Multiparametric MRI is an invaluable tool in the detection, localization and characterization of the prostate lesions, one of the most challenging situation being the one in which prostate cancer may be present in the transitional zone in a patient with benign prostatic hyperplasia. PI-RADS version 2.1 scoring system manages to standardize the radiological reports, facilitate the precise localization of the lesion, and help in the patients’ selection for targeted biopsy.
Evaluarea IRM multiparametrică în hiperplazia benignă de prostată – o adevărată provocare în excluderea cancerului de prostată
Multiparametric MRI evaluation in benign prostatic hyperplasia – a true challenge in prostate cancer exclusion
First published: 14 decembrie 2019
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/OnHe.49.4.2019.2740
Abstract
Rezumat
Evaluarea IRM multiparametrică este un instrument de nepreţuit în depistarea, localizarea şi caracterizarea leziunilor de prostată, una dintre cele mai provocatoare situaţii fiind cea în care cancerul de prostată poate apărea în zona tranziţională la un pacient cu hiperplazie benignă de prostată. Sistemul de scoruri PI-RADS versiunea 2.1 reuşeşte să standardizeze rapoartele radiologice, să faciliteze localizarea precisă a leziunii şi să ajute la selecţia pacienţilor pentru biopsia ghidată.
Introduction
Benign prostatic hyperplasia (BPH) is a histologic diagnosis characterized by proliferation of the prostatic cellular elements. It is one of the most common diseases in ageing men, with a prevalence of 8%, 50% and 80% in the 4th, 6th and 9th decades of life, respectively(1).
Benign hyperplastic nodules are most commonly seen in the transition zone, but they can also protrude into the peripheral zone or even beyond the prostatic capsule, appearing as an exophitic pelvic mass or as a mass within the bladder(2).
BPH is a progressive disease, being the most common cause of lower urinary tract symptoms (LUTS)(3). Usually, there is a direct relationship between prostate enlargement and symptoms severity, although many patients with small prostates also present urinary obstruction, because of the strategically position of the adenoma, sitting right on the bladder outlet(2).
The initial evaluation should asses the frequency and severity of symptoms by using the International Prostate Symptom Score (IPSS)(4) and it should also include a digital rectal examination and urinalysis. Enlargement of the prostate associated with a palpable nodule and elevated PSA (prostate specific antigen) level requires imaging methods of diagnosis, such as transrectal ultrasonography (which provides a more accurate assessment of prostate volume than digital rectal examination does)(5) and MRI (for the characterization of the prostatic tissue, due to its excellent contrast resolution).
The upgraded PI-RADS version 2.1 scoring system manages to standardize the MRI radiological reports and helps in patients’ selection for targeted biopsy, in order to rule out prostate cancer (PCa). In 20% of cases, BPH and PCa coexist in the same prostatic zone(6).
Case report
We present the case of a 60-year-old patient who was referred to the urology department of our clinical institute three years ago, with lower urinary tract symptoms (LUTS). PSA value was 32.27 ng/ml, significantly higher than the upper limit of normal PSA. Initial articles supported the idea that men with a slightly elevated PSA value (4-10 ng/ml) had a 22% chance of having incipient prostate cancer, while those with an important elevated PSA level (>10 ng/ml) had a 67% risk of having prostate cancer(7). Digital rectal examination and transrectal ultrasonography revealed an increased prostate. The patient was directed to our department, where we performed an MRI investigation, in order to rule out prostate cancer, possibly associated with BPH. A written consent was taken from the patient before entering the scanner room, after he was interviewed about his medical history, possible allergies, previous examinations and MRI contraindications. An intravenous antispasmodic agent is routinely used, in order to decrease the artifacts generated by intestinal motility, after a venous line is secured. He was investigated on a Toshiba 1.5T Vantage Titan MRI platform, using a multiparametric protocol, which offers both morphological and functional information. High-resolution multiplanar T2 WI are morphological sequences ideal for the prostate anatomy evaluation. Dynamic contrast enhancement (DCE) and diffusion-weighted (DWI) are functional sequences, corresponding to angiogenesis and cellular density, respectively. MR-spectroscopy (MRS) is another functional sequence that correlates with cellular turnover, but we do not perform it routinely.
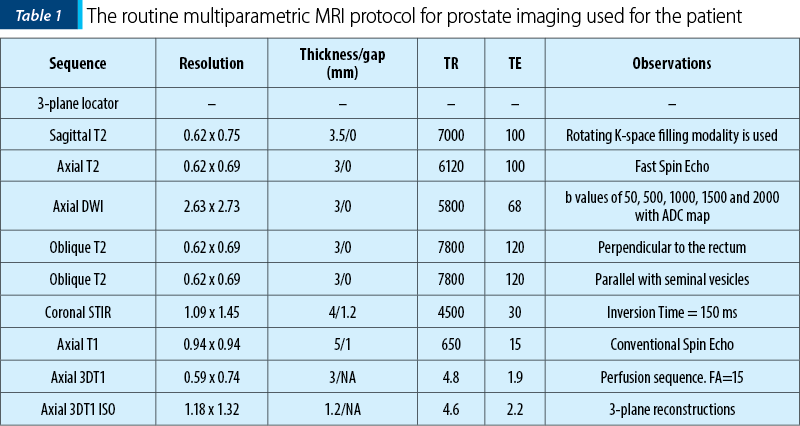
The scanning protocol is listed in Table 1. Contrast media is injected in a volume of 0.1 mL per patient body weight, and the contrast type differs depending on the availability, but usually, an extravascular agent such as Gd-DO3A-butrol or Gd-BOPTA is utilized; a flow of around 2 mL/s is considered sufficient, and a chaser of 20 mL of saline immediately follows the contrast injection.
