Importanţa crucială a diagnosticului diferenţial al greţei şi vărsăturilor în sarcină. Propunere a unui ghid de diagnostic şi management
The critical importance of the differential diagnosis of nausea and vomiting in pregnancy. Proposal of a diagnostic and management guide
Abstract
Nausea, with or without vomiting with mild symptoms, is considered a normal part of the pregnancy pathophysiology. The beginning of the symptoms is the first suggestive sign regarding the basal condition. Nausea and vomiting of pregnancy normally begin to manifest before 9 weeks of gestation. If the onset exceeds this point, other causes should be mandatory investigated. By summarizing the main recommendations from the most important international committees of obstetrics and gynecology, we propose an algorithm for the management of cases of nausea and vomiting during pregnancy and hyperemesis gravidarum that could exclude all the differential diagnoses. We hope that our initiative will ease the time-efficient diagnosis of possible pathological conditions which is a crucial aspect in the successful management of any disease.Keywords
nausea and vomitingpregnancydifferential diagnosisRezumat
Greaţa, însoţită sau nu de vărsături uşoare, este considerată o componentă normală a fiziopatologiei sarcinii. Începutul simptomelor este primul semn în stabilirea diagnosticului de certitudine. Greaţa şi vărsăturile încep în mod normal să se manifeste înainte de 9 săptămâni de gestaţie. Dacă debutul depăşeşte acest punct, ar trebui investigate obligatoriu alte cauze. Prin rezumarea principalelor recomandări din partea celor mai mari societăţi internaţionale de obstetrică şi ginecologie, propunem un algoritm pentru gestionarea cazurilor de greaţă şi vărsături în timpul sarcinii şi diagnosticul diferenţial al acestora. Sperăm că iniţiativa noastră va facilita diagnosticul precoce al posibilelor condiţii patologice, care este un aspect crucial în gestionarea cu succes a oricărei boli.Cuvinte Cheie
greaţă şi vărsăturisarcinădiagnostic diferenţialIntroduction
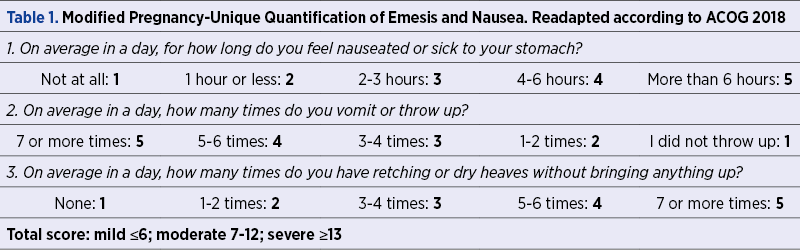
In early pregnancy, nausea, with or without vomiting with mild symptoms, is considered a normal part of the pregnancy pathophysiology. The categorization into degrees of severity implies the assessment of the amount and the duration of nausea and vomiting per day. Respectively, mild cases are characterized by a duration shorter than one hour per day and an amount of up to two times per day, and the severe cases are characterized by more than six hours of vomiting in more than five relapses per day(1). According to the American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin(2), the best quantification of the nausea and vomiting of pregnancy severity is offered by the Pregnancy-Unique Quantification of Emesis and Nausea (PUQE) score which implies also the impact on life quality, but refers strictly to the first-trimester cases. The modified Pregnancy-Unique Quantification of Emesis and Nausea score includes three questions with answers corresponding to different scores, with a final score that places the patient in a mild, moderate or severe form of the condition (Table 1).
The progression to hyperemesis gravidarum, defined as persistent vomiting not justified by other causes and objectified by important ketonuria and the loss of at least 5% of pre-pregnancy weight(3), can be prevented if the early treatment of nausea and vomiting is initiated.
Differential diagnosis
The beginning of the symptoms is the first suggestive sign regarding the basal condition. The nausea and vomiting of pregnancy will begin to manifest before 9 weeks of gestation. If the onset exceeds this point, other causes should be mandatory investigated:
-
Gastrointestinal conditions, such as gastroenteritis, gastroparesis, achalasia, biliary tract disease, hepatitis, intestinal obstruction, peptic ulcer disease, pancreatitis, appendicitis and even malignant conditions of the gastrointestinal tract. A detailed anamnesis, physical and paraclinical exam accompanied by several directed laboratory investigations could clear the diagnosis.
