Introduction. The study aimed to identify complications, risk factors and maternal and fetal follow-up associated with gestational diabetes.
Materials and method. We analyzed 80 patients diagnosed with gestational diabetes, compared to 20 patients who did not have this pathology, all of them being hospitalized at the “Bucur” Maternity, Bucharest.
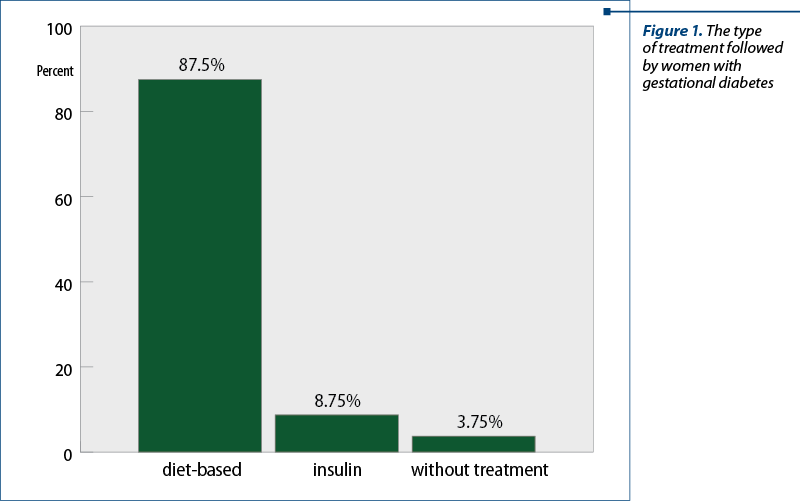
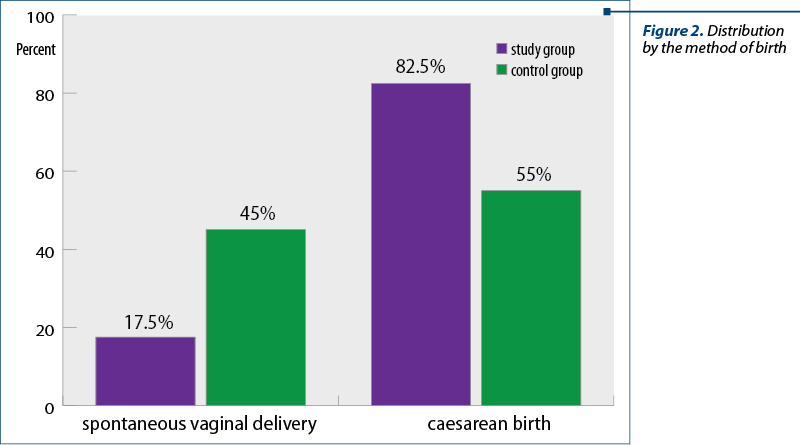
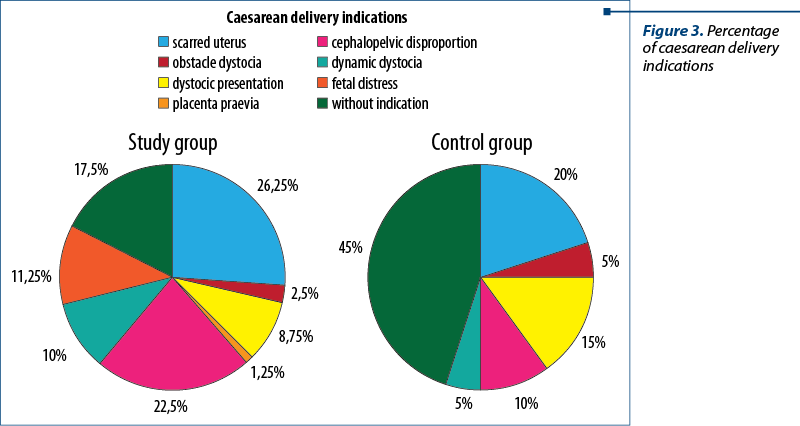
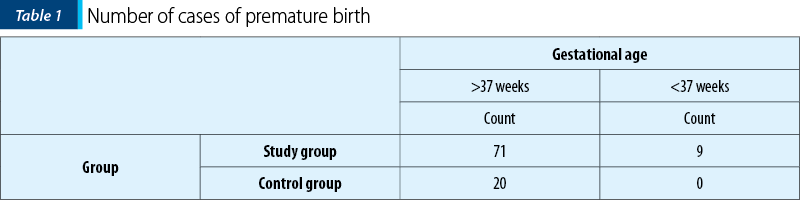
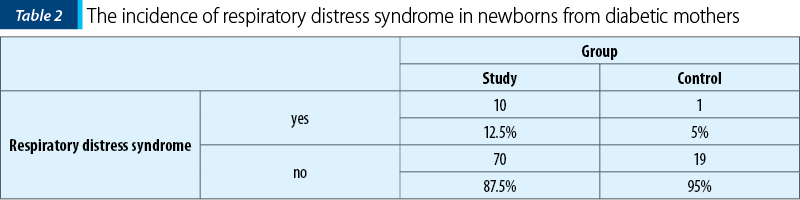
Results. The most frequently used treatment (in 87.5% of cases) to control gestational diabetes was diet-based. The majority (82.5%) of pregnant women with gestational diabetes gave birth by caesarean section, the most frequent indication being caesarean scar (26.25%). The incidence of premature births in the diabetic group was 11.25%. With a higher incidence compared to patients without gestational diabetes, iron deficiency anemia (77.5%) and arterial hypertension (27.5%) were also observed. Neonatal respiratory distress had an incidence of 12.5%.