Imaging findings showed an enlarged prostate, with its three diameters of 51 mm, 61 mm and 41 mm (longitudinal diameter, axial diameter and anteroposterior diameter, respectively), with an estimated total volume of 66.81 mL. The transitional zone (TZ) appeared asymmetrically enlarged, predominantly on the right half of the prostate, which led to the compression of the urethra (being displaced to the left) and thinning the peripheral zone (PZ), especially on the right side of the base. The PZ showed diffuse decreased signal intensity on T2WI and no restricted diffusion, typical aspect for chronic inflammatory lesions. The TZ presented multiple small cystic areas and a multinodular structure (because of the presence of stromal and glandular nodules), the biggest one being located in the right middle third and apex of the TZ, with an axial diameter of 38 mm. We noticed a bulging aspect of the macronodule described in the right TZ, protruding into the neighboring PZ, with a central area of increased signal intensity on diffusion WI and decreased signal intensity on ADC map, but a negative dynamic contrast enhancing (DCE) curve (Figures 1 and 2).
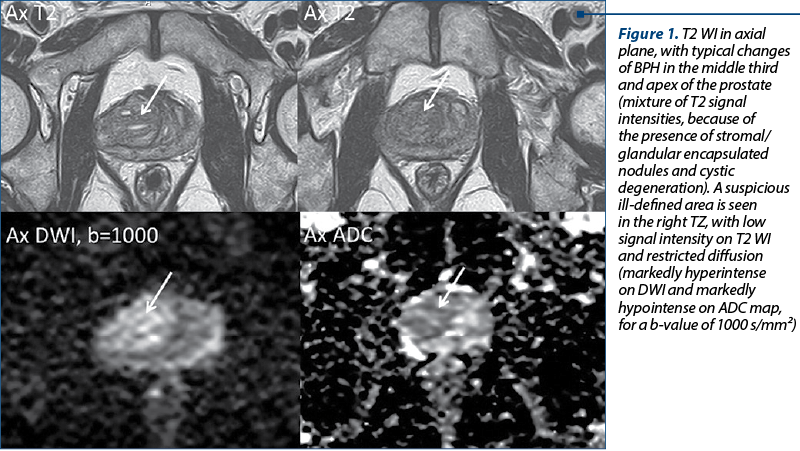
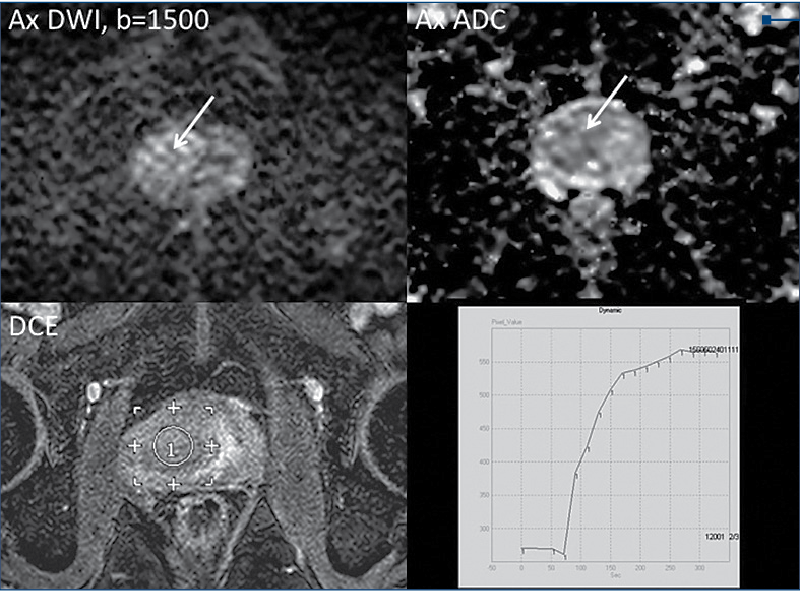
PI-RADS assessment uses a 5-point scale based on the likelihood that a combination of MP MRI findings on T2, DWI and DCE correlates with the presence of a clinically significant cancer(8). T2 WI is the primary determining sequence for assigning the PI-RADS category in TZ(8). This particular right TZ nodule has been marked with a final PI-RADS score of 3, which means that the presence of clinically significant cancer is equivocal. Considering the elevated PSA and the PI-RADS score of 3, the next step in patient management was the targeted biopsy.
