degtirev O, Turbin M, Yakuba A. Laparoscopy versus laparotomy in management of abdominal trauma. Surg Endosc. 2008;22:228e231.
-
Mandrioli M, Inaba K, Piccinini A, et al. Advances in laparoscopy for acute care surgery and trauma. World J Gastroenterol. 2016;22:668e680.
-
Sanchez JI, Chaidas CN. Childhood trauma: now and in the new millennium. The Surg Clin North Am. 1999 Dec;79(6):1503-35.
-
Basaran A, Ozkan S. Evaluation of intra-abdominal solid organ injuries in children. Acta Biomed. 2019 Jan 15;89(4):505-512.
-
Wesson DE, Cooper A. Pediatric Trauma Pathophysiology, Diagnosis and Treatment, Taylor and Francis Group, 2006.
-
George W. Holcomb, Aschcraft’s pediatric surgery fifth edition, Saunders Elsevier, 2010.
-
Lippert SJ, Hartin CW, Ozgediz DE, et al. Splenic conservation: variation between pediatric and adult trauma centers. J Surg Res. 2013;182(1):17-20.
-
Bardain S. Twenty-years of splenic preservation at a level 1 pediatric trauma center. J Pediatr Surg. 2015 May;50(5):864-8.
-
Balcioglu ME, Boleken ME, Cevik M, Savas M, Boyacı FN. Blunt renal trauma in children: a retrospective analysis of 41 cases. Ulus Travma Acil Cerrahi Derg. 2014;20(2):132-5.
-
Sahin H, Akay AF, Yılmaz G, Tacyıldız IH, Bircan MK. Retrospective analysis of 135 renal trauma cases. Int J Urol. 2004 May;11(5):332-6.
-
Rogers CG, Knight V, MacUra KJ, Ziegfeld S, Paidas CN, Mathews RI. High-grade renal injuries in children is conservative management possible? Urology. 2004 Sep;64(3):574-9.