Conclusions. According to this study, women with gestational diabetes and their newborns have clinical complications during pregnancy. Early diagnosis can prevent and alleviate the possible complications.
Particularităţi ale evoluţiei materno-fetale la pacientele cu diabet gestaţional
Maternal and fetal characteristics in pregnancies complicated with gestational diabetes
First published: 24 martie 2022
Editorial Group: MEDICHUB MEDIA
DOI: 10.26416/Gine.35.1.2022.6131
Abstract
Rezumat
Introducere. Studiul elaborat a avut ca obiectiv identificarea complicaţiilor, a factorilor de risc şi a altor particularităţi asociate diabetului gestaţional.
Materiale şi metodă. Am analizat 80 de paciente diagnosticate cu diabet gestaţional, comparându-le cu 20 de paciente care nu au prezentat această patologie, toate fiind internate la Maternitatea „Bucur”, Bucureşti.
Rezultate. Tratamentul cel mai des folosit (în 87,5% din cazuri) pentru a controla diabetul gestaţional a fost cel bazat pe regim. Majoritatea (82,5%) gravidelor cu diabet gestaţional au născut prin cezariană, indicaţia principală fiind uterul cicatricial (26,25%). Incidenţa naşterilor premature în grupul cu diabet a fost de 11,25%. Cu o incidenţă mai mare comparativ cu a pacientelor fără diabet gestaţional, au fost observate şi anemia feriprivă (77,5%), hipertensiunea arterială (27,5%) şi detresa respiratorie neonatală (12,5%) la copiii acestora.
Concluzii. Conform acestui studiului, pacientele cu diabet gestaţional şi copiii lor prezintă complicaţii clinice pe parcursul sarcinii. Diagnosticarea la timp poate preveni şi ameliora posibilele complicaţii.
Introduction
Diabetes mellitus is defined as a group of metabolic disorders, including hyperglycemia secondary to hypoinsulinemia and/or insulin resistance. Insulin deficiency may be genetic or acquired(1). Chronic hyperglycemia has multiple long-term complications, with injury and dysfunction of several organs. The most commonly affected organs are the heart, kidneys, eyes, nerves and blood vessels(1).
The prevalence of diabetes in Europe is currently 4%, but the incidence of obesity is rising alarmingly, thus the World Health Organization predicted a 35% increase in the prevalence of diabetes between 1995 and 2025(2). The diagnosis of gestational diabetes in a patient without a history of diabetes is made in the second or third trimester of pregnancy.
Gestational diabetes was first described in Germany in 1824 by Bennewitz, who observed in a woman that she had glycosuria and polydipsia for three pregnancies in a row. The birth weight of one of the three newborns was 5.5 kilograms(3). The risk factors are multiple, genetic or acquired. There is a clear association between diabetes and obesity, but also between gestational diabetes (GDM) and the mother’s advanced age, short stature, multiparity, sedentary lifestyle, excessive consumption of saturated fatty acids, vitamin D deficiency, chronic hypertension, early menarche, family history of diabetes, personal history of miscarriages, stillbirths and fetuses born with macrosomia. The main objective of the current study was to analyze the risk factors and their impact on maternal and fetal evolution at the level of organ and organ system.
Materials and method
We performed a retrospective, descriptive study over a period of 17 months (between February 2020 and June 2021), which included 80 pregnant women with gestational diabetes (study group) and 20 pregnant women without diabetes (control group). All 100 pregnant women gave birth at the Bucur Maternity, “Sf. Ioan” Emergency Clinical Hospital, Bucharest.