-
Genitourinary tract conditions like ovarian torsion or degenerating uterine leiomyoma, uremia, kidney stones or pyelonephritis.
-
Metabolic disorders such as hyperthyroidism, hyperparathyroidism, diabetic ketoacidosis, porphyria or Addison’s disease.
-
Neurologic disorders like cerebral tumors or pseudotumors, vestibular lesions, migraines or lymphocytic hypophysitis.
-
Medications related to nausea and vomiting are those for cancer chemotherapy (especially cisplatinum, nitrogen mustard and dacarbazine, with severe impact), aspirin, antigout drugs, digoxin, beta blockers and calcium channel antagonists, oral antidiabetics, antibiotics and antivirals like tetracycline, erythromycin, antituberculosis drugs or acyclovir, anticonvulsants, antiparkinsonians or antiasthmatics.
-
It is mandatory to consider pregnancy-related conditions like preeclampsia, HELLP syndrome or acute fatty liver of pregnancy, and also psychologic conditions and drug toxicity.
Hyperemesis gravidarum can cause significant maternal morbidity, such as Wernicke encephalopathy, due to the important vitamin B1 deficiency, esophageal rupture, splenic avulsion, pneumothorax or acute tubular necrosis. In addition, due to the increased hospital admission rate and the significant psychosocial impact, it increases the incidence of associated depression, anxiety and decisions for pregnancy termination(5,6).
By summarizing the main recommendations from the most important international committees of obstetrics and gynecology(7-9), we propose the following algorithm for the management of cases of nausea and vomiting during pregnancy and hyperemesis gravidarum that could exclude all the differential diagnoses. The protocol has as the main guidance points the personal and family medical history, the onset of the symptomatology and the intensity associated, the general and local clinical exam, the laboratory findings and specific paraclinical investigations.
1. Initial assessment
Consider normal if:
-
The onset is between 4 and 7 weeks of gestation.
-
There are factors favorable for hyperemesis gravidarum development – first pregnancy, hyperemesis gravidarum in previous pregnancies, obesity, multiple pregnancy, hydatidiform mole.
Consider abnormal if:
-
The onset is after 11 weeks of gestation.
-
After the specific medication was administred, no response was obtained.
-
Severe abdominal or epigastric pain present.
The medical history will guide the subsequent investigations: obstetrical history, duration of nausea/vomiting, response to the administered treatment, capability of oral intake, weight loss, urinary symptoms, abdominal pain, the characteristics of intestinal transit, thyroid disease, the distance between meals and vomiting episodes.
The physical examination includes: temperature, pulse, blood pressure, oxygen saturation, respiratory rate, abdominal examination, weight, signs of dehydration, signs of muscle wasting, goiter, periorbital edema and dry skin.
The first investigations will include a urine dipstick to quantify the ketonuria level, full blood count for indirect signs of deficits (anemia), malabsorption and dehydration and the differential diagnosis with infection.
The biochemical blood analysis will follow as a priority order and will include mandatory:
-
The specific tests for liver function, excluding this way liver pathology (hepatitis, cirrhosis, gallstones) and documenting severe malnutrition.
-
Amylase for pancreatitis exclusion.
-
Glycemia, lactate dehydrogenase (LDH), electrolytes, urea and creatinine concentration for evaluating the impact of dehydration and malnutrition.
2. For refractory cases
If the diagnosis was not clarified after the aforementioned investigations and the nausea and vomiting of pregnancy continue after 14 weeks of gestation, other pathologies should be considered. The suspicion of an endocrine pathological substrate can be clarified through analyses for hypo-/hyperthyroidism.
Also, an antibody test for Helicobacter pillory is recommended to be performed in refractory, severe cases, as the chronic infection is associated with hyperemesis gravidarum(10).
Unofficially, nausea and vomiting in the first period of pregnancy are considered a good sign for pregnancy outcome, as studies have shown than among population with hyperemesis gravidarum the incidence of miscarriage is significantly lower (3.1%) compared with the one in the general population (15%)(11). However, multiple pregnancy and gestational trophoblastic disease are conditions that increase the risk for a severe form of hyperemesis gravidarum, therefore an obstetrical ultrasound should be considered for clarifying the clinical picture and for adapting the subsequent management(12).
