Congenital diaphragmatic hernia (CDH) is a condition consisting in a defect at the level of the diaphragm that leads to migration of the abdominal viscera into the thoracic cavity, event that generates many complications during intrauterine development, the most severe being represented by hypoplasia of lungs and persistent pulmonary hypertension of the neonate. CDH may appear as an isolated condition or it may be an integrated part of a syndrome. Findings in literature so far suggest that the incidence ranges from 1 in 2000 to 1 in 3000 newborns. In spite of the advance made in both medical and surgical management of this disease, morbidity and mortality remain high. This article presents a rare case of an isolated congenital right diaphragmatic hernia in a born at term patient.
Hernie congenitală diafragmatică pe partea dreaptă - prezentare de caz
Right-sided congenital diaphragmatic hernia - case report
First published: 30 octombrie 2017
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Peri.1.3.2017.1175
Abstract
Rezumat
Hernia diafragmatică congenitală este o patologie ce constă în existenţa unui defect la nivelul diafragmului abdominal, din pricina căruia are loc migrarea viscerelor abdominale în cavitatea toracică. Acest fenomen determină apariţia în lanţ a unor multiple complicaţii în timpul dezvoltării intrauterine, cea mai severă dintre ele constând în hipoplazia pulmonară şi instalarea hipertensiunii pulmonare persistente a nou-născutului. Hernia diafragmatică congenitală poate fi diagnosticată ca entitate de sine stătătoare sau în cadrul unui sindrom. Până în prezent, datele din literatura de specialitate indică o incidenţă a acestei patologii între 1 la 2000 şi 1 la 3000 de nou-născuţi. Cu toate că managementul bolii, atât cel de natură medicală, cât şi cel de natură chirurgicală, a fost considerabil îmbunătăţit, ratele morbidităţii şi mortalităţii rămân ridicate. Acest articol prezintă un caz rar de hernie diafragmatică dreaptă diagnosticată la un nou-născut la termen.
Background
Congenital diaphragmatic hernia (CDH) is characterized by the displacement of the abdominal organs into the thorax, due to an abnormal development of the diaphragm. The diaphragm is a muscular fibrous tissue that lies between the thorax and the abdomen, separating them into two different cavities. Normally, the formation of diaphragm begins around the 3rd-4th week of gestation and is completed by weeks 8-12(1,2). The incomplete or abnormal development of the pleuroperitoneal folds and pathologic muscle migration lead to different congenital defects(1).The most common type of hernias occur at the posterior-lateral region of the diaphragm (70-75%), also called Bochdaleck hernias, with a significantly higher occurrence on the left side (85%) comparing to the hernias occurring on the right side (13%) or bilateral (2%). Anterior congenital defects are named Morgagni hernias and are met in 23-28% of the cases and occur at the diaphragmatic sternocostal hiatus, most of them (90%) being diagnosed on the right side. A much smaller percentage (2-7%) is represented by central or hiatal hernias(1,2). In left-sided hernias, the small and large bowel, along with the solid intraabodminal organs herniate into the thorax whereas the right-sided hernias allow the herniation of liver and a small segment of the large bowel. Bilateral hernia is even more uncommon and has a fatal prognostic(3).
Neonates with CDH commonly present with respiratory distress (cyanosis, retractions, grunting respiration) within the first 24 hours, but in some cases, late occurrence of the symptoms has been seen. If the respiratory distress is severe, circulatory insufficiency can be associated(3,4). Lung hypoplasia or lung immaturity occur on the same side with the hernia. Even though initially it was believed that hypoplasia occurs secondary to a physical compression of the lung by the abdominal viscera, rat model studies suggested that the process begins in the phase of organogenesis, resulting in bilateral hypoplasia followed by constriction of the ipsilateral lung by the abdominal viscera later in intrauterine development(2,4).
In early diagnosis, physical examination reveals right-sided heart (left hernia), decreased breath sounds on the affected lung, scaphoid abdomen, intestinal sounds in the thorax, respiratory distress. CDH can be diagnosed in utero with ultrasonography that often shows the presence of polyhydramnios, or by MRI to assess the visceral malformation. Late diagnosis is determined by the existence of a chest mass on the radiologic exams, gastric volvulus, splenic volvulus or bowel obstruction(1). Other findings in CDH relate to other complications of this condition such as gastric volvulus, hypoplasia of the left ventricle in left-sided hernias or pleural effusion in right-sided hernias and bilateral renal hypertrophy(5).