The data used were collected from: patient’s observation papers, birth and operation records, and from the Hippocrates medical computer system. Initially we analyzed the patients referring to the dispensation of pregnancies and the modality of birth. We also mentioned the type of treatment followed by pregnant women with GDM.
We referred to the peri- and postnatal period by analyzing the following factors: caesarean section indication, Apgar index, baby’s weight at birth and gestational age at birth. The quantification of the risk factors and the maternal and fetal complications within the two study groups were points of interest in the statistical analysis. The data processing was performed with the program SPSS (Statistical Package for the Social Sciences) 23.0. The results were interpreted by analyzing graphs and tables.
Results
Regarding the type of treatment followed by women with gestational diabetes, 87.5% of them had received a diet-based treatment, 8.75% had required insulin, and 3.75% of these did not follow a treatment due to late diagnosis (confirmation was made after birth).
A considerable difference within the two groups in terms of pregnancy dispensation was found. Only 70% of women from the control group had the pregnancy investigated, while in the study group the percentage was 96.25%.
There are significant differences between the two groups in terms of birth: 82.5% of women with gestational diabetes gave birth by caesarean section, while 55% of pregnant women without diabetes gave birth in this way.
Previous caesarean section was more common in patients with diabetes (26.25%) than in those without diabetes (20%). The most common indication for caesarean section in the control group was the dystocic presentation (in 15% of cases), while this indication was classified as the main one in only 8.75% of cases in patients with gestational diabetes. Furthermore, cephalopelvic disproportion and dynamic dystocia were considered the main indication for caesarean section in 22.5% of cases and in 10% of cases among pregnant women with gestational diabetes, and about 10% and 5% of cases in pregnant women without gestational diabetes. A percentage of 11.25% from the indications of caesarean section was the fetal distress in patients with gestational diabetes. This indication was not detected in the control group.
In the study group, there were nine patients with diabetes who gave birth prematurely. All women from the control group gave birth at term. Thus, the incidence of premature births in the diabetic group was 11.25%.
The incidence of gestational hypertension was higher in patients with gestational diabetes (27.5%) than in those without diabetes (15%) and was correlated with the risk of giving birth prematurely (p<0.05). During pregnancy, anemia caused by iron deficiency occurred in 77.5% of pregnant women with gestational diabetes and in 55% of those without gestational diabetes. The p value was below 0.05.
It was observed that there were multiple neonatal complications in newborns from diabetic mothers: in 3.75% of cases hypoglycemia was reported, in 1.25% of cases enterocolitis was identified and, also, with an incidence of 1.25%, pneumonia was observed.
The incidence of neonatal respiratory distress was 12.5% in newborns of mothers with diabetes, respectively 5% in newborns of women who did not have the disease. Also, the incidence of respiratory distress was 33.33% in premature babies and only 8.791% in those born after 37 weeks of gestation. Furthermore, this syndrome was corelated with a higher chance for a low Apgar score.
Discussion
According to the results obtained from the comparison of the study and control groups, the need for caesarean section was higher in diabetic women. Moreover, we mention the presence of the caesarean scar as the main factor in choosing caesarean birth, this feature further strengthening the previously reported premise in light of the fact that they had a history of caesarean births through another possible episode of gestational diabetes. These conclusions are closely in line with the results published by Brody and Harris(4). Fetal distress is another important factor to report as an indication for a caesarean section. Such cases were found in this study only in pregnant women with GDM.
As for the oral glucose tolerance test (OGTT screening), it was performed in a higher percentage in the general population at the time of the study, compared to the prevalence of this screening in Europe, from the data published in 2005(5). This difference can be viewed with optimism, the importance of the OGTT screening being more obvious now.
Similar to the scientific findings published by Rajput et al., the analysis of risk factors associated with gestational diabetes(6) confirmed the higher incidence of gestational hypertension in these patients. Moreover, according to ACOG(7) and to our results, high blood pressure increases the risk of premature birth. It was found in the study group that more than half of premature births corresponded to a hypertensive status in pregnant women.
Following the cases of premature births in these two groups, the hypothesis stated and proven in other scientific reports(8,9) was confirmed once again, the risk of premature birth being higher when gestational diabetes was part of the pathology present in pregnant women. As it has been shown, it is obvious that with the premature birth many other complications are involved.
According to the literature, a higher incidence of cephalopelvic dystocia has been reported in diabetic pregnant women(10). The incidence of macrosomia was equal in both groups of pregnant women in this study. However, the characteristics of the pelvis must be considered with equal importance; in the study group, there are cases of fetuses with normal size, but their mothers had a distocyc pelvis.