General abdominal ultrasound examination in patients with hyperemesis gravidarum is strongly suggested to be considered for cases with late onset, with persistence after 20 weeks of gestation or exacerbation(13), focused on liver, biliary tree and pancreas. If atypical gastrointestinal symptomatology is present, upper gastrointestinal endoscopy with specific monitoring during procedure is recommended.
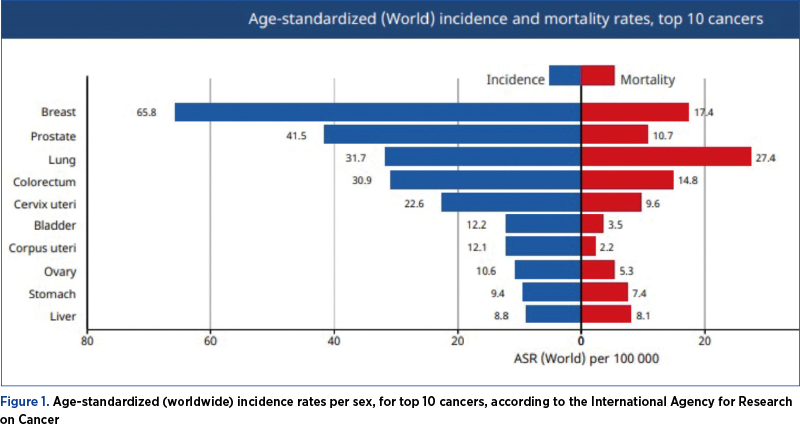
The differential diagnosis with gastric cancer should not be ignored, especially if the risk factors such as immunosuppressive disease, smoking, history of gastric ulcer and advanced age are identified(14). Even though gastric cancer during pregnancy is rare, in 2020, according to the Global Cancer Observatory, this form of cancer was included in the top 10 cancers in terms of incidence and mortality (Figure 1). Usually, when diagnosed in pregnancy, gastric cancer is in an advanced stage, with a grim prognosis for both the mother and the fetus. This diagnosis can be missed due to the similarity in clinical manifestation with hyperemesis gravidarum, thus delaying the diagnosis and the initiation of treatment.
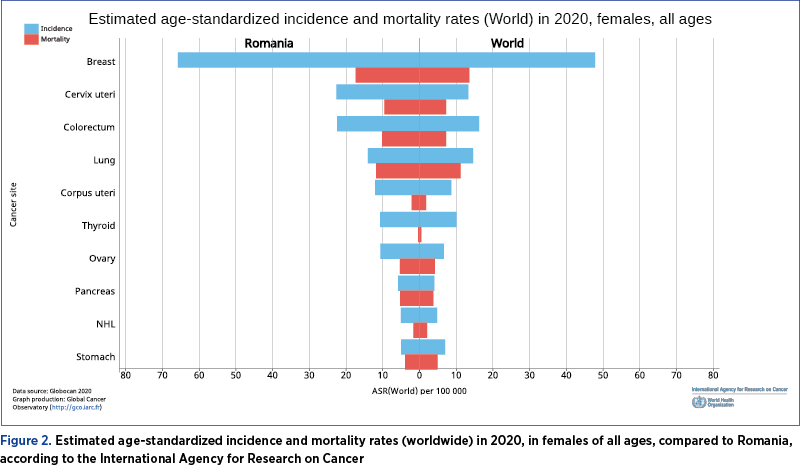
In 2020, according to the International Agency for Research on Cancer, in Romania the incidence and mortality of gastric cancer were below the corresponding values for worldwide incidence and mortality in women (Figure 2), but it should be specified the existence of some deficiencies in the registration, diagnosis and declaration of cases.
Treatment principles
The treatment with antiemetics on an outpatient basis should be offered to the patients with a PUQE score below 13 and with available primary care possibilities. The admission is recommended if nausea and vomiting are persistent, with intolerance to oral antiemetics, ketonuria and/or weight loss >5% of body weight and/or with suspected comorbidities(9).