Although great advances have been made in the management of CDH, morbidity and mortality still remain at high rates(6). In left-sided hernias, most of the morbidity and mortality is related to the pulmonary hypoplasia and subsequent persistent pulmonary hypertension. In right-sided hernias, liver herniation is associated with worse prognosis. Some studies reported 100% survival of neonates without liver herniation, compared to 56% survival of infants with herniated liver(1,2). According to literature, overall mortality after live-birth ranges from 40% to 62% and the presence of associated anomalies significantly decreased survival.

Case report
We present the case of male patient, born at term (37-38 weeks) by vaginal delivery, with no difficulties during extraction, weighting 3150 g, with Apgar score 8/10, with opalescent aminotic fluid, reanimated at birth, with oxygen supply and peripheral stimuli.The mother was 23-years-old and she did not make any prenatal care until week 22 of pregnancy. After being taken into observation, a proper ultrasound monitoring was performed, but none of them revealed any anomaly. Written consent of both parents was signed to allow the authors publish this article.
The physical examination at birth revealed neonatal jaundice and right testicle absent from scrotum. Immediately after delivery, acute respiratory distress occured, with a discreet moan during expiration, subcostal retraction and 60-80/minute respiratory rate (RR). The neonate was taken into the incubator and continuous oxygen was administered.
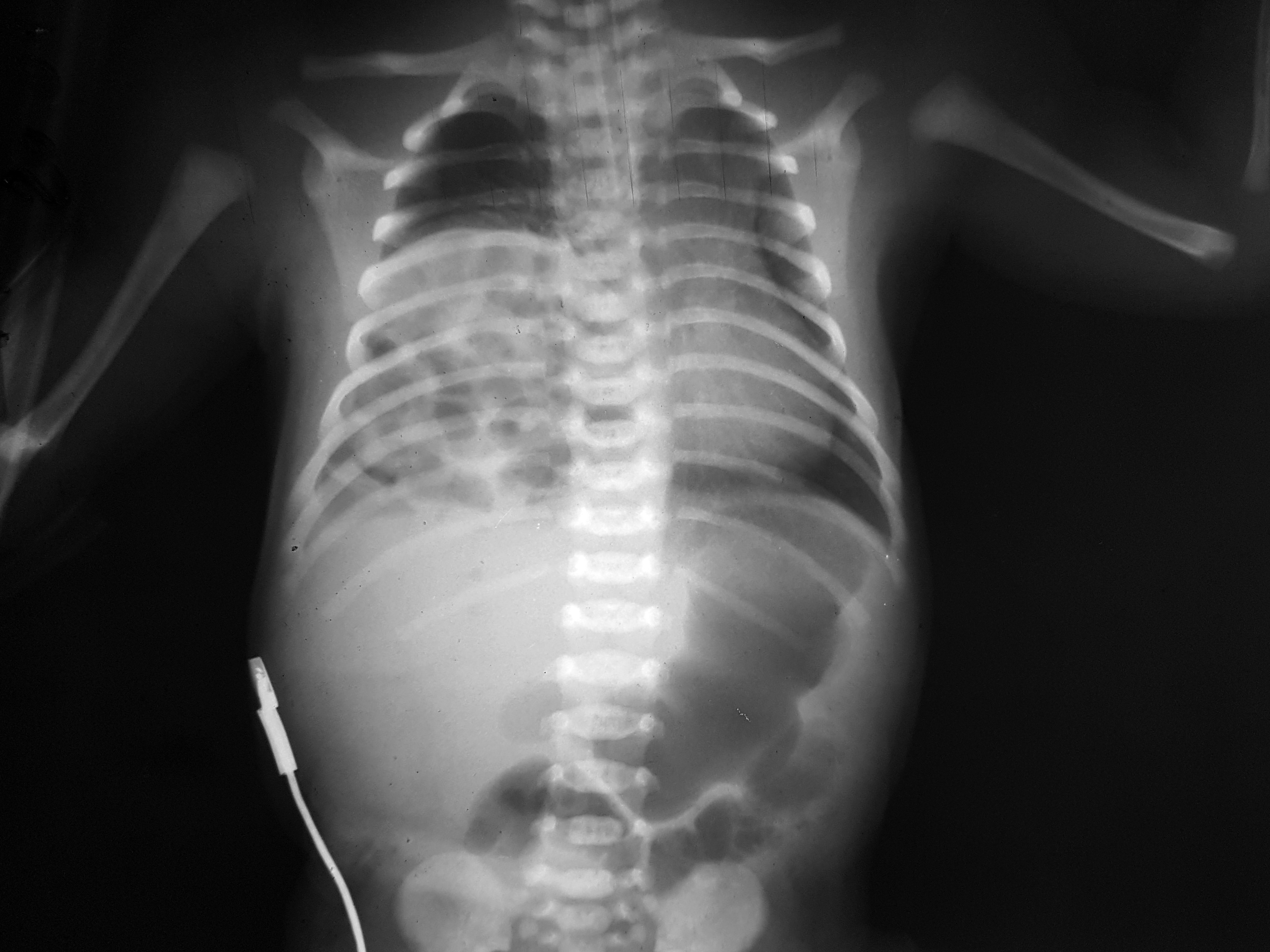
At 2 hours postpartum the acute respiratory distress is more severe, with RR of 80/min, continuous oxygen supply with vital signs monitoring. A chest radiograph was performed and was highly suggestive for right diaphragmatic hernia (Figure 1). The infant was transferred to the Intensive Care Unit were was intubated, and the combined antibiotherapy was started, with intravenous dopamine being administered for hemodynamic support. The next hours, the general condition is maintained stable with blood oxygen level at 100%. After 48 hours, postpartum respiratory and metabolic acidosis occur, and at 72 hours clinical examination reveals acrocyanosis and blood tests show leukopenia and thrombocytopenia. The suspicion of bacterial sepsis with unknown pathogen is risen and previous antibiotherapy is changed with a more aggressive one.
After 72 hours with persistent mechanical ventilation, the neonate is transferred to a different hospital in order to provide surgical care. The ecocardiography showed a persistent foramen ovale, but no other cardiac malformation. Intraoperatory, beside bowel, the left hepatic lobe was partially migrated into the thorax along with right kidney and right adrenal gland.