The newborn’s risk of respiratory distress may be mentioned as higher in the case of the concomitant presence of gestational diabetes, the results being similar to those obtained by a cohort study in France(11). Furthermore, it was observed that premature babies, compared to those born at term, were more predisposed to have this syndrome.
Although iron deficiency anemia is common in pregnant women, it should not be overlooked. According to the results obtained in this study, but also from other studies(12), women with gestational diabetes have a higher incidence of anemia.
Conclusions
According to the study presented, pregnant women with gestational diabetes required caesarean section more frequently than non-diabetics. Arterial hypertension is common in pregnant women with gestational diabetes. The risk of fetal distress is also higher in newborns from diabetic mothers. Data from our study indicated that gestational diabetes increases the risk of preterm birth. Diet-based treatment is most commonly used to control blood sugar levels. Gestational diabetes increases the risk of neonatal respiratory distress. The incidence of iron deficiency anemia is significantly higher in pregnant women with gestational diabetes than in pregnant women in the control group.
Conflict of interests: The authors declare no conflict of interests.
Bibliografie
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2011;34(Suppl 1):S62-S69.
- Chen Y, Quick WW, Yang W, Zhang Y, Baldwin A, Moran J, et al. Cost of gestational diabetes mellitus in the United States in 2007. Popul Health Manag. 2009;12(3):165–74.
- Mestman JH. Historical notes on diabetes in pregnancy. Endocrinologist. 2002;12:224-42.
- Brody SC, Harris R LK. Screening for gestational diabetes: a summary of the evidence for the U.S. Preventive Services Task Force. Obstet Gynecol. 2003;101(2):380–92.
- Luke C, Kemper I, Henschen S BK. Diagnosis and therapy of gestational diabetes-comparison of two surveys of established gynecologists in Berlin and Saxonia-Anhalt. Z Geburtshilfe Neonatol. 2005;209(6):219–22.
- Rajput R, Yadav Y, Nanda S. Prevalence of gestational diabetes mellitus & associated risk factors at a tertiary care hospital in Haryana. Indian J Med Res. 2013;137(4):728-33.
- Premkumar A, Baer JR, Jelliffe-Pawlowski LL, Norton ME. The effect of hypertensive disorders in pregnancy on preterm birth rates among African-American women. Obstet Gynecol. 2017;129(5):122S-123S.
- Köck K, Köck F, Klein K, Bancher-Todesca D, Helmer H. Diabetes mellitus and the risk of preterm birth with regard to the risk of spontaneous preterm birth.
- J Matern Fetal Neonatal Med. 2010;23(9):1004-8.
- Yogev Y. Spontaneous preterm delivery and gestational diabetes: the impact of glycemic control. Arch Gynecol Obstet. 2007;276(4):361–5.
- Gabbe SG, Niebyl JR, Simpson JL. Diabetes mellitus complicating pregnancy. In: Obstetrics, normal and problem pregnancies. 5th ed. Philadelphia: Churchill Livingstone. 2007:976–1005.
- Mitanchez D. Foetal and neonatal complications in gestational diabetes: perinatal mortality, congenital malformations, macrosomia, shoulder dystocia, birth injuries, neonatal complications. Diabetes Metab. 2010;36(6 Pt 2):617–27.
- Lao TT. Anaemia in pregnancy: is the current definition meaningful? Eur J Obstet Gynecol Reprod Biol. 1996;68(1-2):53–8.
Articole din ediţiile anterioare
Creşterea riscului de detresă respiratorie consecutivă operaţiei cezariene
Incidenţa operaţiei cezariene prezintă o tendinţă de creştere la nivel global, depăşind cu mult nivelul optim de 15% recomandat de Organizaţia Mond...
Postpartum hemorrhage – a major obstetrical emergency. Causes and treatment
Hemoragia post-partum (HPP) este o problemă semnificativă de sănătate maternă, reprezentând o cauză majoră de mortalitate obstetricală la nivel g...
Provocările terapeutice ale sindromului de detresă respiratorie a nou-născutului – prezentare de caz
Insuficienţa respiratorie este frecvent observată la nou-născuţii cu asfixie perinatală severă. Aceasta reprezintă rezultatul afecţiunilor sub...
Rolul sarcinii şi al naşterii în apariţia tulburărilor de statică pelvică
Introducere. Multiple studii subliniază consecinţele naşterii vaginale asupra planşeului pelvic, însă sarcina în sine reprezintă un factor de risc ...