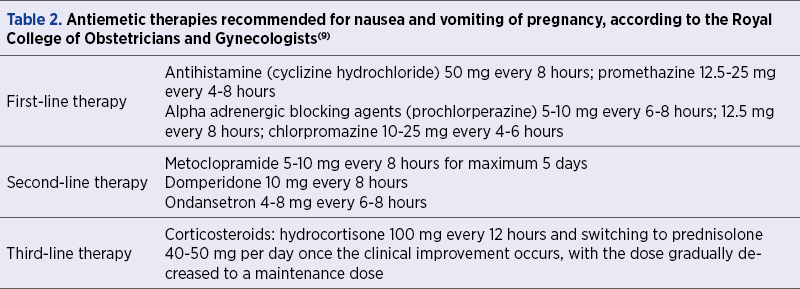
The pharmacological agents considered safe and effective in pregnancy are presented in Table 2.
Conclusions
Nausea and vomiting are considered physiological in normal pregnancy and these symptoms are usually limited to the first trimester. Although there are a small number of cases, without any associated comorbidity, in which these manifestations extend throughout the pregnancy, we consider that the investigations for excluding pathologies that can mimic this physiological state are mandatory. By summarizing the main investigations that should be considered in selected cases of nausea and vomiting of pregnancy and also the justification for considering them, we hope to ease the time-efficient diagnosis of possible pathological conditions, which is a crucial aspect in the successful management of any disease.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Attard CL, Kohli MA, Coleman S, Bradley C, Hux M, Atanackovic G, et al. The burden of illness of severe nausea and vomiting of pregnancy in the United States. Am J Obstet Gynecol. 2002;186:S220–7.
- Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 189: Nausea and Vomiting of Pregnancy. Obstet Gynecol. 2018 Jan;131(1):e15-e30.
- Goodwin TM, Montoro M, Mestman JH, Pekary AE, Hershman JM. The role of chorionic gonadotropin in transient hyperthyroidism of hyperemesis gravidarum. J Clin Endocrinol Metab. 1992;75:1333–7.
- Goodwin TM. Hyperemesis gravidarum. Obstet Gynecol Clin North Am. 2008;35:401–17, viii.
- Di Gangi S, Gizzo S, Patrelli TS, Saccardi C, D’Antona D, Nardelli GB. Wernicke’s encephalopathy complicating hyperemesis gravidarum: from the background to the present. J Matern Fetal Neonatal Med. 2012;25:1499–504.
- Mitchell-Jones N, Gallos I, Farren J, Tobias A, Bottomley C, Bourne T. Psychological morbidity associated with hyperemesis gravidarum: a systematic review and meta-analysis. BJOG. 2017;124:20–30.
- Society of Obstetricians and Gynecologists of Canada (SOGC), Clinical practice guideline on the management of nausea and vomiting of pregnancy. 2016.
- American College of Obstetricians and Gynecologists (ACOG): Practice bulletin – Nausea and vomiting of pregnancy. 2018.
- Royal College of Obstetricians and Gynecologists (RCOG): Green-top guideline for the management of nausea and vomiting of pregnancy and hyperemesis gravidarum. 2016.
- Li L, Li L, Zhou X, Xiao S, Gu H, Zhang G. Helicobacter pylori infection is associated with an increased risk of hyperemesis gravidarum: a meta-analysis. Gastroenterol Res Pract. 2015;2015:278905.
- Bashiri A, Neumann L, Maymon E, Katz M. Hyperemesis gravidarum: epidemiologic features, complications and outcome. Eur J Obstet Gynecol Reprod Biol. 1995 Dec;63(2):135-8.
- Basso O, Olsen J. Sex ratio and twinning in women with hyperemesis or preeclampsia, Epidemiology. 2001 Nov;12(6):747-9.
- Kuscu NK, Koyuncu F. Hyperemesis gravidarum: current concepts and management. Postgrad Med J. 2002 Feb;78(916):76-9.
- Maggen C, Lok CA, Cardonick E, et al. Gastric cancer during pregnancy: A report on 13 cases and review of the literature with focus on chemotherapy during pregnancy. Acta Obstet Gynecol Scand. 2020;99(1):79-88.