Postoperatory, the evolution was favorable, enteral nutrition was started 10 days after surgery and the infant was extubated after 30 days. A CT scan was performed at 7 days postoperatory and showed normal position of right diaphragm, with diffuse pulmonary hyperinflation with no abnormal airway position and branching. The bronchoscopy performed at 21 days postoperative reveals small caliber abnormalities of the segmental bronchi at the right inferior lobe. Usually, the survival without a long-term or permanent morbidity is considered as good outcome(7).
Discussions
Congenital diaphragmatic hernia occur in almost 2 out of 3 cases on the left side, with no differences between males and females(1). We presented a rare case of a neonate diagnosed with right-sided hernia at two hours postpartum, when the acute respiratory distress occur and chest X-ray was performed. It is important to say that the clinical importance overtakes X-rays in case of no diagnosis and no prenatal care(8).The presentation is similar to left-sided CDH, but prior to birth left sided hernias are more easly diagnosed than right-sided hernias.
In the prenatal period, the ultrasonography is highly sensitive in the detection of CDH, showing polyhydramnios, intrathoracic stomach bubble, mediastinal and cardiac shift, and the visualisation of abdominal organs in the thoracic cavity. In right-sided hernia, the right lobe may be herniated or associated with ascites and hydrothorax(5). In our case, the left lobe of the liver was herniated and there was no pathological fluid present in the thorax.
A study from 2016 performed on 3665 patients suggested that infants diagnosed with CDH were commonly discharged with at least one major comorbidity(9).
In the case we presented the infant had isolated right-sided hernia with no other congenital malformation observed with the help of abdominal ultrasound, chest radiograph, CT scan and echocardiography.
Although usually neonates with CDH have pulmonary hypoplasia, the only alteration assessed by bronchoscopy was mild reduction in caliber of the segmental bronchi in the right inferior pulmonary lobe.
There is stated in literature that 10% of infants with CDH associate other abnormalities, in an underlying syndromic diagnosis such as Cornelia de Lange syndrome or Fryns syndrome. Chromosome abnormalities were found in almost 30% of infants with CDH, the condition being described as part of trisomy 13, trisomy 18, trisomy 21 and Turner syndrome(4). In our case, karyotype findings did not reveal any alteration of genes.