Discussion
BPH nodules appear as a mixture of signal intensities, ranging from hypointense to hyperintense on T2 WI, depending on the proportion of their stromal and glandular components. They are well-delineated nodules that arise in the TZ, involving the periurethral regions, but sometimes they can bulge the surgical capsule, so they can be found in the PZ.
The reported macronodule of BPH, located in the right middle third and apex of the TZ, appears mostly encapsulated and heterogeneous, with ill-defined, homogeneous, mildly hypointense included areas on T2 WI, so it was marked with a T2 PI-RADS score of 2. Diffusion plays a major role in changing the assessment of a TZ lesion scored with 2 on T2 WI, if the DWI score for the same area is at least 4. This means that the radiologist should identify that area as being markedly hyperintense on DWI, markedly hypointense on ADC map on a high b-value and measuring <1.5 cm (scored 4 on DWI), or being markedly hyperintense on DWI, markedly hypointense on ADC map on a high b-value and measuring ≥1.5 cm or being invasive (scored 5 on DWI). Since our reported lesion demonstrates restricted diffusion (increased signal intensity on DWI and decreased signal intensity on ADC map, for a b-value of 1000, but also for 1500 s/mm²) and measures at least 20 mm, it was marked with a DWI PI-RADS score of 5. DCE has no value in the PI-RADS v2.1 classification of lesions in the TZ. Following all these decisions regarding T2 and DWI aspect of the lesion, the final PI-RADS score for the lesion was PI-RADS 3 (meaning that the presence of clinically significant cancer is equivocal).
The patient was referred for prostatic biopsy one month after the MR examination, considering the elevated PSA value, which revealed a benign appearance of the sample: polymorphic aspect on account of a chronic inflammatory, non-specific process.
Retrospectively, we can conclude that DWI changes and elevated PSA value may be due to this chronic inflammatory, non-specific process. The patient received anti-inflammatory treatment and remained under urological surveillance.
Conclusions
Multiparametric MRI is a precious tool in prostate tissue characterization, completing clinical and biological information, but in case of BPH, a suspected prostate carcinoma in the TZ may represent a real challenge for the radiologist. Often, biopsy is mandatory for a definitive differentiation between inflammatory lesions and prostate cancer. n
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- Lim KB. Epidemiology of clinical benign prostatic hyperplasia. Asian J Urol. 2017 Jul; 4(3): 148-151.
- Foo KT. Diagnosis and treatment of benign prostate hyperplasia in Asia. Transl Androl Urol. 2015 Aug; 4(4):478-483.
- Emberton M, et al. Benign prostatic hyperplasia as a progressive disease: a guide to the risk factors and options for medical management. Int J Clin Pract. 2008 Jul; 62(7): 1076-1086.
- Liao CH, et al. Diagnostic value of International Prostate Symptom Score voiding-to-storage subscore ratio in male lower urinary tract symptoms. Int J Clin Pract. 2011; 65(5): 552-558.
- Edwards JL. Diagnosis and management of Benign Prostatic Hyperplasia. Am Fam Physician. 2008 May; 77(10): 1403-1410.
- Miah S, Catto J. BPH and prostate cancer risk. Indian J Urol. 2014 Apr-June; 30(2): 214-218.
- Jones JS, et al. Four no more: The “PSA cutoff era” is over. Cleveland Clinic Journal of Medicine. 2008, Jan; 75(1): 30-32.
- American College of Radiology. Revisions in PIRADS v2.
- Jordan EJ, et al. PI-RADS V2 and ADC values: is there room for improvement?. Abdom Radiol (NY). 2018; 43(11): 3109-3116.
- Xi Y, et al. Low-to-high b value DWI ratio approaches in multiparametric MRI of the prostate: feasibility, optimal combination of b values and comparison with ADC maps for the visual presentation of prostate cancer. Quant Imaging Med Surg. 2018; 8(6): 557-567.
- Alcaraz A, et al. Is there evidence of a relationship between benign prostatic hyperplasia and prostate cancer? Findings of a literature review. Eur Urol. 2009; 55(4):864-73.
Articole din ediţiile anterioare
Managementul cancerului de prostată rezistent la castrare
Cancerul de prostată rezistent la castrare (CRPC) este un aspect important al practicii noastre clinice în fiecare zi. Pentru o perioadă foarte lun...
Imagistica multiparametrică de rezonanţă magnetică în diagnosticul cancerului de prostată: o necesitate
Cancerul de prostată reprezintă o importantă problemă de sănătate publică. Imagistica prin rezonanţă magnetică (IRM) este cea mai bună modalitate d...
Aspecte IRM ale leziunilor PI-RADS 5 – experienţa unui centru terţiar
Cancerul de prostată este una dintre cele mai frecvente afecţiuni maligne în rândul bărbaţilor, pentru care se depun eforturi sporite, cu scop...