Regarding treatment, there is controverse whether to perform fetal surgery or to delay the intervention, as there are some reports of increases in mortality rates with early surgical intervention(1). In our case, the patient was first stabilized and only after 72 hours was transferred to a surgical care unit, with good postoperative evolution and excellent outcome with no persistent respiratory distress.
Another issue is that the main challenge is when liver is herniated into the thorax and during reduction, the blood flow through the umbilical vein and inferior cava may become occluded leading to death of the fetus(6), a complication that did not occur periprocedural in our patient. The possible explanation might be that our patient had his left lobe instead of right lobe partially herniated, so blood flow in umbilical vein was conserved.
Although infants with CDH and liver herniation have a worse prognosis than ones without liver herniation(2), our patient did not encounter any complications related to that. A population-based study in Australia stated that 71% of the pregnancies with prenatal CDH diagnosed were terminated because of the existence of another major anomaly(3).
In our case, the mother did not present to the doctor until the 22nd week of pregnancy but even after ultrasonography the monitoring did not reveal any anomaly. Maybe it was for the benefit of the infant that the condition was not discovered antepartum regarding that there is an ongoing ethical controversy between maternal versus fetal rights(7).
Bibliografie
2. Praveen Kumar Chandrasekharan, Munmun Rawat, Rajeshwari Madappa, David H. Rothstein, and Satyan Lakshminrusimha. Congenital Diaphragmatic hernia – a review. Mar 11, 2017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5356475/
3. Robin H Steinhorn. Pediatric Congenital Diaphragmatic Hernia. Apr 25, 2014. http://emedicine.medscape.com/article/978118-overview#a8
4. Holly L Hedrick, N Scott Adzick. Congenital diaphragmatic hernia in the neonate. Jul 25, 2017. https://www.uptodate.com/contents/congenital-diaphragmatic-hernia-in-the-neonate#H3
5. Ali Hekmatnia. Congenital Diaphragmatic Hernia Imaging. Nov 25, 2016. http://emedicine.medscape.com/article/407519-overview#a5
6. Doug N Miniati. Fetal Surgery for Congenital Diaphragmatic Hernia. Jan 03, 2017. http://emedicine.medscape.com/article/2109500-overview
7. Bhatnagar SN, Sarin YK. Management of Congenital Diaphragmatic Hernia in Newborn - Paradigm Shift and Ethical Issues. Jun 16, 2017. https://www.ncbi.nlm.nih.gov/pubmed/28620733
8. Jamile Rizzardi Lava, Guilherme A Hettwer, Cleiton Jonei Reginatto, Guilherme Galoro, Carolina T Gehlen, Maria CM Subtil, Vitor E Valenti, Luiz Carlos de Abreu, Carlos Bandeira de Mello Monteiro, and Márcio Petenusso. Congenital diaphragmatic Bochdaleck hernia: case report. Oct 30, 2012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549796/
9. Putnam LR, Harting MT, Tsao K, Morini F, Yoder BA, Luco M, Lally PA, Lally KP. Congenital Diaphragmatic Hernia Study Group. Congenital Diaphragmatic Hernia Defect Size and Infant Morbidity at Discharge. Nov 2016. https://www.ncbi.nlm.nih.gov/pubmed/27940787
Articole din ediţiile anterioare
Sindromul Prader-Willi - prezentare de caz şi revizuirea literaturii
Sindromul Prader-Willi este consecinţa mai multor defecte genetice în regiunea 15q11-q13, între care şi modificările de metilare, şi este asociat l...
Artrogripoza la un nou-născut prematur provenit din sarcină gemelară. Prezentare de caz
Artrogripoza congenitală multiplă (AMC) este caracterizată în literatura de specialitate de multiple contracturi articulare congenitale la nou-născ...
Agenezia renală unilaterală – prezentare de caz
Agenezia renală unilaterală se caracterizează prin absenţa parenchimului renal, care apare în urma erorilor din cursul organogenezei, şi are o inci...
Infecţia herpetică neonatală – review
Autorii trec în revistă epidemiologia, etiologia, incidenţa, tabloul clinic, diagnosticul şi diagnosticul diferenţial al infecţiilor herpetice neon...